
Suprailiac versus transiliac approach in transforaminal endoscopic discectomy at L5–S1: a new surgical classification of L5—iliac crest relationship and guidelines for approach
IntroductionOther Section
Percutaneous endoscopic lumbar discectomy for lumbar disc herniations has been an established and well-known procedure (1). It was first introduced in 1983 by Kambin and Gellman (2). Kambin and Schaffer, in their study used arthroscope for visualization and excision of the disc (3). Yeung AT developed rigid working channel endoscope for a transforaminal endoscopic discectomy and proposed a crystallized learning objective of precise needle placement to the pain generator, the YESS system (4). Developments of technique and endoscopic instruments lead to expansion of indications of this procedure. Yeung and Gore, in their study, mentioned that all disc levels from T10 to S1 are accessible to this procedure. They, however, indicated that the successful results depend on the indications and contraindications of this procedure (5).
Spinal surgery at junctional areas has always been challenging in terms of surgical approaches. L5–S1 level has its challenges for the endoscopic procedure. At L5–S1, the available surgical options for disc herniations include microlumbar discectomy, microendoscopic discectomy, suprailiac transforaminal approach, transiliac transforaminal approach and interlaminar endoscopy (6). However, sometimes transforaminal endoscopic discectomy at L5–S1 may be challenging due to high iliac crest, sacral ala, large transverse process, wide facet joint and narrow foramen (7). Several studies have reported transforaminal endoscopic discectomy at L5–S1 by the transiliac approach to be feasible and safe (8,9). Transiliac approach allows entering into the disc in the line of inclination. The only disadvantage is of drilling the ilium bone which may lead to increased blood loss, pain and discomfort to patient intra-operatively, whereas suprailiac approach can avoid these iliac bone-related problems. But in case of suprailiac approach, entry into the disc may not be in the line of inclination needing a more expansile foraminotomy and/or annulotomy (6). The vertical collapse in the aging spine may further complicate the situation.
However, so far to our knowledge no radiological classification or approach guidelines have been reported in the literature for pre-operative assessment and decision making at L5–S1 for transforaminal endoscopic discectomy. Our study aims to validate a new radiograph based surgical classification and approach guideline for selection of suprailiac or transiliac transforaminal approach at L5–S1.
MethodsOther Section
Patients
A prospective study was performed on a cohort of 90 consecutive patients of transforaminal endoscopic discectomy by transiliac or suprailiac approach for L5–S1 disc herniation from June 2016 to June 2018. The pre-operative radiological assessment was done on anteroposterior (AP) and lateral radiographs of the lumbosacral spine. A note was made in radiographs to include both the hip joints in AP and lateral views. L5 spinous process must be equidistant from both the pedicles on AP view.
Inclusion/exclusion criteria
The inclusion criteria were:
- All types of L5–S1 herniations i.e., central, paracentral, foraminal, extraforaminal and migrated extruded herniations;
- All type of herniations at last mobile segment in cases with transitional anatomy (i.e., L4–5 herniations in sacralized L5 and S1–2 herniations in lumbarized S1).
The exclusion criteria were:
- Sequestrated dorsally migrated herniations;
- Concomitant multilevel bilateral lumbar canal stenosis;
- Fixed pelvic obliquity;
- Previous ilium deformity;
- Associated instability.
Radiographic criteria on the anteroposterior (AP) view (Figure 1)
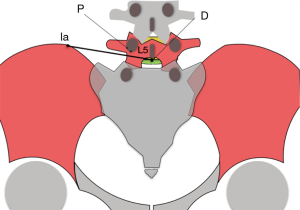
The following parameters were defined to assess the feasibility of the transforaminal access to the L5–S1 level on the anteroposterior radiographic view:
Ia: Most medial highest point on iliac crest in AP view.
D: Point on the midline on the posterior margin of inferior end-plate of L5. If inferior endplate of L5 is not visible, then most caudal point at spinous process of L5 is considered (Note: anterior margin of inferior end plate of L5 which appears concave superiorly, should not be considered).
P: Point marked at 6 o’clock of the ipsilateral pedicle of L5.
Ia D: Line joining point Ia & D.
