Comparison of outcomes following minimally invasive and open posterior cervical foraminotomy: description of minimally invasive technique and review of literature
Introduction
Cervical radiculopathy is a clinical condition resulting from compression of cervical nerve roots (1). Patients can present with a wide range of clinical manifestations including radiating pain, sensory deficits, motor deficits, diminished reflexes, or any combination of the above (1). Cases of cervical radiculopathy that have failed non-operative management can be treated with multiple surgical interventions including from both anterior and posterior approaches. Originally described in two cadaveric studies in 2000, minimally invasive posterior cervical foraminotomy (MIS-PCF) has gained significant traction as a minimally invasive treatment for lateral spinal canal pathology causing radiculopathy (2,3). Although initial case series focused on minimally invasive endoscopic approaches, the surgeons armamentarium has since expanded to include microscopic and percutaneous endoscopic (full-endoscopic) approaches (4-7).
Several case series and technique papers have been published describing endoscopic/microscopic MIS-PCF (MIS-PCF) and percutaneous endoscopic (full-endoscopic) posterior cervical foraminotomy (FE-PCF) (8-32). There are, however, very few studies directly comparing minimally invasive to open posterior cervical foraminotomy or MIS-PCF to percutaneous endoscopic(full-endoscopic) posterior cervical foraminotomy. Additionally, the majority of previously published meta-analyses include non-comparative studies and instead use pooled analysis from multiple single-arm case series (33-35). This study includes a description of the current technique employed by the senior author to perform a MIS-PCF and a systematic review of literature and analysis of clinical studies directly comparing outcomes between MIS-PCF and open posterior cervical foraminotomy and between MIS-PCF and FE-PCF. Studies were evaluated for differences in operative/hospital admission metrics, patient-reported outcomes including visual analog scale (VAS) and neck disability index (NDI), complications, and reoperation.
Methods
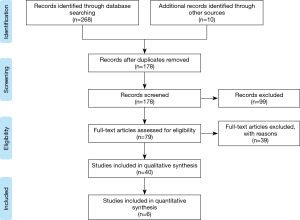
This study includes a systematic review of literature conducted based on the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement using PubMed, the Cochrane Library, Scopus, and included citations to identify clinical studies comparing MIS-PCF to open posterior cervical foraminotomy or percutaneous endoscopic (full-endoscopic) posterior cervical foraminotomy (FE-PCF). Specific MeSH terms and key words including “cervical radiculopathy” “foraminotomy” “posterior foraminotomy” “minimally invasive cervical foraminotomy” “percutaneous endoscopic foraminotomy” and “full endoscopic foraminotomy” were used to identify studies of interest. Additional manual searches through cited references were performed. Randomized controlled trials, prospective/retrospective cohort and case-control studies were included in further analysis. Non-English publications, editorials, conference abstracts, errata, book chapters, systematic reviews, meta-analyses, case reports, and case series were excluded. Studies that reported outcomes of continuous variables as medians were excluded. Studies were evaluated for differences in operative/hospital admission metrics, patient-reported outcomes (VAS, NDI), complications, and reoperation.
