
Patients with ankylosing spondylitis suffering from AO Type B3 traumatic thoracolumbar fractures are associated with increased frailty and morbidity when compared with patients with diffuse idiopathic skeletal hyperostosis
Introduction
Formal fracture classification systems enable systematic research and aid in surgical decision-making. The AO Spine thoracolumbar injury spine injury classification system is the most up to date, comprehensive and popular classification system used at present. The AO Type B3 fracture subclass is defined as a hyperextension injury with disruption of the anterior tension band with an intact posterior element hinge preventing gross translation (1). This is an unstable injury where surgical management is recommended.
Ankylosing spondylitis (AS) is a seronegative spondyloarthropathy diagnosed usually before 30 years of age and is associated with the HLA-B27 gene (2). Patients with AS suffer from ossification of spinal ligaments, discs, endplates and apophyseal structures giving the vertebral column the classic “bamboo spine” appearance. Kyphotic deformity, ankylosis of the craniocervical junction are present in AS (3). On the other hand, diffuse idiopathic skeletal hyperostosis (DISH) is usually diagnosed in the older age group in patients who are predisposed to the metabolic syndrome. It usually involves the thoracic and lumbar spine, with ossification predominantly in the spinal anterior longitudinal ligament. As opposed to AS, patients with DISH do not have disease involvement in the sacroiliac joint, apophyseal joints, and craniocervical joints (4). Due to the ankylosed spine in AS and DISH, long-segment fixation is usually required to restore spinal vertebral stability.
Not all AO Type B3 fractures are associated with ankylosing spinal disorders, and the converse is also true. However, there is a large overlap between AO Type B3 fractures and AS-DISH patients with up to 71.4% to 93.7% of patients with ankylosing spinal disorders sustaining an AO Type B3 fracture post spinal injury (5).
In this study, the authors examine the clinical profile of surgically-managed AO Type B3 traumatic thoracolumbar fractures in patients with AS or DISH. We also compare the pre-morbid and clinical factors between patients with AS and DISH in the setting of AO Type B3 fractures.
Methods
The registry of a state spinal trauma service was queried between January 2008 and December 2018 for consecutive patients who met the following inclusion criteria: (I) adult patient ≥18 years old, (II) AO Type B3 traumatic thoracolumbar fracture from T9–L2 and (III) received operative treatment. Fracture classification was determined from preoperative computed tomography with magnetic resonance imaging as required and verified by two authors (T Tan, J Tee). Operative treatment had to be undertaken within the index admission and not in a delayed fashion. We excluded patients with pathological fractures secondary to malignancy. This study was approved by the institutional review board (reference 219/19, study outcomes not affecting future management, no informed consent required, patient personal data anonymized) and was undertaken in accordance with the Helsinki Declaration 2013.
An electronic spreadsheet (Microsoft Excel, Redmond, WA, USA) was formulated a-priori to capture study variables. Patient demographics [age, gender, body mass index (BMI)], baseline co-morbid condition [presence of AS, presence of DISH, American Society of Anesthesiologists (ASA), Charlson-comorbidity index, modified frailty index (mFI) (6)], injury characteristics [level of injury, mechanism of injury, pre- and post-operative American Spinal Injury Association (ASIA) grade], surgical variables (number of levels fixated), radiographical variables (pre and postoperative Cobb angle, Gardner angle, sagittal index), postoperative outcomes (mortality, length of stay, complication profile) was recorded. Frailty was defined as an mFI of more than or equal to 0.36 (4 of 11 factors). Radiographical measures were calculated using mid-sagittal plain radiographs or computed tomography scans using methods as summarized by Keynan et al. (7). The change in Cobb angle postoperatively was calculated and defined as follows: ΔCobb angle = Cobb angle(postoperative) – Cobb angle(preoperative). The change in Cobb angle was calculated in the immediate postoperative period (within 2 postoperative days), and also at the point of final follow-up. Similar indices were calculated for the change in Gardner angle, and change in sagittal index. Loss of Cobb angle correction was calculated and is defined as: loss of correction [Cobb angle] = Cobb angle(final follow-up) – Cobb angle(immediate postoperative). Similar indices were calculated for Gardner angle and sagittal index. Overall morbidity rate was defined by the presence of any (at least one) complication during the follow-up period.
