
The Berg balance scale for assessing dynamic stability and balance in the adult spinal deformity (ASD) population
Introduction
Patients with adult spinal deformity (ASD) present with a variety of symptoms, including lower back pain, radicular pain, and cosmetic issues (1). As a result of their scoliotic curve, these patients suffer from a three-dimensional, structural problem that often impairs normal standing balance and gait mechanics. Over the recent decade, there has been a focus on sagittal and spinopelvic parameters and their ability to drive health related quality of life (HRQOL) outcomes (2). There have been numerous attempts to classify the pathology based on two-dimensional radiographic measurements (3).
However, in a homogenous ASD population, recent evidence suggests that static radiographic parameters may not correlate as well as previously thought with either HRQOL measures (4) or clinical outcomes (5). Although sagittal parameters and spinopelvic measurements represent tangible and concrete targets for spinal deformity surgeons, they are likely not the sole driver of patient outcome. Two-dimensional radiographic parameters are measured in an upright, static position which restricts their ability to assess the dynamic postural changes that occurs with activities of daily living (ADL). As such, patients with ASD have been shown to walk with a greater forward tilt of the trunk as compared to that when standing (6).
Despite the focus on sagittal parameters, the influence of dynamic posture, standing balance, and walking balance on ASD patients have not yet been extensively studied. There are multiple clinical measurement tools reported in the physiatry and neurology literature that have aimed to quantify balance and dynamic stability in patients with neuromuscular disorders—notably the Berg Balance Scale (BBS), physical performance test, and Balance Evaluation Systems Test (BESTest) (7,8). The BBS was developed to measure balance by assessing the performance of functional tasks. Physiatrists have advocated the BBS as a useful tool for evaluation of the effectiveness of physical therapeutic interventions and for quantitative descriptions of function in clinical practice and research. The purpose of the current study was to determine if BBS is a useful metric for evaluating functional status in ASD patients.
Methods
After Institutional Review Board approval and informed consent, ASD patients were prospectively evaluated from 2014 through 2016 at a single, high-volume spine surgery center. Patients were screened for inclusion criteria, including the requirement of surgical thoracolumbar fusion extending to the pelvis. Balance and dynamic stability was quantified in each patient with the BBS. Any patient who failed to complete BBS testing preoperatively and at six months postoperatively was excluded. Additionally, any patient with less than 2 years of clinical follow up was excluded. The BBS clinical measurement was performed and scored by a certified physical therapist with extensive experience with the scale.
Standard demographic, radiographic and surgical data were collected. Demographic data included a detailed past medical history specific for neuropathy, diabetes, visual impairment, vestibular disease, cervical spine pathology, multiple falls, and other disorders that may impact neuromuscular control. Baseline and postoperative radiographic data included sacral vertical axis (SVA), major/minor coronal Cobb angles, thoracic kyphosis (T2–T12), lumbar lordosis (L1–S1), pelvic incidence and pelvic tilt. Changes in HRQOL were measured through the Oswestry disability index (ODI), EuroQOL-5D, and numeric rating scales (0 to 10) for back and leg pain. Process measures, such as proportion of patients who agree to undergo the test, the time it takes to administer the test, and impediments to test administration in the clinic, were also recorded.
Unadjusted univariate analysis was performed to determine the mean differences between measurements utilizing independent student t-test for continuous data and Chi-squared or Fischer’s exact testing for categorical variables. Findings were considered statistically significant when the P value was <0.05. Analysis was conducted using IBM SPSS Statistics Version 24.
Results
Twenty-one patients enrolled in the study. Of the 21 patients, 19 (90.5%) completed preoperative and postoperative BBS. The mean age was 59.8±13.3 years with 14 females (73.7%). There were 3 patients with diabetes mellitus (15.8%), 6 patients with neuropathy (31.6%), 14 patients requiring corrective glasses (73.7%), 2 patients with prior eye surgery (10.5%), 3 patients with vestibular disease (15.8%), and no patients with a history of stroke. There were 2 patients (10.5%) with neurologic disease—epilepsy and post-polio syndrome. Two patients (10.5%) had an oncologic history—one with metastasis (5.3%). Three patients had a history of multiple falls (15.8%) and four patients required assistive devices for ambulation (21.1%). There were no patients who required a wheelchair preoperatively or postoperatively (Table 1).
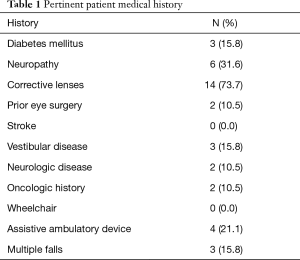
Full table
There was a statistically significant improvement in all radiographic parameters outcome scores (Table 2) after surgery. The major coronal Cobb angle improved from 27.86° pre-op to 13.03° post-op (P=0.002); thoracic kyphosis improved from 33.22° to 44.29° (P=0.002); and lumbar lordosis improved from 27.64° to 42.39° (P=0.000).