Surgical technique
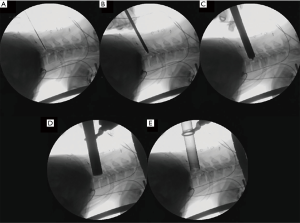
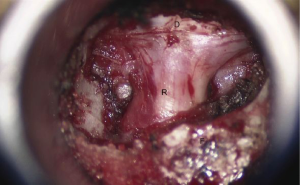
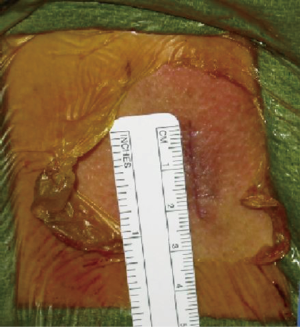
Following intubation, the patient is placed in Gardner-Wells tongs and placed prone on the surgical table. A radiolucent Jackson frame is used, and the patients head is placed in a slightly flexed position (Figure 1). The C-arm is placed beneath or anterior to the patient. An initial image is acquired to confirm visualization of the desired level and to plan the initial entry point. The surgical area is shaved, prepared, and draped in the usual fashion. Preoperative antibiotics are administered. Prior to incision the operative level is re-confirmed on lateral fluoroscopy by placing a Kirschner (K)-wire or another long radiopaque instrument over the lateral side of the patient’s neck. Following an injection of local anesthetic, a 2-cm longitudinal incision is made 1.5 cm lateral of the midline. The K-wire is advanced carefully though the musculature under fluoroscopic guidance and docked at the inferomedial edge of the rostral lateral mass of the level of interest. The cervical fascia is incised, not exceeding the length of the skin incision, and the tubular retractors are serially inserted (Figure 2). The final tubular retractor, usually 16-mm or 18-mm in diameter, is placed over the dilators and fixed into place using a table-mounted flexible retractor arm. The dilators are then removed and the microscope is brought into position. Monopolar cautery is used to clear the remaining soft tissue from the lamina and lateral mass of interest. The laminotomy and foraminotomy are performed using a high-speed drill and Kerrison rongeur. Once the laminotomy is complete, the ligamentum flavum can be removed from medial to lateral to identify the proximal nerve root and lateral dura. Bony resection of the medial facet is carried out to expose the proximal foraminal course of the nerve root, however, careful attention should be paid to not resect greater than 50% of the facet. This limits the risk of iatrogenic instability. After the root is well visualized (Figure 3) a fine-angled dissector can be used to palpate ventral to the nerve root and confirm the root is adequately decompressed. To allow removal of any osteophytes or disc fragments additional drilling of the superomedial quadrant of the caudal pedicle can be carried out to allow greater access without excessive retraction of the nerve root. The foramen is inspected one last time for adequacy of decompression prior to hemostasis, antibiotic-impregnated irrigation, and multi-layer closure (Figure 4).

Results
In total 178 abstracts were reviewed of which 99 were excluded; 79 full text articles were assessed of which 39 were excluded. Several articles were excluded if they did not include minimally invasive procedures, if it was unclear from the manuscript whether or not minimally invasive techniques were performed, or if they included open or “mini-open” cervical foraminotomies within a posterior cervical cohort (36-46). Articles were excluded if they included laser-mediated decompressions (47-49). or if they included anterior endoscopic approaches (50). Overall 5 comparative studies, including one randomized controlled trial, were included in analysis comparing open to MIS-PCF (5,51-54). One study was included in analysis that compared minimally invasive tubular retractor based posterior cervical foraminotomy to percutaneous endoscopic cervical foraminotomy and discectomy (“full-endoscopic”) (55). A flow chart of study inclusion and exclusion is shown in Figure 5 (56).
Five studies were included comparing minimally invasive cervical foraminotomy to open cervical foraminotomy (5,51-54). Fessler et al. included a prospectively collected, retrospectively analyzed cohort series whereas Kim et al. (in 2009) consisted of a randomized controlled trial (5,51). The remainder of series were retrospective cohort series (Table 1).
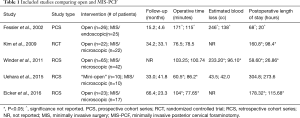
Full table
Average operative time was reported in 5 studies which ranged from 60.5 to 171 minutes in the open group and 77.65 to 115 minutes in the minimally invasive group (5,51-54). Eicker et al. was the only study to find a statistically significant decrease in operative time in the MIS group (53).Kim et al. (in 2009) and Winder et al. failed to find a statistically significant difference in operative time between the two groups, and Uehara et al. found operative time to be significantly increased in the minimally invasive tubular retractor group (51,52,54). Mean intraoperative estimated blood loss was reported in 3 studies which ranged from 43.5 to 246 cc in the open group and 42 to 138 cc in the MIS group (5,52,54). Winder et al. was the only included comparative study to show a statistically significant decrease in estimated blood loss in the MIS group (52). Five studies reported postoperative length of stay which ranged from 58.6 to 304.8 hours in the open group and 20 to 273.6 hours in the MIS group (5,51-54). Eicker et al., Winder et al., and Kim et al. (in 2009) all found significant decreases in postoperative length of stay in patients undergoing MIS posterior cervical foraminotomy (51-53) (Table 1). Regarding postoperative analgesia, Winder et al. and Eicker et al. found significantly decreased dosages of pain medication in the minimally invasive group, whereas Kim et al. (in 2009) found that patients in the minimally invasive group had a significantly decreased duration of pain medication usage (51-53). Both Kim et al. (in 2009) and Eicker et al. found significantly decreased skin incision lengths in the MIS group (51,53).
