
Ambulatory spine surgery
Spinal surgery in the ambulatory setting has gained popularity with providers, patients and healthcare systems due to its efficiency and cost advantages combined with comparable clinical results. With an increasing case variety and complexity performed in this setting, it is important to understand proper patient selection and preoperative preparation to minimize complications and optimize outcomes. The shift to outpatient spinal surgery in ambulatory surgery centers (ASC) has mirrored improvements in anesthesia protocols, pain management, perioperative infections, outcomes, and patient satisfaction with the ability for patients to leave the facility the same day and recover in the comfort of their own home. In addition to the clinical benefits, the transition is fueled by system wide financial concerns of escalating costs. Healthcare cost containment strategies are intensely debated as they rise at a faster rate than the average annual income (3.9% vs. 1.8% in 2017, respectively) (1,2). The transition to outpatient or ambulatory surgical centers is a simple solution to help reduce this financial burden for both patients and payors, but only if the safety of the patient is sustained. That being said, an increase in complications or readmission rates would negate the overall benefits of outpatient ASC use. Numerous studies assess the association of postoperative complications and outcomes of various spine surgeries when performed in an outpatient setting versus an inpatient setting (3-13). The studies have discovered several preoperative considerations the surgeon must take into account in order to best select where to perform the surgery. These factors include the type of surgical procedure and invasiveness, location and extent of the procedure, various patient comorbidities, and multiple operative factors that differ between patients and surgeons.
The list of spine case types performed in an ambulatory setting has increased with advances in surgical technique, anesthesia, and postoperative care (6). Table 1 shows a list of the common spine procedures performed in the ASC setting. The procedures marked with "*" indicate more recent procedures that have started transitioning to the ASC setting. These procedures may be associated with higher risks and increased operative difficulty and should be performed by more experienced surgeons who can consistently predict surgical time and operative parameters. In 2006, anterior cervical discectomy and fusion (ACDF) comprised 17% of all outpatient spine procedures (14). Idowu et al. published a retrospective study that showed nearly 30% of single level ACDF are performed in an outpatient setting while 70% are still performed inpatient in 2014. Other common spine procedures done in ambulatory centers include microlumbar discectomy (MLD), lumbar laminectomy (35% of cases are outpatient), posterior cervical foraminotomy, cervical disc arthroplasty (CA), and the less common posterior lumbar fusions (6.9% of cases are outpatient). All of these procedures displayed an increase in proportion of outpatient versus inpatient procedures performed between 2003–2014 (15). Gray et al. observed a similar increase in popularity of outpatient lumbar procedures between 1994 and 2000 and noted that discectomy was the most common procedure comprising 70–90% of all lumbar outpatient cases (16). The shift towards outpatient spine surgery should continue as safety of these procedures is supported with research, allowing patients to decrease their length of stay in a hospital and the overall healthcare costs.
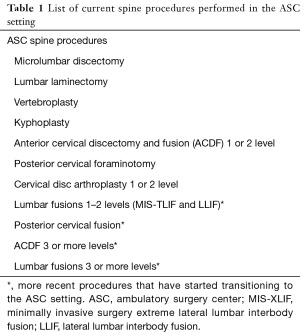
Full table
Other than case type, several other factors are considered when choosing patients for the ambulatory setting. Table 2 provides a comprehensive summary of studies evaluating preoperative characteristics and postoperative complications of inpatient and outpatient spine surgery. One and two level procedures are considered appropriate for outpatient, while greater than two level procedures are performed less frequently and usually in selected young healthy patients (3,4,6,8,10,11). A prospective study of 1–2 level ACDF performed in an outpatient setting using microsurgical techniques resulted in only two postoperative hematomas out of the 376 performed. Regarding 1–2 level lumbar decompression, seven out of 1,073 cases were complicated by postoperative hematomas including one retroperitoneal hematoma. All hematomas were detected prior to discharge within a postoperative observation period and every patient recovered without any hematoma-associated sequelae (18). A retrospective study by Mullins et al. found that 3–4 level ACDF had a higher complication rate when compared to 1–2 level ACDF, though there was no significant difference between complication rate of 3–4 level ACDF when done outpatient versus inpatient (11). Another study focusing on Medicare patients having an ACDF of 3 or more levels determined that outpatients might be associated with lower rates of readmissions, complications, and surgical charges. However, the data may be confounded by a much smaller sample size in the outpatient group and a discordance with conversion rates from outpatient to inpatient in large scale database studies (9). Even so, large database studies without clear ASC subgroups are more challenging to interpret as there is less clarity on the number of patients converted from outpatient to inpatient status after complications arise.