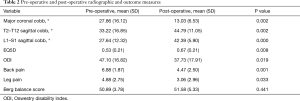
Full table
The EQ5D domain improved from 0.53 to 0.67 (P=0.008) and ODI decreased from 47.10 to 37.73 (P=0.019) after surgery. Back pain decreased from 6.88 to 4.47 (P=0.001) and leg pain decreased from 4.88 to 3.06 (P=0.033) after surgery. Balance stability, as assessed by BBS, did not change significantly with surgical intervention (50.89 to 51.58, P=0.441). Only one patient had a BBS score low enough to be considered a medium fall risk. Four patients required a revision surgery. Two patients had revision surgery for both non-union and proximal junctional kyphosis (PJK), one patient for nonunion and one patient for PJK. There was no difference in the pre-op BBS scores in the four patients that had revision surgery compared to those that did not.
Discussion
Sagittal alignment correlates with HRQOL in ASD both before and after surgery (2). However, the correlation between correction of sagittal alignment and clinical improvement has been more difficult to demonstrate (Ha). Recent evidence supports the concept that static, radiographic parameters may not likely to be the sole driver of outcomes (4,9-11). Although authors have reported a discrepancy between standing posture and sagittal balance during walking in patients with ASD (6), the exact influence of dynamic variables, including standing and walking balance, on ASD patients has not yet been defined. The Dubousset “cone of economy” illustrates importance of balance in maintaining an upright posture and minimizing energy expenditure with standing and walking (12). Our previously limited focus on purely mechanical factors and alignment in ASD may be imperfect and dynamic stability may play a larger role in maintenance of the cone and the HRQOL outcomes of ASD patients than previously understood.
Clinical balance and proprioception has been studied preliminarily in adolescent idiopathic scoliosis populations (13) and in osteoporotic thoracic kyphosis (14). However, there have been relatively few studies evaluating balance in ASD. Anecdotally, surgeons have noted poor outcomes and higher revision rates in patients with associate neuropathic or neurologic pathologies who have undergone surgical correction of their deformity. While this is well document for patients with substantial neurologic disorders, such as Parkinson’s disease (15), the impact of lesser neurologic impairment or other abnormalities of balance has not been fully elucidated. Glassman and colleagues attempted to evaluate the neurologic issues affecting deformity surgery. The authors reported that 76% of patients who suffered proximal junctional kyphosis also suffered from co-morbidities that adversely affected balance, irrespective of alignment (9). A follow up study similarly reported 75% versus 32% rate of preoperative neurologic comorbidities in a matched series of proximal junctional failure (PJF) and non-PJF deformity patients (P<0.001) (11). A lack of neuromuscular control, regardless of the mechanism or etiology, may contribute to an inability to rebalance the spine cephalad to a long fusion construct. Similarly, Yagi et al. showed that corrective spinal surgery for ASD improved radiographic spinal alignment, but failed to improve standing stability (10). This data suggests that neuromuscular fatigue and dysfunction in the proprioceptive and postural response system may affect balance in ASD patients.
Human balance is regulated by a complicated system of neural and musculoskeletal proprioceptive mechanisms with the integration of vestibular, visual, and somatosensory information (16). There have been multiple clinical measurement tools designed to quantify balance and dynamic stability in patients with neuromuscular dysfunction. The BBS was one such clinical tool developed to assess balance through the performance of functional tasks (7). Although originally developed to measure balance in an isolated elderly population, it has since been used to measure balance in a wide variety of patients and evaluated in several reliability studies (17). The scale involves 14 balance tests, each of which are scored 0 (lowest function) to 4 (highest function). The scores are summed to make a total score between 0 and 56, where 0–20 is a high fall risk, 21–40 is a medium fall risk, and 41–56 is a low fall risk. We sought to determine if BBS is a useful metric for evaluating functional status in ASD patients.
In the current study, we reported a statistically significant improvement in outcome scores and radiographic parameters with surgical treatment of ASD. However, there was no change in BBS scores before and after surgical intervention. Moreover, when comparing patients who underwent revision to those who did not, there was no statistical difference in the preoperative BBS scores. There was only a single patient in our series with a BBS score low enough to be considered a medium fall risk suggesting that the scale may have a significant ceiling effect in the ASD population.
Although successfully evaluated in several reliability studies, the BBS appeared to exhibit ceiling effects in our small series of ASD patients. The ceiling effect is likely due to the lower variability in balance in the operative ASD population and because of this, the BBS was unable to discriminate between the patients. Even if there was a real change in balance and dynamic stability from preoperative to postoperative assessment, the BBS scale was unlikely to detect a difference.
On the other hand, patient performance on the BESTest, another clinical assessment of dynamic balance, has been shown to impact HRQOL measures greater than 2D radiographic sagittal parameters and demographic variables in ASD. Unlike the BBS, performance on BESTest was able to predict nearly 3% of variance in ASD HRQOL measures (18). Thus, it is plausible that a clinical measurement tool with increased sensitivity and granularity may provide ability to detect the differences in balance of ASD patients.