Regarding patient reported outcomes (PRO’s), Kim et al. (in 2009) found no significant differences in VAS-A scoring however VAS-N was significantly increased in the open group from 1 day to 4 weeks postoperatively. There was no significant difference in VAS-N from 3 to 24 months postoperatively (51). Eicker et al. reported VAS-N was significantly reduced in the minimally invasive group compared to the open group on the first postoperative day and day of discharge however was not significant at 6 weeks postoperatively. VAS-A scores were not significantly different between groups (53). Uehara et al. found no significant differences in PRO’s (NDI, VAS-A, VAS-N) postoperatively (54). Regarding complications, Fessler et al. reported three overall complications in the minimally invasive group including two CSF leaks and one partial thickness dural violation (5). There were no reported complications in the open group. Kim et al. (in 2009) reported no complications in either group (51). Total complications were not statistically different between groups in Winder et al. and were not specified by group in Eicker et al. (52,53). Three of five studies did not include reoperations (51,52,54). Fessler et al. reported no cases of reoperations within either cohort and Eicker et al. did not specify reoperations by group (5,53).
One study was included in analysis that compared minimally invasive tubular retractor based posterior cervical foraminotomy (MIS-PCF) to percutaneous endoscopic (full endoscopic) cervical foraminotomy (FE-PCF). Kim et al. (in 2015), a retrospective cohort study, compared 24 consecutive patients who underwent percutaneous endoscopic cervical foraminotomy and discectomy to 34 patients who underwent minimally invasive tubular assisted microscopic cervical foraminotomy (55). Mean follow up times were not reported although all patients were followed for >2 years. Postoperatively at 24 months, the mean NDI and VAS-N were significantly lower after percutaneous endoscopic cervical foraminotomy than minimally invasive tubular assisted microscopic cervical foraminotomy. There was however no significant change in VAS-A between the two groups.
Discussion
Five studies were included comparing minimally invasive cervical foraminotomy to open cervical foraminotomy (5,51-54). All of these studies were retrospective cohorts except Kim et al. (in 2009) and Fessler et al. All five of the studies had significant limitations including small sample sizes and relatively short follow-up periods. There was significant heterogeneity in the study designs. Four of the five studies involved minimally invasive tubular assisted microscopic cervical foraminotomy, however Fessler et al. included an endoscopic series in the minimally invasive group. Fessler et al. also contained an operative technique change as the first 12 cases in the minimally invasive group were done in prone position and the final 13 cases were done in sitting position. Uehara et al. further compared minimally invasive tubular assisted microscopic cervical foraminotomy to a “mini-open” retractor based foraminotomy. Given the significant heterogeneity between studies a meta-analysis was not performed.
Operative time was found to be decreased in Eicker et al. and Fessler et al., however, a level of significance was not reported in the latter study (5,53). Kim et al. (in 2009), and Winder et al. failed to find a statistically significant difference in operative time between the two groups, and Uehara et al. found operative time to be significantly increased in the minimally invasive group (51,52,54). This discrepancy may be related to an increased learning curve that occurs with using the tubular retractor or endoscopic system leading to increased operative time. Fessler et al. found decreased operative blood loss and surgical duration when switching from prone to sitting position (5). None of the other studies were performed in the sitting position which may have led to increased operative time compared to open procedures.
Of only two studies that analyzed estimated blood loss for statistical significance, Winder et al. was the only study to show MIS-PCF had significantly lower blood loss than Open-PCF (52). Uehara et al. did report decreased blood loss in the MIS group however it was not statistically significant. This may be related to the open cohort in Uehara et al. actually being a “mini-open” cohort and thus the blood loss may be closer to a MIS approach than an open approach (54). Kim et al. (in 2009), Winder et al., and Eicker et al. all reported statistically significant decreases in hospital length of stay and postoperative analgesic usage in the minimally invasive group (51-53). Regarding PRO’s both Kim et al. (in 2009) and Eicker et al. reported significantly increased VAS-N scores postoperatively in patients undergoing open cervical foraminotomies. Both studies also reported that the differences lost statistical significance with longer follow-up. This is likely related to a longer incision and increased muscle dissection in the open approach. There was not enough data included in the above studies to suggest a difference in complication rate and reoperation rate between minimally invasive and open cervical foraminotomy.