Radiographic criteria on the lateral (Lat) view (Figure 2)
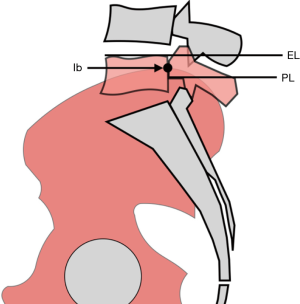
The following parameters were defined to assess the feasibility of the transforaminal access to the L5–S1 level on the lateral radiographic view:
Ib: Most dorsal highest point on iliac crest when both the iliac crests are coinciding. If these points are not coinciding then the point midway between those two points is considered.
EL: Line drawn along the upper end plate of L5 vertebral body.
PL: Line drawn along the inferior margin of L5 pedicle parallel to upper end plate of L5.
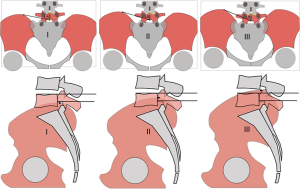
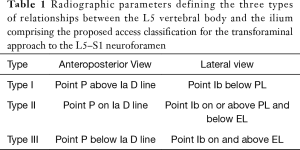
Proposed radiograph based surgical classification
For the purpose of stratifying patients for suprailiac or transiliac transforaminal access to the L5–S1 neuroforamen, the authors proposed the following radiograph based surgical classification defining three types of the relationship of iliac crest to L5 vertebral body (Figure 3). The classification and the constellation of its defining radiographic variables is summarized in Table 1. The proposed approach guidelines to choose suprailiac approach or an approach through a transiliac window are summarized in Table 2.
Full table
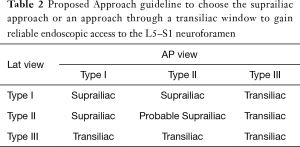
Full table
Choice of approach
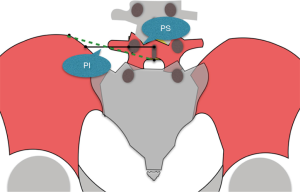
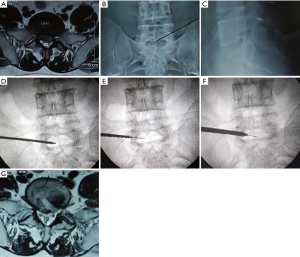
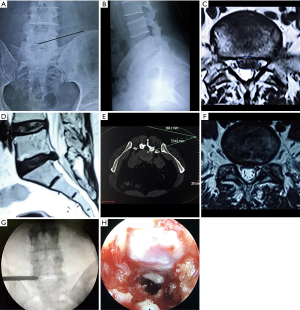
The choice of suprailiac or transiliac approach was made on the basis of the proposed radiological classification and was performed accordingly. In type II/II relationships, approach was determined on the basis of the type of herniation. In the authors experience, central or superiorly migrated herniations may be best approached with the transiliac approach, whereas paracentral or foraminal herniations may be preferably accessed by suprailiac approach. The ratio of pedicle-iliac crest distance and pedicle spinous process distance (PI:PS) is of importance during this assessment. It is defined as a horizontal line passing through the middle of the L5 pedicle joining the L5 spinous process to medial margin of iliac crest. If the distance from the lateral pedicular line to iliac crest (PI) is more than the lateral pedicular line to spinous process (PS), the suprailiac approach can be attempted considering type of herniation as well (Figure 4). Intermediate cases may exist and the authors recommend to make the choice of preferred approach on the basis of all clinical factors including the type of herniation and its location. Representative case examples are shown in Figures 5 and 6 for either approach.
Surgical technique
All procedures were performed in a prone position on a radiolucent table using c-arm fluoroscopy under local anesthesia & conscious sedation. Patients could communicate with the surgeon during the entire procedure, which enabled the surgeon to avoid damaging the neural tissues. The skin entry point was determined using standard skin entry point measuring methods following the YESS™ technique (4). Besides, measurements on preoperative MRI and CT scans were used to verify the distance from the midline to the skin entry point. Typically, the entry point was approximately located 11 to 14 cm from the midline depending upon the type of herniation, patient’s weight & central obesity. After the local anesthesia, a small stab incision is taken to facilitate needle entry, and the selected approach under fluoroscopic guidance inserts an 18-gauge needle. The Entry points were labeled from medial to lateral as (I) 45–45, (II) posterolateral (PL), (III) tip of the spinous process (TOSP), and (IV) dorsum of the facet joint (DFJ).