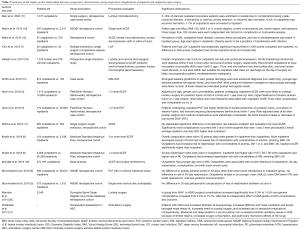
Full table
The increased acceptance of posterior lumbar fusions (PLF) in the outpatient setting correlates with significant advances in approach related morbidity reduction and improvements of pain management using a multi-modality approach. A retrospective cohort study matched outpatients and inpatients based off multiple characteristics including multi-level lumbar fusions. They found no significant difference in postoperative adverse events other than a lower blood transfusion rate in the outpatient group. The adverse events examined included wound-related infection, thromboembolic events, sepsis, pneumonia, urinary tract infection, myocardial infarction, unplanned intubation, wound dehiscence, renal insufficiency, cerebrovascular accident, death, renal failure, and being placed on a ventilator for >48 hours (6). Other studies failed to propensity match cohorts for comorbidities and as a result developed conclusions with selection bias and possible confounding factors (19). Other studies lack sufficient follow up to fully interpret the results (8-10). More extensive research is needed to verify this relationship across the multitude of spinal procedures done in an outpatient setting. However, as surgical technique continues to evolve the possibility of performing higher risk multilevel spine procedures is becoming more realistic in the outpatient setting. Therefore, surgeons are cautioned against performing spinal fusion procedures in the ASC on more than two levels when co-morbidity is present and the option for overnight stay is not available. Other than safety concerns, surgeons should know their own performance levels measured by typical length of stay for each surgery type. They should have a relatively reproducible level of pain control, patient mobility, and discharge time on procedures shifted to ASC’s. Otherwise high transfer rates to inpatient hospital beds will damage the viability of the ASC they are using.
Increased risk of complications has a significant influence on choice of surgical setting. Patient comorbidities and factors are extremely important to consider in the context of the current literature. Martin et al. used a multivariate logistic regression analysis to evaluate 2,881 patients undergoing inpatient and outpatient single level ACDF for independent risk factors for complications within thirty days. The study recommends inpatient admission for patients over sixty-five years old, body mass index (BMI) greater than 30 kg/m2, American Society of Anesthesiologists (ASA) class of 3 or 4, current dialysis, current corticosteroid use, operative times >120 minutes, and sepsis within thirty days of surgery due to increased risk for any complication (all P value <0.05). Furthermore, any patient with a difficult airway or intubation, for example a patient with Mallampati score of 4, should be considered for inpatient admission because of the increased risk of airway compromise. This is especially important to consider for ACDF cases where there is close proximity between the airway and anticipated postoperative swelling. After propensity score matching for all of these independent risk factors, there was no significant difference in complication rate between inpatient and outpatient, and there was an increased rate of reoperation in the inpatient group (10). Khalid et al. performed two similar studies on outpatient ACDF (a 1–2 level study and a multilevel 3 or more study) which revealed that anemia, diabetes mellitus (DM), and BMI >30 kg/m2 had increased risk of 30-day readmission due to complications (8,9). These risk factors are analogous to the risk factors found in a study by Smith et al., which reviewed patient outcomes in outpatient lateral lumbar interbody fusion (XLIF) and minimally invasive posterior lumbar fusions (MIS-PLF) to determine predictors of early postoperative discharge. The strongest baseline predictors of lower complications were a less advanced diagnosis, younger age, elevated baseline hemoglobin levels, and a lower BMI. The strongest variable predictors for lower complication rates were a fewer number of levels treated and elevated postoperative hemoglobin levels (12). A majority of the factors listed above are considered in the ASA classification system and contribute to a higher class (20). ASA class alone could be a helpful predictor of both complications and outcomes in spine surgery. In one study comparing outcomes of ASA classes 1 through 3, surgical complications of lumbar procedures increased from 5.0% to 14.5% and general complications from 2.9% to 15.7% with age of the patient having no unique variance in outcomes (22).
The impact of ASA classification and comorbidities on outcomes has been a focus of several studies. Helseth et al. performed a prospective single-center study of 1,449 outpatient spine procedures to develop a guideline for beginner surgeons using ASA and other significant factors. They suggested thresholds for patient selection including ASA class 1 or 2, age <70 years old, and operating on only a single level for lumbar or cervical procedures. Concerning the safety of outpatient spine procedures, they caution surgeons in their early career from using outpatient status in patients with ASA class of 3 or more, noncooperative patients (e.g., cognitive impairment), moderate/severe myelopathy, cervical degenerative spinal disease requiring corpectomy, laminectomy, or posterior fusion, or lumbar degenerative spine disease requiring laminectomy or instrumented fusion (18). This data correlates complexity of the procedure performed and patient comorbidities as independent risk factors for postoperative complications.
