
Posterior screw fixation in the subaxial cervical spine: a technique and literature review
Introduction
Posterior cervical spine fixation is a key component in posterior cervical arthrodesis, which is commonly performed to treat various degenerative, neoplastic, inflammatory and traumatic conditions affecting the cervical spine (1,2). The cervical spine is highly mobile and is composed of seven vertebrae. The first and second cervical vertebrae, known as the atlas and axis respectively, have unique morphologies and anatomical features (1-3). The subaxial cervical spine from C3 to C7, has more similar anatomical characteristics.
Cervical vertebrae are much smaller than the thoracic and lumbar vertebrae and most cervical vertebrae can be clearly distinguished by the presence of transverse foramen which encloses the vertebral artery and vein (1). In the majority of the patients, the vertebral artery enters the transverse foramen at C6; however, some patients may have variants with the vertebral artery entering at either C5 or C7 (in less than 10% of the cases) (1). This is an important point to consider and check preoperatively when planning for posterior cervical instrumentation. Aberrant vascular anatomy may predispose the vertebral artery for iatrogenic injury (1). For this reason, careful review of pre-operative films and meticulous surgical planning are required to minimize complications.
Historical context
Historically, posterior cervical fixation was based on wiring techniques, which improved fusion rates when compared with in situ fusion followed by cervical immobilization (1,2). These techniques required an intact posterior bony ring (such as the lamina, spinous process and facet joints, which may be compromised in some traumatic cases or in cervical decompressions), as well as were only able to restore posterior tension band without providing immediate stabilization (2). Wiring only offers stabilization for flexion, but does not immobilize the spine against extension, lateral bending or rotation forces, which may put the fixation at high risk for mechanical failure (1,2). Wiring techniques in the subaxial cervical spine were mainly based on interspinous wiring, such as those proposed by Rogers and Bohlman, since sublaminar techniques had a higher risk of neurological deterioration due to the small canal dimensions (2,4,5). Although wiring techniques are not commonly used today, they still have some role especially in children with very small spine dimensions were moderns’ screws could not be used, as well as in some salvage cases where screw fixation is not possible (1).
Screw fixation techniques
The development of new techniques for cervical fixation improves fusion rates and offers immediate spinal stability, avoiding or minimizing the need of post-operative cervical orthosis or prolonged immobilization. Current posterior cervical spine fixation techniques are mainly based on a construct with screw fixation attached to rigid rods, which provides immediate stabilization and high fusion rates despite earlier mobilization. In this paper, we discuss the current status and the most commonly used techniques of posterior subaxial cervical spine screw fixation.
Lateral mass (LM) screw fixation
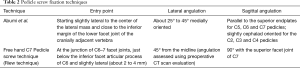
The LM is the bony structure between the inferior and superior facet joints, laterally to the lamina (between the lamina and the LM there is the medial facet line, a sulcus at the junction) (6). It is the most commonly used and is less technically demanding compared to other screw fixation techniques. Since its first description by Roy-Camille in the 1960s, many different variations of LM screw techniques had been proposed (1,2,7). As a general rule, the screws are angling laterally to decrease the risk of vertebral artery injury in the transverse foramen, and also aimed cranially to allow longer screws but not excessively long to avoid injuring the exiting nerve root. In Table 1 we described six different techniques of LM screw fixation according to the proposed surgical techniques (1,7-11).

Full table
General considerations about the techniques of LM fixation
Coe et al. performed a systematic review to evaluate the safety and efficacy of LM screw fixation (12). Comparative studies of LM vs. wiring techniques reported that the risk of complications was similar between both techniques (ranging from 0 to 7.1% vs. 0 to 6.3%, respectively). Complications evaluated in 18 case series reported nerve root injury in 1% [95% confidence interval (CI), 0.3% to 1.6% of patients], with no documented vertebral artery injury. Fusion rate was up to 97% in these cases and less than 1% of screw loosening was reported.