For transiliac approach, sequential reamers (Maxmore Gmbh) were used to make window in the iliac bone after infiltration of xylocard 1% on the periosteum. Regardless of the chosen suprailiac or transiliac access, a foraminotomy may be required for the working sleeve entry. In those cases, trephines, serial reamers, and a motorized burr were used. The authors frequently observed that a foraminotomy with a medialization of the annulotomy was required in cases with: (I) hard, calcified disc herniations, (II) a central extruded or migrated herniations, and (III) endplate osteophytes interfering with the access to the intervertebral disc. These combined maneouvers resulted in adequate decompression of the traversing and exiting nerve roots, which was assessed by the authors under direct videoendoscopic visualization as unimpeded floating and associated epidural fat mobility or movement. The free pulsations of the neural elements satisfied the authors as an adequate decompression.
Postoperative rehabilitation and clinical follow-up
Patients were allowed sitting, standing, and ambulation 1 hour after the procedure and discharged the next day. Patients were asked to resume light activities over 6 weeks gradually. Follow-up was done at 6 weeks, three months, and six months. We report functional outcome data obtained during the first six months postoperative follow-up period using the visual analog scale (VAS, 0–10) and the Oswestry Disability Index (ODI, 0–100%). These functional outcome data were obtained at each follow-up visit.
Correlative surgical outcomes analysis
For the clinical outcome analysis, descriptive statistics including mean and standard deviation of the pre- and post-operative VAS and ODI were calculated at final follow-up using IBM SPSS Statistics software, Version 25.0. A paired t-test was used to calculate any statistically significant difference in functional clinical outcomes. Any association between the type of approach—suprailiac or transiliac—and outcomes, was assessed by crosstabulation methods using the Pearson χ2 and the likelihood-ratio χ2 tests as statistical measures of association. An informal assessment of the interrater reliability of the proposed radiograph based surgical classification between two independent observers was assessed by calculating the percentage of agreement in the designation of type I, type II, or type III categories. Formal kappa analysis was not attempted as it was beyond the scope of this feasibility study. The authors are planning to perform a formal statistical intra- and inter-rater agreement analysis with a larger number of patients and observers in the future.
ResultsOther Section
In our study, a total of 90 patients were included with 54 male and 36 female patients. The mean age of the cohort was 39 years (range, 21 to 71 years). Transforaminal endoscopic discectomy was performed through the suprailiac approach in 46 patients and through transiliac approach in 44 patients. Demographic data are listed in Table 3. In all cases, the preoperative radiological assessment was done, and the preoperative planning was contemplated using the criteria listed in the method section of this manuscript.
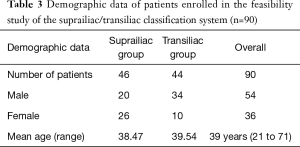
Full table
The overall VAS score decreased from a preoperative value of 7.67 to 2.22 at 6 months follow-up (P value <0.05), and the overall ODI score improved from 66.13 to 15.11 (P value <0.05). Similarly, the VAS score in suprailiac and transiliac groups improved from 7.60 to 2.17 (P value <0.05) and 7.72 to 2.27 (P value <0.05), respectively. The ODI score in suprailiac and transiliac groups also improved from 67.08 to 14.52 (P value <0.05) and 65.13 to 15.72 (P value <0.05), respectively. The functional clinical outcome data are listed in Table 4. The informal agreement analysis of the radiograph based surgical classification system in the preferred choice of approach showed 92.5% between two independent observers.

Full table
DiscussionOther Section
Minimally invasive surgical options for L5–S1 disc herniations include microlumbar discectomy, microendoscopic discectomy, transforaminal percutaneous decompression, and interlaminar approach (5,9). The interlaminar approach can be useful in L5–S1 disc herniations for the reason that the interlaminar window at L5–S1 is the largest (31 mm on average) and the little overhang of upper lamina makes interlaminar approach possible and relatively easy (1). In the interlaminar approach, however, neural structures are encountered before the removal of the disc. This has a higher risk of neural injury, including postoperative dysesthesia because it requires manipulation of the traversing nerve root. Moreover, the interlaminar approach is preferred for axillary type and high-migrated disc herniations (10). Choi et al. in their study of 67 patients with interlaminar approach reported complications such as dural tears, transient dysesthesia, recurrence, and conversion to open surgery in few cases (11). Transforaminal endoscopic decompression for L5–S1 disc herniations can be approached by suprailiac window in patients with low iliac crest. In patients with high iliac crests, Lee et al. performed foraminoplasty to enlarge the foramen using endoscopic bone cutters with the intent of reducing the occurrence of exiting nerve injuries (7).