Anesthesiologists have a unique perspective on what cases have a higher risk when performed in an outpatient setting. They focus on certain details distinct from that of the surgeon, and therefore have valuable information to contribute to outpatient case selection. The ASA classification system does not recommend which patients should be done outpatient, but rather categorizes patients based on comorbidities allowing surgeons to weigh the risks. Obstructive sleep apnea (OSA) presents an important influence on the risk of patients undergoing spine procedures, especially in the cervical spine. Even though OSA has been shown to have no relationship between unplanned admissions or life threatening events in outpatient surgery, OSA patients have a significantly greater likelihood of intraoperative issues (23). OSA increases the risk of a difficult intubation and ventilation, the need for supplemental oxygen, and the use of vasoactive medications to correct hemodynamic derangements (21,23). The risk is amplified when patients are placed in the prone position for posterior spinal procedures. There is a significant increase in potential ventilation issues in OSA patients due to their limited reserve of oxygen, increased oxygen consumption, and the effects of sedation and being prone on pulmonary mechanics (21). The surgeon has a critical responsibility in determining the safest location for the patient, but the anesthesia team may also play an important role in preoperative considerations. Additional research should be done to evaluate the relationship between OSA and complications specifically after cervical spine procedures where approach related airway inflammation would complicate OSA respiratory mechanics.
Social, psychiatric, and cognitive issues also play a significant role in facility designation. Helseth et al. reviewed the impact of uncooperative patients and those with cognitive impairment (18). Additionally, patient household proximity to the facility and an appropriate emergency room should be considered. Those patients without family support and cognitive limitations for self care would complicate outpatient discharge. Surgeons should consider home care needs and family support in the context of the anticipated postoperative activity limitations. On one end of the spectrum, homeless patients or those with poor nutrition may require additional days in the hospital, for example. Furthermore, patients with low pain tolerance or high resistance to pain medication will pose higher risks during ambulatory discharge evaluations.
Whether or not research can establish guidelines or thresholds for patient selection in the ASC setting, individual surgeon outcomes should be considered. There is tremendous variability of skill level and experience that plays a large role in selecting the facility. Reviewing average length of stay for each procedure type and number of levels should be included in the early phases of shifting patients to ASC facilities. In summary, preoperative consideration for selecting a case for outpatient spine procedures should be based on multiple distinct patient specific factors. Most researchers across the board seem to agree that an increasing age specifically >65, a BMI >30 kg/m2, ASA >2, extended operative times, quantity of levels operated on, and complexity of the instrumentation have a significant influence on whether a patient should be considered for outpatient surgery. Secondary considerations examined with less statistical strength include surgeon’s experience, current dialysis, current corticosteroid use, sepsis within thirty days, difficult airways, anemia, diabetes, smoking, OSA, and positioning of patients in the operating room. The ASA classification system attempts to combine the comorbidities and independent risk factors associated with complications in order to simplify a patient’s overall risk for surgery. Its use may end up being more influential in the future as the strength of its relationship in predicting complications and outcomes is supported further with research. Identifying these risk factors preoperatively is vital as it assists the surgeon in deciding whether or not a patient is suitable for ambulatory or outpatient spine surgery.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- American Medical Association. Trends in healthcare spending. Available online: [Accessed 15th July 2019].https://www.ama-assn.org/about/research/trends-health-care-spending
- Frazee G. 3 Charts that explain the rise in U.S. household income. Available online: [Accessed 15th July 2019].https://www.pbs.org/newshour/economy/making-sense/3-charts-that-explain-the-rise-in-u-s-household-income