Hockel et al. performed a morphometric analysis of the LMs for optimal screw trajectory planning evaluating 55 patients who underwent LM screw fixation using a modified Magerl technique (13). Postoperative computed tomography (CT) were used to determine the LM anatomy, length of the screws, complication rates and bicortical screw percentages. The LM geometry was evaluated at different sagittal angulations (strict sagittal, 20°, 30°, ideal angulation) for the optimal screw trajectories at the C3–7 segments. They reported that, from 284 LM screws, the mean length was 16 mm and had 88% of bicortical purchase. Misplacement was observed in 3.8%. Interesting, LM thickness varied substantially in all cervical levels, within optimal angulation in sagittal plane increasing from C3 (14°) to C7 (38°). This increasing in angulation allows gains in screw length compared with strict sagittal plane insertion.
Nazarian technique is easily performed once the screw is inserted straight ahead to the LM (0° of lateral angulation) and perpendicular to the bone in the sagittal plane (9). However, longer screws may injury the vertebral artery (once there is no lateral angulation) (1). Riew technique is a freehand technique that is very easy to follow, with real intraoperative anatomic landmarks (lateral and sagittal angulation toward the upper and outer corner of the LM) (1). The only drawback of this technique is that the spinous process at C6 and C7, when prominent, may get in the way of achieving good lateral angulation (1).
Anatomic studies of LM screws
An anatomic study compared three different techniques (Magerl vs. Anderson vs. An technique) using 20 screws of 20 mm each (to over-penetrate the LMs on purpose), and evaluated the nerve violation rate in two specimens for each technique (14). Considering nerve violation, 95% of the screws reach the nerve using the Magerl technique, 90% using the Anderson technique and 60% using the An technique (P<0.05).
Henler et al. compared the Roy-Camille technique with the Magerl technique in 26 cadavers inserted by three spine surgeons (about 80–100 screws each) (15). An independent observer evaluated violation of nerve roots, facet joints, vertebral arteries and spinal cord. Pooled data analysis revealed that the Roy-Camille technique had less risk of nerve root injury (0.8% vs. 7.3%, P=0.02) compared with the Magerl technique, who had less risk of facet joint violation (2.4% vs. 22.5%).
Ebrahein et al. evaluated the mean safe LM screw lengths in two different techniques of fixation (Roy-Camille and Magerl) in cadaveric cervical specimens (16). Using 14 cervical spines, the LMs from C3 to C7 were drilled according to the techniques described by Roy-Camille in the right side and Magerl in the left side and the screw path length between the dorsal and ventral cortices were measured. Screw length decreases from C3 to C7 in both techniques (mean screw length from C3 was 15.7±1.7 to 11.3±0.8 mm at C7 in the Roy-Camille technique and the mean screw length in the Magerl technique was 15–16 mm, decreasing from C3 to C6 and with a mean value of 13.8 mm at C7. They proposed that a screw length of 14–15 mm is safe for Roy-Camille technique and 15–16 mm in the Magerl technique at C3 to C6, but shorter screws should be used at C7. A potential explanation for this is that C7 is a transitional vertebra, which the facet joint between C7 and T1 is similar to a thoracic facet joint, with small dimensions at the LM for proper screw insertion. Patients could not have acceptable C7 LM screw using any method. They concluded that this modified Roy-Camille technique using a higher starting point may be a better option for C7 LM screw fixation, avoiding placing the screw into the T1 facet joint.
Pedicle screw fixation
Pedicle screw fixation was first proposed in the lumbar spine, followed by the thoracic spine and, finally, Abumi et al. introduced pedicle screws at the subaxial cervical spine, which has superior pull-out strength when compared with LM screws but a potential higher risk of neurovascular injury (17). The technique proposed by Abumi is detailed in Table 2. In 2000, Abumi et al. reported that, from 1,024 cervical pedicle (CP) screws, there was 129 (12.60%) of lateral pedicle perforation and seven aborted pedicles (18).