The present study had a small sample size consisting only of operative ASD patients, which is a potential weakness. However, the data was collected in a prospective fashion with a minimum of 2-year follow-up. Extensive corrective fusion surgery for ASD may take a long time to recover functionally. Administration of the BBB at six months after surgery may have not allowed enough time for the patients to reach maximum improvement in over-all health and balance. All radiographic measures were performed at a single center using standardized image analysis software to minimize potential variation in technique. Further variation was minimized with a single certified physical therapist performing every clinical examination independently, as the BBS instructions may be interpreted and delivered in slightly different ways by different assessors.
Conclusions
Although balance and dynamic stability likely contribute to the improvement of HRQOL scores in ASD patients, BBS did not appear to be associated with measures of clinical and radiographic improvement in this small pilot series. Unfortunately, the test exhibited a ceiling effect, which was potentially problematic in that it lacked the ability to discriminate differences in balance stability in this patient population. Additionally, BBS required significant time with a trained physical therapist for administration. A more sensitive, streamlined assessment, such as BESTest, quantified Romberg, or dynamic posturography, may provide the power to differentiate dynamic subtleties in this patient population. Continued effort and future research is necessary to identify a viable measure of balance dysfunction in ASD patients.
Acknowledgments
Funding from the Fischer-Owen Kotcamp Orthopaedic Fund was received for the design, the collection, analysis, and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study has received Institutional Review Board approval and informed consent.
References
- Engsberg JR, Bridwell KH, Reitenbach AK, et al. Preoperative gait comparisons between adults undergoing long spinal deformity fusion surgery (thoracic to L4, L5, or sacrum) and controls. Spine 2001;26:2020-8. [Crossref] [PubMed]
- Glassman SD, Bridwell K, Dimar JR, et al. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 2005;30:2024-9. [Crossref] [PubMed]
- Schwab F, Ungar B, Blondel B, et al. Scoliosis research society - Schwab adult spinal deformity classification. Spine (Phila Pa 1976) 2012;37:1077-82. [Crossref] [PubMed]
- Chapman TM, Baldus CR, Lurie JD, et al. Baseline patient-reported outcomes correlate weakly with radiographic parameters. Spine (Phila Pa 1976) 2016;41:1701-8. [Crossref] [PubMed]
- Ha KY, Jang W, Kim Y, et al. Clincial relevance of the SRS-Schwab classification for degenerative lumbar scoliosis. Spine (Phila Pa 1976) 2016;41:E282-8. [Crossref] [PubMed]
- Arima H, Yamato Y, Hasegawa T, et al. Discrepancy between standing posture and sagittal balance during walking in adult spinal deformity patients. Spine (Phila Pa 1976) 2017;42:E25-30. [Crossref] [PubMed]
- Berg K, Wood-Dauphine S, Williams JI, et al. Measuring balance in the elderly: preliminary development of an instrument. Physiotherapy Canada 1989;41:304-11. [Crossref]
- Miyata K, Kaizu Y, Usuda S. Prediction of falling risk after discharge in ambulatory stroke or history of fracture patients using Balance Evaluation Systems Test (BESTest). J Phys Ther Sci 2018;30:514-9. [Crossref] [PubMed]
- Glassman SD, Coseo MP, Carreon LY. Sagittal balance is more than just alignment: why PJK remains an unresolved problem. Scoliosis Spinal Disord 2016;11:1. [Crossref] [PubMed]
- Yagi M, Ohne H, Kaneko S, et al. Does corrective spine surgery improve the standing balance in patients with adult spinal deformity? Spine J 2018;18:36-43. [Crossref] [PubMed]
- Arima H, Glassman SD, Dimar JR, et al. Neurologic comorbidities predict proximal junctional failure in adult spinal deformity. Spine Deformity 2018;6:576-86. [Crossref] [PubMed]
- Dubousset J. Three-dimensional analysis of the scoliotic deformity. In: Weinstein SL, Weinstein S. editors. The Pediatric Spine: Principles and Practice. New York: Raven Press, 1994:479-96.
- Le Berre M, Guyot M, Agnani O, et al. Clinical balance tests, proprioceptive system and adolescent idiopathic scoliosis. Eur Spine J 2017;26:1638-44. [Crossref] [PubMed]
- Sinaki M, Brey RH, Hughes CA, et al. Balance disorder and increased risk of falls in osteoporosis and kyphosis: significance of kyphotic posture and muscle strength. Osteoporos Int 2005;16:1004-10. [Crossref] [PubMed]
- Babat LB, McLain RF, Bingaman W, et al. Spinal surgery in patients with Parkinson’s disease: construct failure and progressive deformity. Spine (Phila Pa 1976) 2004;29:2006-12. [Crossref] [PubMed]
- Assaiante C, Barlaam F, Cignetti F, et al. Body schema building during childhood and adolescence: a neurosen- sory approach. Neurophysiol Clin 2014;44:3-12. [Crossref] [PubMed]
- Downs S, Marquez J, Chiarelli P. The Berg balance scale has high intra- and inter-rater reliability but absolute reliability varies across the scale: a systematic review. J Physiother 2013;59:93-9. [Crossref] [PubMed]
- Moke L, Severijns P, Schelfaut S, et al. Performance on balance evaluation systems test (BESTest) impacts health-related quality of life in adult spinal deformity patients. Spine (Phila Pa 1976) 2018;43:637-46. [Crossref] [PubMed]


