Degree of satisfaction following full-endoscopic cervical foraminotomy
Introduction
Cervical radiculopathy (CR) causes radiating pain to the arm and disability in activities of daily life. Compression of the cervical nerve roots results in CR. Compression of the nerve root may be caused by impingement due to disc herniation or bony osteophytes. The symptoms of CR are typically presented as unilateral arm pain and upper back pain around the scapula and, sometimes, motor weakness of the arm (1,2). A population-based study estimated that the annual incidence of CR is 107.3 per 100,000 for males and 63.5 per 100,000 for females (3). Some studies have demonstrated that the natural history of CR is on benign course (3,4), and approximately 90% of patients experience improvements of the symptoms with conservative treatment (5,6). However, the rest of the patients with CR do not respond to conservative therapy and require surgery.
Foraminotomy by a posterior approach has been reported to be effective for the treatment of CR, as well as anterior cervical decompression and fusion or disc replacement (1,2,7). Worldwide, foraminotomy has been performed by an open approach or minimally invasive approach using a microscope or endoscope. A review of the literature has revealed that both the open and minimally invasive approach yield good clinical results, although the minimally invasive approach is superior to the open approach in terms of blood loss, operation time, and duration of hospital stays (2,8-10). Since the introduction of microendoscopic cervical foraminotomy (MECF) in 2002 (11), we have performed MECF for patients with CR for fourteen years. The diameter of the endoscope used for MECF was 16 mm. We had previously reported good clinical results of MECF (12). Following MECF, full-endoscopic cervical foraminotomy (FECF) had been developed and first reported in 2007 (13). The diameter of the endoscope for FECF is 7 mm. We have adopted FECF in our hospital since 2016. The purpose of this study was to evaluate the degree of satisfaction following FECF for CR.
Methods
Subjects
We diagnosed CR using physical findings and findings of radiological examinations such as radiography, magnetic resonance imaging, and computed tomography. Patients whose symptoms do not sufficiently improve in spite of a 3-month course of conservative therapy proceeded to FECF. All operations were performed at Iwai Orthopaedic Medical Hospital. The data of 109 consecutive patients who underwent FECF between October 2016 and April 2019 were collected.
Background information of the patients, including age and sex, were collected. Preoperative diagnosis, level of the operated foramen, operated side, operation time, estimated blood loss, complications related to the operation, and occurrence of reoperation in 3 months were obtained from medical records. The preoperative diagnosis was based mainly on magnetic resonance imaging and computed tomography. If the main factor of nerve root compression was disc herniation without any bony stenosis, we classified it as cervical disc herniation. If the main factors were bones such as osteophytes of the vertebral body and/or ossification of the posterior longitudinal ligament (OPLL), we classified as cervical spondylotic radiculopathy and OPLL, respectively. If motor weakness of the upper extremity with no radiating pain accompanied with spondylosis was noted, we classified it as cervical spondylotic amyotrophy. If there was motor weakness with any degree of pain, we classified the case as the aforementioned three diagnoses according to the main cause of nerve root compression. The numerical rating scale (NRS) score for the arm was assessed preoperatively and postoperatively at the time of discharge to evaluate the degree of pain. The NRS score was obtained by nurses or physical therapists. The satisfaction score was also recorded at discharge from the hospital and at 3 months after the operation. The satisfaction score was then obtained by a medical clerk using a ten-level rating scale similar to the NRS. The associations of the satisfaction score with the pre- and postoperative NRS scores for the arm were evaluated.
Operation and postoperative care
Patients were placed in a prone position under general anesthesia. An 8-mm longitudinal skin incision was done approximately 15 mm lateral to the midline of the vertebral level operated. A 7-mm-diameter outer sheath was placed on the cervical lamina after splitting paravertebral muscles. Under full-endoscopic assistance with continuous irrigation, the caudal side of the inferior process of the upper vertebra and the cranial side of the superior process were resected using surgical airtome. Subsequently, exposure of the whole nerve root circumference was carefully performed. When a herniated disc was identified without much bleeding and any traumatic procedure to the nerve root, we resected the herniated disc. When it was done with bleeding or any traumatic procedure to the nerve root, we did not resect the herniated disc. Skin closure was performed without a drainage tube. The patients were allowed to walk at day one after surgery without any cervical orthoses.
Statistical methods
Descriptive statistics are presented as means and standard deviations or frequencies and percentages. The differences in the NRS score and the satisfaction score between the two time points were evaluated using Student’s t-test. Statistical analysis was performed using the JMP 14.2 software program (SAS Institute, Cary, NC, USA). A P value <0.05 was considered significant.
Results
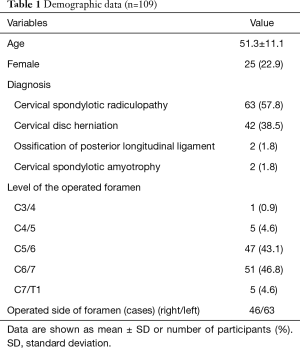
In total, 109 patients were included in this study. The age was 51.3±11.1 years; 22.9% were female and 77.1% were male. The patient characteristics including details of preoperative diagnosis are shown in Table 1. The cervical level most frequently operated on was C6/7, followed by C5/6. The duration of hospital stay was 4.7±1.0 days.