Full table
Yoshihara et al. performed a systematic review comparing screw related complications of two different techniques: LM screws vs. CP screws in the subaxial spine (19). They evaluated clinical studies with surgical procedures of the subaxial cervical spine in which LM screws (ten studies) or CP screws (12 studies) that reported complications rate related to screws insertion. CP screws had a slightly but statistically higher risk of vertebral artery injury (P=0.012), but LM screw had a higher rate of screw loosening (P=0.09). Studies with CP screws were generally outside North America and LM screws generally from North America, suggesting regional differences in the use of both techniques. Complication rates were low for both techniques and, although vertebral artery injuries were more common in CP, they were extremely rare, in which the authors justified its use in select cases. By this reason, they also suggested that surgeons should evaluate the specific patients’ anatomy and use the technique according on individual case requirements. Another important consideration regarding CP screws is that they are commonly used at C2 and C7 due to larger pedicle dimensions at these levels, as well as the absence of vertebral artery in the C7 transverse foramen for most patients.
Due to the risk of neurovascular injuries, Celikoglu et al. proposed a mini-laminotomy for improving the safety and accuracy of CP screws (20). They palpated the cortical bone of the medial pedicle wall with a mini-laminotomy and using a small curette. The hand drill was then guidance based on the proper trajectory and screws from 26 to 30 mm were used in 214 patients (a total of 1,024 CP screws). A total of 129 screws had lateral perforation (12.60%), which 101 (9.86%) were classified as grade I (less than 2 mm of the lateral pedicle) and 28 (2.73%) grade II (critical perforation of the pedicle wall by screw placement larger than 2 mm). There was a higher perforation rate at C3 (P<0.05) and no symptom or sign of neurovascular injuries in their series.
Image-assisted CP screws
To improve the safety profile of CP placement, stealth navigation and 3D image Guidance have been utilized by various authors (21-23). Theologis and Burch reported their retrospective experience with 121 CP screws inserted using O-Arm and Stealth Navigation (4 at C2, 20 at C3, 22 at C4, 23 at C5, 18 at C6 and 34 at C7) (21). More than 99% of the screws were properly placed without any neurovascular injury. One screw breaches the medial wall leading to C5 nerve root palsy was found in a postoperative CT scan and was subsequently removed followed by laminoforaminotomies at C4–6. They reported that O-Arm imaging with stealth navigation was a safe and effective method for CP screw fixation for complex cervical surgeries. Ishikawa et al. also reported that 3D Image (O-Arm) based navigation system facilitates the insertion of CP screws, with no severe misplacement or neurovascular complications in 108 CP screws insertion in 21 consecutive patients (22).
Takahata et al. reported the results of a case control study where they compared the accuracy and safety of intraoperative C-arm cone beam CT placement (166 pedicle screws) vs. freehand CP screws under lateral fluoroscopy (1,065 pedicle screws) (23). The intra-operative 3D imaging from C-arm was used with a pilot screw without navigation system—they performed a preoperative planning to create a screw path in each pedicle, excluding small pedicles (less than 3.5 mm) created an entry point in the LM. Intraoperatively, a guided screw was freehand placed and the first intraoperative CT was performed to assess direction of pilot hole. The proper direction was then verified, followed by definitive screw insertion and then a second CT scan was performed. After 166 CP screws insertion, they reported that overall malposition rate of 2.4% compared with 14.8% in lateral fluoroscopy guided freehand placement. They reported that intraoperative 3D C-arm guidance resulting in accurate and safe screws placement, despite an increased risk of radiation exposure compared with lateral fluoroscopy.
In Table 2, the technique of CP fixation proposed by Abumi et al. and the C7 pedicle screw fixation using the technique proposed by Riew are summarized (1,17).
Subaxial intralaminar screw fixation
Proposed in 2004 by Wright NM, C2 crossing laminar screws were used in atlantoaxial fixation, craniocervical junction cases and also for C2 incorporation in subaxial constructions (24).