Statistical analysis
Results are presented in two forms: (I) as a single cohort of all included patients, and (II) as a comparative analysis between patients with AS versus patients with DISH. Summary statistics and frequency distributions are presented in the form of proportions, means, medians, and standard deviations. Univariate analysis was undertaken using contingency tables (Fisher’s exact test), student t-test and Mann-Whitney U test for categorical variables, parametric data, and ordinal non-parametric data respectively to compare AS and DISH groups (SPSS Inc., Chicago, IL, USA). Odds ratio were calculated where appropriate with 95% confidence intervals (CIs). All tests were two-tailed with significance of P values set at 0.05 or less.
Results
Single cohort analysis
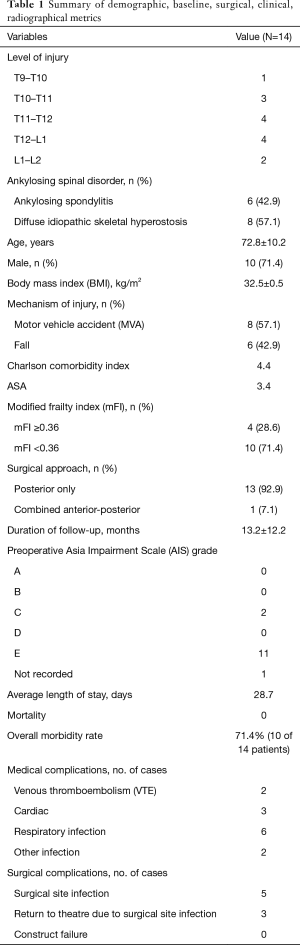
A total of 14 patients were included. The average age was 72.8±10.2 years, with 71.4% (n=10) of patients being male and an average BMI of 32.5±0.5 kg/m2. In our cohort, all patients with AO Type B3 fractures had either AS or DISH, with 6 patients having AS and the remaining 8 patients having DISH. None of the patients had a pre-injury diagnosis of AS or DISH. The average Charlson-comorbidity index was 4.4 (median: 4). Twenty-eight point six percent (n=4) of patients were frail with an mFI of ≥0.36.
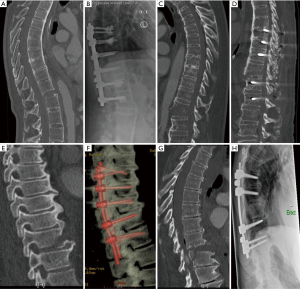
Motor vehicular accidents accounted for 57.1% (n=8) of injuries. The most common level of injury was T11–12 (n=4), and T12–L1 (n=4). Seventy-eight point six percent (n=11) of patients were neurologically intact (ASIA E) preoperatively. Ninety-two point nine percent (n=13) of patients underwent surgery via a posterior-only approach, with the remaining 1 patient undergoing a combined anterior-posterior approach. The average length of stay was 28.7 days and duration of follow-up was 13.2±12.2 months. Figure 1 illustrates preoperative and postoperative imaging appearances of patients with AS and DISH.
There were zero cases of perioperative mortality within 30 days of surgery. The overall morbidity rate was 71.4% (n=10 patients had at least one morbidity). The most common medical complication was secondary to a respiratory cause, followed by cardiac causes. The overall rate of surgical site infection was 35.7% (n=5), all of which were superficial surgical site infections. There were zero cases of construct failure which required revision/supplemental surgery during the follow-up period.
Table 1 summarizes the demographical, baseline, surgical and clinical variables of the entire cohort.
Full table
Comparative analysis
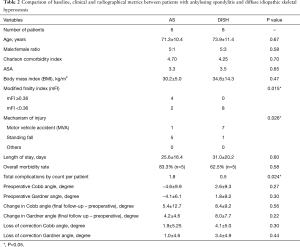
There were 6 patients with AS and 8 patients with DISH. There were no statistically significant between-group differences in terms of age, gender, BMI, ASA and Charlson-comorbidity index. Patients with AS were significantly more likely than DISH patients to be frail [mFI ≥0.36] [odds ratio (OR): 30.6, 95% CI: 1.2 to 784.7, P=0.015]. There were no differences between the spinal level of injury, or the degree of spinal cord injury (as measured by ASIA grading) between groups. The mechanism of injury was significantly more likely to be secondary to a low fall in patients with AS than DISH (OR: 35.0, 95% CI: 1.7 to 703.0, P=0.026).