Full table
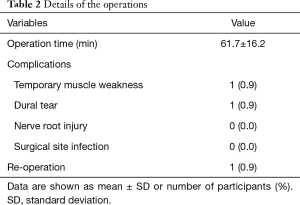
Details of the operations are shown in Table 2. Herniotomy in addition to foraminotomy was performed in six cases. The operation time was 61.7±16.2 minutes. The estimated blood loss was 0 to 10 mg in all cases. One case exhibited temporary postoperative muscle weakness, although the patient recovered within 1 year. There was one case of dural tear. Because the tear was like a pin hole, additional procedures were not performed. The tear was left as it was, however, cerebrospinal fluid leakage did not occur after the operation. There was no cases of nerve root injury and surgical site infection. The overall complication rate was 1.8%. There was one case of reoperation by MECF in 3 months due to insufficient improvement.
Full table
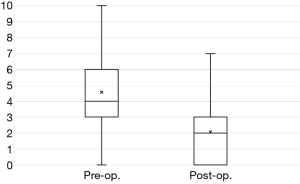
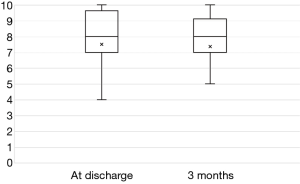
The preoperative NRS scores for the arm of 4.6±2.1 improved significantly postoperatively to 2.1±2.0 (P<0.0001) (Figure 1). The mean satisfaction score at discharge was 7.5±2.5. The mean score at 3 months after the operations was 7.4±2.8, which was not significantly improved over the score at discharge (P=0.8102) (Figure 2).
Discussion
The patients’ backgrounds were similar to that of our previous study about MECF (12). A result that CR was more popular in males than in females matched to a systematic review (14). The mean operation time of 61.7 minutes was almost the same as that of 57.7 minutes for one level in our previous MECF study (12). The operating time and minimal bleeding characterize the minimal invasiveness of FECF. The low complication rate in the current study of 1.8% was lower than that reported in a systematic review (5.8%) (15). Temporary muscle weakness was present in only one case (0.9%), and recovered within 1 year, while in our MECF series, 7% of patients had temporary muscle weakness (12). Dural tear occurred in one case (0.9%), and there was no nerve root injury, which was similar to our MECF series (12). A systematic review showed that transient nerve root palsy was present more frequently in FECF (4.5%) than in MECF (1.5%), and the difference was significant (15). The difference may result from the limited working space in FECF. The limited space could result in traumatic retraction of a nerve root. It also showed that the incidence of dural tear in FECF (1.5%) and that of superficial wound infection in FECF (2.2%) (15) were higher than those in the current study. The reoperation rate of 0.9% in our study was lower than that in the systematic review with 4.8% (14). In addition, there was a report dealing with osseous foraminal stenosis showing a reoperation rate of 18.6% (16). The follow-up period of only 3 months in the current study was short, whereas previous articles had follow-up periods of more than one year (14,16). The reoperation rate of our study due to recurrences of symptoms may increase with longer follow-up.
We compared the NRS scores of the arm in the current study for FECF with that for MECF in our previous study (12). The mean preoperative NRS score for FECF of 4.6 was lower than that for MECF of 5.4. The mean postoperative NRS score for FECF was 2.1 equivalent to that for MECF of 2.0 (12). The minimal clinically important difference of the NRS for the arm was reported as 4.1 (17). The difference between the pre- and postoperative NRS score was smaller than the value of 4.1. The reason could be that the preoperative NRS score of the patients of the current study was not much high, which indicated that they did not suffer much severely. A limitation of the comparison was the timing of the evaluation. The postoperative NRS score was evaluated at discharge for FECF, while it was one year after the operation for MECF. The score for FECF could change one year after the operation.
The mean satisfaction score for FECF at discharge was 7.5 of 10, remaining the same after 3 months. In our previous study for MECF, postoperative satisfaction was assessed using a seven-level rating scale (12). We hypothesized quasi-scores for each item in order to compare with the satisfaction score in the current study: extremely satisfied as 10, very satisfied as 9, satisfied as 7, borderline as 5, unsatisfied as 3, very unsatisfied as 1, and extremely unsatisfied as 0. As a result, the quasi-score of satisfaction for MECF was 7.9±2.4, which corresponded to the score for FECF in the current study. A limitation of the comparison was also the timing of the evaluation, which was the same as that for the postoperative NRS score. The satisfaction score was evaluated at discharge and 3 months after the operation for FECF, while it was one year after the operation for MECF. The score for FECF could change with regard to the potential change of postoperative NRS score as time goes by. A systematic review showed that the clinical success rate was 93.6% for FECF and 89.9% for MECF, respectively, without significant difference (14). However, the definition of the clinical success was not specified. Results should therefore be interpreted with caution.