The small dimensions of the lamina at C3 to C6 limited the adaptation of intralaminar screws in the subaxial cervical spine. Cho et al. evaluated the anatomy for inserting translaminar screws in the subaxial spine (25). A total of 18 cadaveric cervical spines were used and a 1-mm CT scan was obtained with 3D reconstructions. They simulated bilateral screw entry points and their trajectories. The first screw was selected to achieve the maximal bone purchase, whereas the second one was selected to achieve the best diameter possible without cortical breach (not necessarily the best purchase). Diameters of 3.5 and 3 mm were simulated and, using caliper measurement, the same portions were measured in 11 of 18 cadavers. They reported that for C3, only one specimen allowed two screws (3 mm each), whereas the remained permitted only one unilateral screw of 3.5 mm. For C4, 37% of the specimens permitted 2 screws (3.5/3 mm or 3/3 mm) and the rest only one screw. For C5, two screws (3.5/3.5 or lesser) were allowed in 58% of the cases. For C6, 89% of the specimen permitted two screws (3.5/3.5 or less) and for C7 all specimens allowed 2 screws. The average length of the screws was 26.14 mm for the first screw and 24.01 mm for two screws for CT and 22.58 mm (first screw) and 23.44 mm (second screw). The proposal entry point for the first screw was the distance of the diameter of desired screw superior to the inferior margin of lamina-spinous process junction and target toward the most superomedial corner of the LM, whereas for the second screw was the distance of the diameter of the desired screw below the superior margin of lamina-spinous process junction and target toward the superolateral corner of LM.
For C7, there are more studies addressing translaminar screws, potentially due to the wider and larger lamina dimension (26). It can be a savage technique for LM or pedicle screw fixation. The technique is performed without fluoroscopy, with the starting point about 4 mm at the caudal aspect of the spinolaminar junction directing the drill guide toward the opposite lamina checking cortical violation; the second hole is made in the rostral aspect of the spinolaminar junction on the other side, also directing the drill guide in the contralateral lamina (generally towards the inferior portion of the laminas, which are thicker than the superior one) (1,27,28). A biomechanical cadaveric study suggested that the pullout strength of a C7 translaminar screw was similar to the C7 pedicle screw (P=0.06) (29).
Transfacet screw fixation
Another option for subaxial screw fixation is the transfacet screw (30). Biomechanical studies support the use of transfacet screw, although clinical studies are sparse (30-34). In Table 3 we described some different proposal techniques of transfacet screw fixation we found in our literature review (30-34). The majority of the techniques proposal to entry in the midportion or inferior portion of the LM, directing the screw caudally with mild or no lateral angulation.
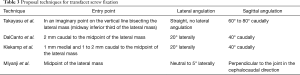
Full table
Muthukumar reported a narrative review of his own experience with transfacet screws (30). He proposed that the entry point should be 2 mm above the middle of the LM, curetting the facet joints before to facilitate fusion (packed with autologous bone graft). The drill guided is used perpendicular to the facet joint. He did not advocate any lateral angulation. During drill guidance, surgeons should fell the four cortical surfaces of the facet joints. Generally, 3.5 mm diameter, 16 mm length screws were used (ranging from 14 to 18 mm). He did not suggested use this to C7, due to the transitional characteristic of the C7–T1 facet joints (only used for C3 to C6). Some important technical tips from the authors: (I) cervical lordosis should be restored prior to facet screws insertion; (II) it may be difficult to use this technique at the upper levels in obese patients; (III) osteoporotic patients are at higher risk of facet fractures, and (IV) fixed cervical kyphosis is an absolute contra-indication to this technique. Finally, no rod fixation is necessary to attach the screw head in this technique, since direct motion unit fixation is performed.