Radiographical variables were statistically similar between groups. Specifically, preoperative Cobb angle, Gardner angle and sagittal index were similar. At final follow-up, the degree of change (i.e., correction) of sagittal radiographical parameters (Cobb angle, Gardner angle, sagittal index) were similar between patients with AS and DISH. Further, there were no differences in the degree of loss of sagittal correction between patients with AS and DISH.
There was a trend towards an increased overall morbidity rate in patients with AS versus DISH (83.3% vs. 62.5%) respectively. There was a statistically significant increase in the absolute number of complications per patient in the AS group (AS: 1.8 complications/patient vs. DISH: 0.5 complications/patient, P=0.024).
Table 2 summarizes the demographical, baseline, surgical, radiographical and clinical variables of the AS and DISH groups.
Full table
Discussion
This is a study specifically on AO Type B3 traumatic thoracolumbar fractures in patients with AS and DISH who were surgically managed. In our cohort, there were no patients without an ankylosing spinal disorder. We did not include patients with other fracture morphologies, e.g., AO Type C translational displacement fractures in our attempt to reduce the study bias.
In the current study, the proportion of patients without spinal cord/conus/cauda equina injury (i.e., ASIA A-D) is 21.4%. This is consistent with the rate of spinal cord injury in studies of patients with AS and DISH, with reported rates of 13.0–23.0% in the thoracolumbar spine (8). It should be noted that the rate of spinal cord injury in our study would be even higher if we included patients with ankylosing spinal disorders and AO Type C fractures (outside the scope of this study). The high rate of neurological deficit, coupled with the inherent unstable fracture morphology, renders surgical management the recommended option in patients who are fit for surgery (8).
It is well-known that in spinal fractures, patients with ankylosing spinal disorders have a higher rate of in-hospital mortality and morbidity compared to the general population (9). However, it is not definitively known if there is a difference between patients with AS and DISH with regards to mortality and morbidity. A study by Westerveld et al. (5) reported mortality rates of 6.4% and 7.3% of surgically-treated AS and DISH patients respectively. The current study demonstrates that in patients with AO Type B3 fractures, patients with AS are objectively frailer than patients with DISH, as denoted by an mFI of ≥0.36. An increased mFI is indicative of frailty and predicts increased mortality and morbidity (10). This has been shown in large-scale registry studies (6), and also in spine surgery (11) and trauma (10). In our study, patients with AS were designated as “frail” despite similarities in the age, gender, ASA and Charlson-comorbidity index between the AS and DISH groups. This reinforces the sensitivity of the mFI as a clinical tool to assist in risk stratification and complication reduction. The global ageing population, especially in developed countries, and the concomitant increase in burden of chronic illnesses, further compounds the risk profile for patients with AS or DISH sustaining spinal fractures.
Within the elderly population, low falls or falls from standing height account for 4.4% of injury-related deaths (12). In our study, we found that patients with AS had a significantly increased probability to have sustained their fracture secondary to a low fall as compared to patients with DISH. One possible explanation for this is the presence of fixed kyphotic deformity seen in patients with AS (3) that is not usually seen in DISH. Intuitively, this could be because the bone density in a patient with DISH is generally thought to be higher than that of a patient with AS. This finding has significant implications in primary prevention and should be further investigated. Another key point is that late diagnosis of spinal fractures is a frequent occurrence in ankylosing spinal disorders. As such, clinicians should maintain a high index of suspicion for spinal fractures, particularly in patients with AS, even if the underlying mechanism is innocuous.
Regarding radiographical parameters, we found no difference in preoperative Cobb angle, Gardner angle and sagittal index. This demonstrates the similarity in sagittal malalignment between AS and DISH patients. Further, with an average 4.7 (AS) and 4.9 (DISH) spinal levels of pedicle screw fixation, there was no difference during follow up in terms of the change of radiographic parameters, nor was there any differences in loss of sagittal correction between patients with AS or DISH. This demonstrates that post-traumatic kyphosis is not more likely to occur after an AO Type B3 fracture in AS than DISH in the postoperative setting.