There were some limitations to the current study. First, the follow-up period was short. The outcomes may change with longer follow-up. Second, outcome measurement scores other than the NRS scores were not collected. Although a previous study reported that the neck disability index is the most valid and responsive measure of the improvement in pain and disability after cervical spine surgery (18), we did not evaluate it. Third, there was selection bias among our patients. Since therapy for CR is usually conservative, an indication for the operation is mainly determined by the willingness of the patient. The patients who were included in the current study could have a tendency to be willing to undergo surgery.
Conclusions
The degree of satisfaction following FECF for CR was high and preferable 3 months after the operation.
Acknowledgments
We would like to thank Ai Ido, who is a medical clerk at the hospital, for collecting the data.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Hisashi Koga and Alf Giese) for the series “Full-endoscopic Spine Surgery” published in Journal of Spine Surgery. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss.2020.01.02). The series “Full-endoscopic Spine Surgery” was commissioned by the editorial office without any funding or sponsorship. HK served as the unpaid Guest Editor of the series and serves as an unpaid editorial member of Journal of Spine Surgery from October 2018 to October 2020. The other authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the medical ethics review board of Iwai Orthopaedic Medical Hospital. Written informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Woods BI, Hilibrand AS. Cervical radiculopathy: epidemiology, etiology, diagnosis, and treatment. J Spinal Disord Tech 2015;28:E251-9. [Crossref] [PubMed]
- Iyer S, Kim HJ. Cervical radiculopathy. Curr Rev Musculoskelet Med 2016;9:272-80. [Crossref] [PubMed]
- Radhakrishnan K, Litchy WJ, O'Fallon WM, et al. Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain 1994;117:325-35. [Crossref] [PubMed]
- Sampath P, Bendebba M, Davis JD, et al. Outcome in patients with cervical radiculopathy. Prospective, multicenter study with independent clinical review. Spine (Phila Pa 1976) 1999;24:591-7. [Crossref] [PubMed]
- Rhee JM, Yoon T, Riew KD. Cervical radiculopathy. J Am Acad Orthop Surg 2007;15:486-94. [Crossref] [PubMed]
- Saal JS, Saal JA, Yurth EF. Nonoperative management of herniated cervical intervertebral disc with radiculopathy. Spine (Phila Pa 1976) 1996;21:1877-83. [Crossref] [PubMed]
- Selvanathan SK, Beagrie C, Thomson S, et al. Anterior cervical discectomy and fusion versus posterior cervical foraminotomy in the treatment of brachialgia: the Leeds spinal unit experience (2008-2013). Acta Neurochir (Wien) 2015;157:1595-600. [Crossref] [PubMed]
- McAnany SJ, Kim JS, Overley SC, et al. A meta-analysis of cervical foraminotomy: open versus minimally-invasive techniques. Spine J 2015;15:849-56. [Crossref] [PubMed]
- Dodwad SJ, Dodwad SN, Prasarn ML, et al. Posterior cervical foraminotomy: indications, technique, and outcomes. Clin Spine Surg 2016;29:177-85. [Crossref] [PubMed]
- Song Z, Zhang Z, Hao J, et al. Microsurgery or open cervical foraminotomy for cervical radiculopathy? A systematic review. Int Orthop 2016;40:1335-43. [Crossref] [PubMed]
- Fessler RG, Khoo LT. Minimally invasive cervical microendoscopic foraminotomy: an initial clinical experience. Neurosurgery 2002;51:S37-45. [Crossref] [PubMed]
- Tonosu J, Inanami H, Oka H, et al. Factors related to subjective satisfaction following microendoscopic foraminotomy for cervical radiculopathy. BMC Musculoskelet Disord 2018;19:30. [Crossref] [PubMed]
- Ruetten S, Komp M, Merk H, et al. A new full-endoscopic technique for cervical posterior foraminotomy in the treatment of lateral disc herniations using 6.9-mm endoscopes: prospective 2-year results of 87 patients. Minim Invasive Neurosurg 2007;50:219-26. [Crossref] [PubMed]
- Wu PF, Li YW, Wang B, et al. Posterior cervical foraminotomy via full-endoscopic versus microendoscopic approach for radiculopathy: A systematic review and meta-analysis. Pain Physician 2019;22:41-52. [PubMed]
- Wu PF, Liu BH, Wang B, et al. Complications of full-endoscopic versus microendoscopic foraminotomy for cervical radiculopathy: A systematic review and meta-analysis. World Neurosurg 2018;114:217-27. [Crossref] [PubMed]
- Oertel JM, Philipps M, Burkhardt BW. Endoscopic Posterior Cervical Foraminotomy as a Treatment for Osseous Foraminal Stenosis. World Neurosurg 2016;91:50-7. [Crossref] [PubMed]
- Parker SL, Godil SS, Shau DN, et al. Assessment of the minimum clinically important difference in pain, disability, and quality of life after anterior cervical discectomy and fusion: clinical article. J Neurosurg Spine 2013;18:154-60. [Crossref] [PubMed]
- Godil SS, Parker SL, Zuckerman SL, et al. Accurately measuring the quality and effectiveness of cervical spine surgery in registry efforts: determining the most valid and responsive instruments. Spine J 2015;15:1203-9. [Crossref] [PubMed]