This analysis has some advantages and similar limitations over previously published meta-analyses. McAnany et al. included 8 studies in meta-analysis however only one study, Kim et al. (in 2009), was comparative in nature (33). The remainder of studies were either case series of minimally invasive (both endoscopic and microscopic) or open procedures which were pooled for analysis. The meta-analysis found that there was no statistically significant difference in the pooled clinical success rate for either procedure (33). Clark et al. included 18 publications of which 3 were directly comparative [Kim et al. (in 2009), Fessler et al., Winder et al.] (57). Given the degree of heterogeneity the authors did not perform a meta-analysis. Similar to this analysis, in data aggregated from the included publications they found that patients undergoing minimally invasive cervical foraminotomy have less inpatient analgesic use, and shorter hospital stays. Aggregate data from Clark et al. also showed patients undergoing minimally invasive cervical foraminotomy have lower blood loss and shorter surgical time compared with patients undergoing open procedures (57).
Only one study was found in systematic review that compared minimally invasive tubular retractor based posterior cervical foraminotomy to percutaneous endoscopic cervical foraminotomy and discectomy and thus meta-analysis was not able to be performed. Although the study was limited by short follow-up and low sample size, the authors showed that percutaneous endoscopic cervical foraminotomy had significantly lower mean NDI and VAS-N scores postoperatively (55). It is unclear why the scores would be different between the two procedures. According to the surgical methods the difference in the incisions is 1.2 cm and muscular dissection should be minimized in both procedures. Postoperative differences would likely normalize by 24 months as they were in the minimally invasive vs open foraminotomy studies. Two meta-analyses have been done that compare MIS-PCF to percutaneous endoscopic cervical foraminotomy (34,35). Both studies include Kim et al. (in 2015) as the only directly comparative study within their meta-analysis. Wu et al. (in 2018) evaluated total complications, complications for single level radiculopathy, dural tear, transient root palsy, and superficial wound infection and found only a statistically increased rate of transient root palsy in the full-endoscopic group (35). The meta-analysis was however significantly limited by heterogeneity, included only one directly comparative study, and included multiple series that were excluded from this analysis including a case series of patients undergoing open cervical foraminotomy (35,46). Wu et al. (in 2019) compared the clinical success rate, total complication rate, and reoperation rate between MIS-PCF and percutaneous endoscopic cervical foraminotomy and found no statistically significant difference (34). It is limited by many of the same limitations as the previous study.
Limitations
There are several limitations to this study. Following systematic review only 6 studies were included that met inclusion/exclusion criteria. Although all studies were directly comparative in nature there were several key differences between the studies that limited the ability to perform meta-analysis. A majority of studies did not include or did not stratify reoperation or complications. Follow-up time and cohort size were additionally limited. Regarding studies comparing minimally invasive to percutaneous (full-endoscopic) approaches only one directly comparative paper was found.
Conclusions
Direct comparative studies between MIS-PCF and open cervical foraminotomy are limited in number. Although, there is a significant heterogeneity in studies comparing open and MIS-PCF there appears to be a trend of decreased hospital length of stay and postoperative analgesic usage in the minimally invasive cohort. There is not enough data currently to suggest a difference in complication rate and reoperation rate between minimally invasive and open cervical foraminotomy. There is not enough data to currently compare MIS-PCF and FE-PCF in a meaningful manner.