Choi et al. in their study described the relation of the iliac crest with L5–S1 disc space. In cases where the iliac crest is above the mid-L5 pedicle in lateral radiography, foraminoplasty may be considered for suprailiac transforaminal access for L5–S1 disc herniation. Suprailiac transforaminal access can be utilized without difficulty in patients with low iliac crest, where the iliac crest height is below the mid-L5 pedicle (12). While accessing the herniations at L5–S1, the commonly faced challenges are a high iliac crest, large transverse process of L5, sacral ala, narrow AP dimension of foramina, considerable interpedicular distance and disc inclination due to lumbar lordosis (6,7,11). Osman et al. studied the endoscopic trans-iliac approach for L5–S1 disc herniations and found it to be feasible and safe with minimal blood loss and short operating time (8,9).
The transiliac approach provides a technically easier inline access to the L5–S1 disc space directly targeting the pain generator at the expense of the drilling the iliac bone, and restricted maneuverability of the rigid endoscope through the transiliac bony window. Other side effects include pain and discomfort to patient intra- and postoperatively. Suprailiac approach can avoid these iliac bone related problems, but entry into the disc may not be inline of disc inclination. Hence, these access problems may limit the ability to carry out an adequate decompression. The chances of iatrogenic endplate injury increase when the cannula is not inline with the disc inclination. A bigger foraminotomy and annulotomy may be required to access the herniation, to achieve adequate decompression and to reduce the chances of exiting nerve root injury (6,7,13-15).
In our experience, transforaminal endoscopic discectomy at L5–S1 usually needs foraminotomy or medialization of annulotomy, except in cases of foraminal or paracentral soft herniations. Datar et al. described certain technical modifications to reach the dorsal part of the disc in the midline and to access ventral epidural space for central herniations (16). Even though initially, our preference in this study had been suprailiac approach, transiliac approach was adopted in cases where we encountered the possibly equivocal type II/II relationship (Table 2) on plain preoperative radiography. Based on our study, the authors recommend:
- Type I/I, I/II and II/I relationship can be approached by suprailiac access;
- Type III relationship in either AP or lateral view, is preferably accessed via the transiliac approach;
- Type II/II relationship can be approached through either suprailiac or transiliac window depending on the type of herniation and pedicle-iliac crest to pedicle spinous process distance ratio PI:PS (vide supra).
In our study, type II/II relationship was encountered in six cases. In four cases, the transiliac approach was required because of central and migrated herniations. In the remaining two cases, a suprailiac endoscopic discectomy was performed. In both these latter two cases, the paracentral herniation and pedicle-iliac crest distance to pedicle spinous process distance ratio (PI:PS) favored the suprailiac approach. Cases with type II/II relationship can be classified under “Probable suprailiac approach”. In these cases, the choice of approach was decided based on the type of disc herniation and the pedicle-iliac crest to pedicle spinous process distance ratio (PI:PS).
The limitations of this feasibility study lie in the small patient cohort and the assessment of two-dimensional radiographs. However, the authors favored plain radiography as a screening tool since they are readily available in most patients. No other costly advanced imaging study or technology was required to stratify patients preoperatively before the L5–S1 transforaminal endoscopic discectomy surgery.
Additional limitations are inherent to the informal reliability assessment between the two independent evaluators. A formal Cohen Kappa coefficient analysis with more than two observers in a large patient group is planned for the future, but was beyond the scope of this feasibility study with limited clinical follow-up. Additionally, the comparison of functional clinical outcome results between patients undergoing L5–S1 transforaminal endoscopic decompression with either the suprailiac or the transiliac approach was also beyond the scope of this study and will have to be attempted in future clinical studies. Similarly, the proposed use of the approach guidelines will have to be validated by correlating their choice to clinical outcomes. Ultimately, the question is whether there is an added benefit to patients with a problematic anatomical transforaminal access to their L5–S1 neuroforamen by stratifying select cases for the transiliac approach. The authors envision a more extensive study group and three-dimensional radiological assessments by multiple independent observers to ultimately achieve this validation of their classification.
In spite of these limitations, the authors stipulate that their proposed radiograph based surgical classification provides the basis for an easy-to-understand patient selection guideline for either of the two conventional transforaminal approaches to the L5–S1 neuroforamen. The authors' work is relevant to patients with a high iliac crest or other bony obliterations that may be a result of a variation of normal or transitional anatomy, or vertical collapse of the aging spine thereby impeding the direct transforaminal access to the L5–S1 neuroforamen with a straight, rigid spinal endoscope. The authors’ classification and approach guideline system go beyond the choice of the suprailiac or transiliac approach for percutaneous transforaminal endoscopic discectomy. It also has implications to the required extent of a wider medialized annulotomy during the decompression procedure and assists the surgeon preoperatively in making educated decisions to avoid unexpected intraoperative difficulties.