Illustrative cases
Case 1
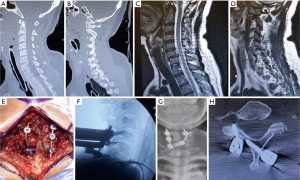
Lateral (Figure 1A) and antero-posterior (Figure 1B) plain radiographs of a multilevel cervical degenerative myelopathic patient treated with an anterior C34, C45 and C7T1 discectomies, a hemicorpectomy at C6 (involving the C56 and C67 discs), plating the bottom levels (C5–T1) at greater risk of pseudoarthrosis. Then, a posterior C3, C4, C5, C6 LM screw fixation and T1 pedicle screws were performed (Figure 1).
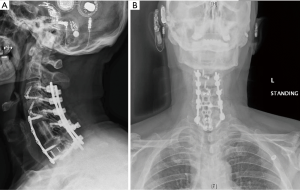
Case 2
Figure 2 shows lateral (Figure 2A) and antero-posterior (Figure 2B) plain radiographs of a multilevel cervical degenerative myelopathic patient treated with posterior augmentation of anterior decompression & arthrodesis. LM screw fixation at C3, C4, C5, C6 and pedicle screws at T1 were performed (Figure 2).
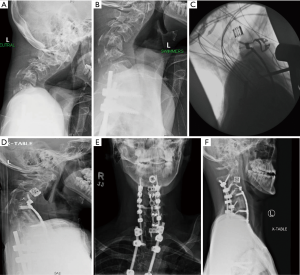
This young boy had a congenital cervical kyphosis associated with a previous thoracolumbar deformity correction. Figure 2A,B show lateral preoperative cervical plain radiographs with a clear cervical kyphosis. Intraoperative fluoroscopy (Figure 2C) shows the anterior cervical approach (C23 and C34 discectomies, C5 corpectomy, C67 and C7T1 discectomies) and deformity reduction. Figure 2D shows post-operative lateral X-ray after the anterior cervical approach with loss of reduction. Figure 2E,F show anteroposterior and lateral final plain radiographs after posterior cervical approach with C2 pars screws, subaxial LM screws and dominoed on to the thoracic instrumentation with good final alignment.
Case 3
A 40-years-old woman had a C6 left side fracture after a car accident. Midline sagittal CT scan did not show any dislocation (Figure 3A) and facet fracture had no significant gap between the bone fragments (Figure 3B). A trial of conservative treatment with a cervical brace was attempted. Once she persisted with severe cervical pain, a magnetic resonance imaging (MRI) was requested, with a new mild C67 spondylolisthesis and worsening of the fracture displacement (Figure 3C and D, respectively). We performed a C567 LM screw fixation at the right side and a C5 LM screw at the left side and a laminar screw at C7 was performed due to a broken LM of C7. Figure 3E shows intraoperative view of the posterior cervical construction. Figure 3F shows intraoperative lateral plain fluoroscopy showing the screws in the LM. Antero-posterior final X-ray (Figure 3G) and post-operative axial CT scan reconstruction at C7 (Figure 3G) show the LM screw at C7 and the laminar screw on the left side fixed in the right C7 lamina (Figure 3).
Conclusions
Subaxial cervical spine screw fixation is an important component for achieving successful cervical arthrodesis. Spine surgeons should be familiar with various different techniques in order to optimize clinical outcome. Advantages and disadvantages of each technique, as well as surgeons’ experience and patients’ specific characteristics should guide the choice of the specific technique selected.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Lee A. Tan and Ilyas S. Aleem) for the series “Advanced Techniques in Complex Cervical Spine Surgery” published in Journal of Spine Surgery. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: The series “Advanced Techniques in Complex Cervical Spine Surgery” was commissioned by the editorial office without any funding or sponsorship. LT serves as the unpaid editorial board member of Journal of Spine Surgery from Jan. 2019 to Jan. 2021 and served as the unpaid Guest Editor of the series. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Joaquim AF, Mudo ML, Tan L, et al. Posterior subaxial cervical spine screw fixation: a review of techniques. Global Spine J 2018;8:751-60. [Crossref] [PubMed]
- Ghori A, Le HV, Makanji H, et al. Posterior fixation techniques in the subaxial cervical spine. Cureus 2015;7:e338. [PubMed]
- Joaquim AF, Riew KD. Axis screw fixation – a step-by-step review of the surgical techniques. Arq Bras Neurocir 2017;36:101-7. [Crossref]
- Rogers WA. Treatment of fracture-dislocation of the cervical spine. J Bone Joint Surg Am 1942;24:24-58.