- Arshi A, Park HY, Blumstein GW, et al. Outpatient Posterior Lumbar Fusion: A Population-Based Analysis of Trends and Complication Rates. Spine (Phila Pa 1976) 2018;43:1559-65. [Crossref] [PubMed]
- Arshi A, Wang C, Park HY, et al. Ambulatory anterior cervical discectomy and fusion is associated with a higher risk of revision of surgery and perioperative complications: an analysis of a large nationwide database. Spine J 2018;18:1180-7. [Crossref] [PubMed]
- Bovonratwet P, Fu MC, Tyagi V, et al. Safety of Outpatient Single-Level Cervical Total Disc Replacement. Spine (Phila Pa 1976) 2019;44:E530-8. [Crossref] [PubMed]
- Bovonratwet P, Ottesen TD, Gala RJ, et al. Outpatient elective posterior lumbar fusions appear to be safely considered for appropriately selected patients. Spine J 2018;18:1188-96. [Crossref] [PubMed]
- Chin KR, Pencle FJR, Coombs AV, et al. Lateral Lumbar Interbody Fusion in Ambulatory Surgery Centers. Spine (Phila Pa 1976) 2016;41:686-92. [Crossref] [PubMed]
- Khalid SI, Carlton A, Wu R, et al. Outpatient and Inpatient Readmission Rates of 1- and 2-Level Anterior Cervical Discectomy and Fusion Surgeries. World Neurosurgery 2019;126:1475-81. [Crossref] [PubMed]
- Khalid SI, Kelly R, Wu R, et al. A comparison of readmission and complication rates and charges of inpatient and outpatient multiple-level anterior cervical discectomy and fusion surgeries in the Medicare population. J Neurosurg Spine 2019.1-7. [Epub ahead of print]. [Crossref] [PubMed]
- Martin CT, Pugely AJ, Gao Y, et al. Thirty-Day Morbidity After Single-Level Anterior Cervical Discectomy and Fusion: Identification of Risk Factors and Emphasis on the Safety of Outpatient Procedures. J Bone Joint Surg 2014;96:1288-94. [Crossref] [PubMed]
- Mullins J, Pojskic M, Boop FA, et al. Retrospective single-surgeon study of 1123 consecutive cases of anterior cervical discectomy and fusion: a comparison of clinical outcome parameters, complication rates, and costs between outpatient and inpatient surgery groups, with a literature review. J Neurosurg Spine 2018;28:630-41. [Crossref] [PubMed]
- Smith WD, Wohns RNW, Christian G, et al. Outpatient Minimally Invasive Lumbar Interbody: Fusion Predictive Factors and Clinical Results. Spine (Phila Pa 1976) 2016;41:S106-22. [PubMed]
- Walid MS, Robinson JS 3rd, Robinson ER, et al. Comparison of outpatient and inpatient spine surgery patients with regards to obesity, comorbidities and readmission for infection. J Clin Neurosci 2010;17:1497-8. [Crossref] [PubMed]
- Best MJ, Buller LT, Eismont FJ. National Trends in Ambulatory Surgery for Intervertebral Disc Disorders and Spinal Stenosis: A 12-Year Analysis of the National Surveys of Ambulatory Surgery. Spine (Phila Pa 1976) 2015;40:1703-11. [Crossref] [PubMed]
- Idowu OA, Boyajan HH, Ramos E, et al. Trend of Spine Surgeries in the Outpatient Hospital Setting Versus Ambulatory Surgical Center. Spine (Phila Pa 1976) 2017;42:E1429-36. [Crossref] [PubMed]
- Gray DT, Deyo RA, Kreuter W, et al. Population-Based Trends in Volumes and Rates of Ambulatory Lumbar Spine Surgery. Spine (Phila Pa 1976) 2006;31:1957-63. [Crossref] [PubMed]
- Best NM, Sasso RC. Success and Safety in Outpatient Microlumbar Discectomy. J Spinal Disord Tech 2006;19:334-7. [Crossref] [PubMed]
- Helseth Ø, Lied B, Halvorsen CM, et al. Outpatient Cervical and Lumbar Spine Surgery is Feasible and Safe: A Consecutive Single Center Series of 1449 Patients. Neurosurgery 2015;76:728-37; discussion 737-8. [Crossref] [PubMed]
- Mundell BF, Gates MJ, Kerezoudis P, et al. Does patient selection account for the perceived cost savings in outpatient spine surgery? A meta-analysis of current evidence and analysis from an administrative database. J Neurosurg Spine 2018;29:687-95. [Crossref] [PubMed]
- Mannion AF, Fekete TF, Porchet F, et al. The influence of comorbidity on the risks and benefits of spine surgery for degenerative lumbar disorders. Eur Spine J 2014;23:S66-71. [Crossref] [PubMed]
- Prabhakar A, Helander E, Chopra N, et al. Preoperative Assessment for Ambulatory Surgery. Curr Pain Headache Rep 2017;21:43. [Crossref] [PubMed]
- American Society of Anesthesiologists. ASA Physical Status Classification System. Available online: [Accessed 14th August 2019].https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system
- Stierer TL, Wright C, George A, et al. Risk Assessment of Obstructie Sleep Apnea in a Population of Patients Undergoing Ambulatory Surgery. J Clin Sleep Med 2010;6:467-72. [PubMed]