In our study, there was a trend of an increased rate of overall morbidity in the AS group. Additionally, there was a statistically significant increase in the absolute number of complications per patient in the AS group. This is consistent with the increased frailty in the AS group in our study. One of the few studies comparing morbidity in AS and DISH patients reported equivalent morbidity rates of 87.5% and 85.7% for AS and DISH respectively (9). One potential reason for this discrepancy might be the older (72 vs. 69 years) and higher co-morbidity load (mean Charlson-comorbidity index: 4.4 vs. 1.15) in our study.
Limitations
There are several limitations to this study. The small sample size of this study affects the statistical rigor of the comparative results. Regarding neurological status, this study provides an accurate representation of patients with AO Type B3 fractures, but not of ankylosing spinal disorders as the presence of such a disorder was not part of the inclusion criteria. Inclusion of all thoracolumbar fracture types sustained by patient with ankylosing spine disorders could have increased the documented rate of spinal cord injury. As we have not included patients who underwent conservative management in our study, the overall morbidity rate in AO Type B3 patients is likely underestimated. This is because the reason patients undergo conservative management is usually that they are too unwell for surgical management.
Conclusions
In the setting of AO Type B3 fractures, patients with AS are more frail and have higher in-hospital morbidity compared to patients with DISH. Despite both pathologies being ankylosing in nature, further studies are required to fully understand the clinical differences between the two entities so as to enable clinicians to apply a more targeted and nuanced approach in managing fractures in ankylosing spinal disorders.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the institutional review board (reference 219/19, study outcomes not affecting future management, no informed consent required, patient personal data anonymized) and was undertaken in accordance with the Helsinki Declaration 2013.
References
- Vaccaro AR, Oner C, Kepler CK, et al. AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976) 2013;38:2028-37. [Crossref] [PubMed]
- Dakwar E, Reddy J, Vale FL, et al. A review of the pathogenesis of ankylosing spondylitis. Neurosurg Focus 2008;24:E2. [Crossref] [PubMed]
- Mundwiler ML, Siddique K, Dym JM, et al. Complications of the spine in ankylosing spondylitis with a focus on deformity correction. Neurosurg Focus 2008;24:E6. [Crossref] [PubMed]
- Mader R, Verlaan JJ, Eshed I, et al. Diffuse idiopathic skeletal hyperostosis (DISH): where we are now and where to go next. RMD Open 2017;3:e000472. [Crossref] [PubMed]
- Westerveld LA, Verlaan JJ, Oner FC. Spinal fractures in patients with ankylosing spinal disorders: a systematic review of the literature on treatment, neurological status and complications. Eur Spine J 2009;18:145-56. [Crossref] [PubMed]
- Farhat JS, Velanovich V, Falvo AJ, et al. Are the frail destined to fail? Frailty index as predictor of surgical morbidity and mortality in the elderly. J Trauma Acute Care Surg 2012;72:1526-30; discussion 1530-1. [Crossref] [PubMed]
- Keynan O, Fisher CG, Vaccaro A, et al. Radiographic measurement parameters in thoracolumbar fractures: a systematic review and consensus statement of the spine trauma study group. Spine 2006;31:E156-65. [Crossref] [PubMed]
- Lukasiewicz AM, Bohl DD, Varthi AG, et al. Spinal Fracture in Patients With Ankylosing Spondylitis: Cohort Definition, Distribution of Injuries, and Hospital Outcomes. Spine (Phila Pa 1976) 2016;41:191-6. [Crossref] [PubMed]
- Westerveld LA, van Bemmel JC, Dhert WJ, et al. Clinical outcome after traumatic spinal fractures in patients with ankylosing spinal disorders compared with control patients. Spine J 2014;14:729-40. [Crossref] [PubMed]
- Vu CCL, Runner RP, Reisman WM, et al. The frail fail: Increased mortality and post-operative complications in orthopaedic trauma patients. Injury 2017;48:2443-50. [Crossref] [PubMed]
- Ali R, Schwalb JM, Nerenz DR, et al. Use of the modified frailty index to predict 30-day morbidity and mortality from spine surgery. J Neurosurg Spine 2016;25:537-41. [Crossref] [PubMed]
- Spaniolas K, Cheng JD, Gestring ML, et al. Ground level falls are associated with significant mortality in elderly patients. J Trauma 2010;69:821-5. [Crossref] [PubMed]