- Abdu WA, Bohlman HH. Techniques of subaxial posterior cervical fusions: an overview. Orthopedics 1992;15:287-95. [PubMed]
- Mohamed E, Ihab Z, Moaz A, et al. Lateral Mass Fixation in Subaxial Cervical Spine: Anatomic Review. Global Spine J 2012;2:39-46. [Crossref] [PubMed]
- Roy-Camille R, Roy-Camille M, Demeulenaere C. Ostéosynthèse du rachis dorsal, lombaire et lombo-sacré par plaques métalliques vissées dans les pédicules vertébraux et les apophyses articulaires. Presse Med 1970;78:1447-8. [PubMed]
- Roy-Camille R, Salient G, Mazel C. Internal fixation of the unstable cervical spine by a posterior osteosynthesis with plates and screws. In: Sherk HM, The Cervical Spine Research Society editors. The Cervical Spine. 2nd edition. Philadelphia: JB Lippincott, 1989:390-403.
- Nazarian SM, Louis RP. Posterior internal fixation with screw plates in traumatic lesions of the cervical spine. Spine (Phila Pa 1976) 1991;16:S64-71. [Crossref] [PubMed]
- Jeanneret B, Magerl F, Ward EH, et al. Posterior stabilization of the cervical spine with hook plates. Spine (Phila Pa 1976) 1991;16:S56-63. [Crossref] [PubMed]
- Anderson PA, Henley MB, Grady MS, et al. Posterior cervical arthrodesis with AO reconstruction plates and bone graft. Spine (Phila Pa 1976) 1991;16:S72-9. [Crossref] [PubMed]
- Coe JD, Vaccaro AR, Dailey AT, et al. Lateral mass screw fixation in the cervical spine: a systematic literature review. J Bone Joint Surg Am 2013;95:2136-43. [Crossref] [PubMed]
- Hockel K, Maier G, Rathgeb J, et al. Morphometric subaxial lateral mass evaluation allows for preoperative optimal screw trajectory planning. Eur Spine J 2014;23:1705-11. [Crossref] [PubMed]
- Xu R, Haman SP, Ebrahein NA, et al. The anatomic relation of lateral mass screws to the spinal nerves: a comparison of the Magerl, Anderson, and An techniques. Spine (Phila PA 1976) 1999;24:2057-61. [Crossref] [PubMed]
- Heller JG, Carlson GD, Abitbol JJ, et al. Anatomic comparison of the Roy-Camille and Magerl techniques for screw placement in the lower cervical spine. Spine (Phila PA 1976) 1991;16:S552-7. [Crossref] [PubMed]
- Ebraheim NA, Klausner T, Xu R, et al. Safe lateral-mass screw lengths in the Roy-Camille and Magerl techniques. An anatomic study. Spine (Phila Pa 1976) 1998;23:1739-42. [Crossref] [PubMed]
- Abumi K, Kaneda K. Pedicle screw fixation for nontraumatic lesions of the cervical spine. Spine (Phila Pa 1976) 1997;22:1853-63. [Crossref] [PubMed]
- Abumi K, Shono Y, Ito M, et al. Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine (Phila Pa 1976) 2000;25:962-9. [Crossref] [PubMed]
- Yoshihara H, Passias PG, Errico TJ. Screw-related complications in the subaxial cervical spine with the use of lateral mass versus cervical pedicle screws: a systematic review. J Neurosurg Spine 2013;19:614-23. [Crossref] [PubMed]
- Celikoglu E, Borekci A, Ramazanoglu AF, et al. Posterior Transpedicular Screw Fixation of Subaxial Vertebrae: Accuracy Rates and Safety of Mini-laminotomy Technique. Asian J Neurosurg 2019;14:58-62. [Crossref] [PubMed]