ConclusionsOther Section
Our new surgical classification and approach guideline system based on radiograph provides a well-defined method to choose the most appropriate transforaminal approach for endoscopic discectomy at L5–S1 level. The transiliac approach should be considered in all with type III/III, type II/III, type III/II and certain patients with type II/II. The suprailiac approach can be considered as most appropriate in type I/I, I/II, II/I and selected type II/II L5-iliac crest relationship for transforaminal endoscopic surgery at L5 S1.
AcknowledgmentsOther Section
None.
FootnoteOther Section
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by institutional ethical committee of Global SNG Hospital and written informed consent was obtained from all patients.
ReferencesOther Section
- Choi G, Pophale CS, Patel B, et al. Endoscopic spine surgery. J Korean Neurosurg Soc 2017;60:485-97. [Crossref] [PubMed]
- Kambin P, Gellman H. Percuraneous lateral discectomy of the lumbar spine: A preliminary report. Clin Orthop Relat Res 1983.127-32.
- Kambin P, Schaffer JL. Percutaneous lumbar discectomy. Review of 100 patients and current practice. Clin Orthop Relat Res 1989.24-34. [Crossref] [PubMed]
- Yeung AT. Minimally invasive disc surgery with the Yeung Endoscopic Spine System (YESS). Surg Technol Int 1999;8:267-77. [PubMed]
- Gore S, Yeung A. The “inside out” transforaminal technique to treat lumbar spinal pain in an awake and aware patient under local anesthesia: Results and a review of the literature. Int J Spine Surg 2014;8. [Crossref] [PubMed]
- Mahesha K. Endoscopic transiliac approach to L5-S1 disc and foramen, technique and results. J Orthop Allied Sci 2018;6:22-8. [Crossref]
- Lee SH, Kang HS, Choi G, et al. Foraminoplastic ventral epidural approach for removal of extruded herniated fragment at the L5-S1 level. Neurol Med Chir (Tokyo) 2010;50:1074-8. [Crossref] [PubMed]
- Osman SG, Marsolais EB. Endoscopic transiliac approach to L5-S1 disc and foramen. A cadaver study. Spine (Phila Pa 1976) 1997;22:1259-63. [Crossref] [PubMed]
- Osman SG, Sherlekar S, Malik A, et al. Endoscopic trans-iliac approach to L5-S1 disc and foramen - a report on clinical experience. Int J Spine Surg 2014;8:20. [Crossref] [PubMed]
- Choi KC, Kim JS, Ryu KS, et al. Percutaneous endoscopic lumbar discectomy for L5-S1 disc herniation: Transforaminal versus interlaminar approach. Pain Physician 2013;16:547-56. [PubMed]
- Choi G, Lee SH, Raiturker PP, et al. Percutaneous endoscopic interlaminar discectomy for intracanalicular disc herniations at L5-S1 using a rigid working channel endoscope. Neurosurgery 2006;58:ONS59-68; discussion ONS59-68.
- Choi KC, Park CK. Percutaneous Endoscopic Lumbar Discectomy for L5-S1 Disc Herniation: Consideration of the Relation between the Iliac Crest and L5-S1 Disc. Pain Physician 2016;19:E301-8. [PubMed]
- Tezuka F, Sakai T, Abe M, et al. Anatomical considerations of the iliac crest on percutaneous endoscopic discectomy using a transforaminal approach. Spine J 2017;17:1875-80. [Crossref] [PubMed]
- Kapetanakis S, Gkasdaris G, Angoules AG, et al. Transforaminal Percutaneous Endoscopic Discectomy using Transforaminal Endoscopic Spine System technique: Pitfalls that a beginner should avoid. World J Orthop 2017;8:874-80. [Crossref] [PubMed]
- Krzok G. Transpedicular Endoscopic Surgery for Highly Downmigrated L5-S1 Disc Herniation. Case Rep Med 2019;2019:5724342. [Crossref] [PubMed]
- Datar GP, Shinde A, Bommakanti K. Technical consideration of transforaminal endoscopic spine surgery for central herniation. Indian J Pain 2017;31:86-93. [Crossref]