- Theologis AA, Burch S. Safety and Efficacy of Reconstruction of Complex Cervical Spine Pathology Using Pedicle Screws Inserted with Stealth Navigation and 3D Image-Guided (O-Arm) Technology. Spine (Phila Pa 1976) 2015;40:1397-406. [Crossref] [PubMed]
- Ishikawa Y, Kanemura T, Yoshida G, et al. Intraoperative, full-rotation, three-dimensional image (O-arm)-based navigation system for cervical pedicle screw insertion. J Neurosurg Spine 2011;15:472-8. [Crossref] [PubMed]
- Takahata M, Yamada K, Akira I, et al. A novel technique of cervical pedicle screw placement with a pilot screw under the guidance of intraoperative 3D imaging from C-arm cone-beam CT without navigation for safe and accurate insertion. Eur Spine J 2018;27:2754-62. [Crossref] [PubMed]
- Wright NM. Posterior C2 fixation using bilateral, crossing C2 laminar screws: case series and technical note. J Spinal Disord Tech 2004;17:158-62. [Crossref] [PubMed]
- Cho W, Le JT, Shimer AL, et al. Anatomy of Lamina in the Subaxial Cervical Spine With the Special Reference to Translaminar Screws: CT and Cadaveric Analysis With Screw Trajectory Simulation. Clin Spine Surg 2017;30:E535-9. [Crossref] [PubMed]
- Wilson PJ, Selby MD. C7 intra-laminar screws for complex cervicothoracic spine surgery-a case series. J Spine Surg 2017;3:561-6. [Crossref] [PubMed]
- Koltz MT, Maulucci CM, Sansur CA, et al. C7 intralaminar screw placement, an alternative to lateral mass or pedicle fixation for treatment of cervical spondylytic myelopathy, kyphotic deformity, and trauma: A case report and technical note. Surg Neurol Int 2014;5:4. [Crossref] [PubMed]
- Hong JT, Yi JS, Kim JT, et al. Clinical and radiologic outcome of laminar screw at C2 and C7 for posterior instrumentation - review of 25 cases and comparison of C2 and C7 intralaminar screw fixation. World Neurosurg 2010;73:112-8. [Crossref] [PubMed]
- Ilgenfritz RM, Gandhi AA, Fredericks DC, et al. Considerations for the use of C7 crossing laminar screws in subaxial and cervicothoracic instrumentation. Spine (Phila Pa 1976) 2013;38:E199-204. [Crossref] [PubMed]
- Muthukumar N. Transfacet screw fixation of the subaxial cervical spine--how I do it? Acta Neurochir (Wien) 2013;155:1235-9. [Crossref] [PubMed]
- Miyanji F, Mahar A, Oka R, et al. Biomechanical differences between transfacet and lateral mass screw-rod constructs for multilevel posterior cervical spine stabilization. Spine (Phila Pa 1976) 2008;33:E865-9. [Crossref] [PubMed]
- Klekamp JW, Ugbo JL, Heller JG, et al. Cervical transfacet versus lateral mass screws: a biomechanical comparison. J Spinal Disord 2000;13:515-8. [Crossref] [PubMed]
- DalCanto RA, Lieberman I, Inceoglu S, et al. Biomechanical comparison of transarticular facet screws to lateral mass plates in two-level instrumentations of the cervical spine. Spine (Phila Pa 1976) 2005;30:897-2. [Crossref] [PubMed]
- Takayasu M, Hara M, Yamauchi K, et al. Transarticular screw fixation in the middle and lower cervical spine. Technical note. J Neurosurg 2003;99:132-6. [PubMed]