Acknowledgments
We would like to acknowledge the Rush University Department of Neurological Science Research team for their help in this paper.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Lee A. Tan and Ilyas S. Aleem) for the series “Advanced Techniques in Complex Cervical Spine Surgery” published in Journal of Spine Surgery. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: The series “Advanced Techniques in Complex Cervical Spine Surgery” was commissioned by the editorial office without any funding or sponsorship. Dr. O’Toole is a consultant for Globus Medical, RTI Surgical and the Food and Drug Administration, and receives royalties from Globus Medical and RTI Surgical. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Iyer S, Kim HJ. Cervical radiculopathy. Current Reviews in Musculoskeletal Medicine 2016;9:272-80. [Crossref] [PubMed]
- Burke TG, Caputy A. Microendoscopic posterior cervical foraminotomy: a cadaveric model and clinical application for cervical radiculopathy. J Neurosurg 2000;93:126-9. [PubMed]
- Roh SW, Kim DH, Cardoso AC, et al. Endoscopic foraminotomy using MED system in cadaveric specimens. Spine (Phila Pa 1976) 2000;25:260-4. [Crossref] [PubMed]
- Adamson TE. Microendoscopic posterior cervical laminoforaminotomy for unilateral radiculopathy: results of a new technique in 100 cases. J Neurosurg 2001;95:51-7. [PubMed]
- Fessler RG, Khoo LT. Minimally Invasive Cervical Microendoscopic Foraminotomy: An Initial Clinical Experience. Neurosurgery 2002;51:S37-45. [Crossref] [PubMed]
- Hilton DL Jr. Minimally invasive tubular access for posterior cervical foraminotomy with three-dimensional microscopic visualization and localization with anterior/posterior imaging. Spine J 2007;7:154-8. [Crossref] [PubMed]
- Ruetten S, Komp M, Merk H, et al. A new full-endoscopic technique for cervical posterior foraminotomy in the treatment of lateral disc herniations using 6.9-mm endoscopes: prospective 2-year results of 87 patients. Minim Invasive Neurosurg 2007;50:219-26. [Crossref] [PubMed]
- O'Toole JE, Sheikh H, Eichholz KM, et al. Endoscopic posterior cervical foraminotomy and discectomy. Neurosurg Clin N Am 2006;17:411-22. [Crossref] [PubMed]
- Gala VC, O'Toole JE, Voyadzis JM, et al. Posterior minimally invasive approaches for the cervical spine. Orthop Clin North Am 2007;38:339-49. [Crossref] [PubMed]
- Holly LT, Moftakhar P, Khoo LT, et al. Minimally invasive 2-level posterior cervical foraminotomy: preliminary clinical results. J Spinal Disord Tech 2007;20:20-4. [Crossref] [PubMed]
- Santiago P, Fessler RG. Minimally invasive surgery for the management of cervical spondylosis. Neurosurgery 2007;60:S160-5. [Crossref] [PubMed]
- Branch BC, Hilton DL Jr, Watts C. Minimally invasive tubular access for posterior cervical foraminotomy. Surg Neurol Int 2015;6:81. [Crossref] [PubMed]
- Won SJ, Kim CH, Chung CK, et al. Clinical Outcomes of Single-level Posterior Percutaneous Endoscopic Cervical Foraminotomy for Patients with Less Cervical Lordosis. Journal of Minimally Invasive Spine Surgery and Technique 2016;1:11-7. [Crossref]
- Won S, Kim CH, Chung CK, et al. Comparison of Cervical Sagittal Alignment and Kinematics after Posterior Full-endoscopic Cervical Foraminotomy and Discectomy According to Preoperative Cervical Alignment. Pain Physician 2017;20:77-87. [PubMed]
- Skovrlj B, Gologorsky Y, Haque R, et al. Complications, outcomes, and need for fusion after minimally invasive posterior cervical foraminotomy and microdiscectomy. Spine J 2014;14:2405-11. [Crossref] [PubMed]
- Kwon Y-J. Long-Term Clinical and Radiologic Outcomes of Minimally Invasive Posterior Cervical Foraminotomy. 2014;56:224.
- Peto I, Scheiwe C, Kogias E, et al. Minimally Invasive Posterior Cervical Foraminotomy: Freiburg Experience With 34 Patients. Clin Spine Surg 2017;30:E1419-25. [Crossref] [PubMed]
- Oertel JM, Philipps M, Burkhardt BW. Endoscopic Posterior Cervical Foraminotomy as a Treatment for Osseous Foraminal Stenosis. World Neurosurg 2016;91:50-7. [Crossref] [PubMed]
- Youn MS, Shon MH, Seong YJ, et al. Clinical and radiological outcomes of two-level endoscopic posterior cervical foraminotomy. Eur Spine J 2017;26:2450-8. [Crossref] [PubMed]
- Burkhardt BW, Muller S, Oertel JM. Influence of Prior Cervical Surgery on Surgical Outcome of Endoscopic Posterior Cervical Foraminotomy for Osseous Foraminal Stenosis. World Neurosurg 2016;95:14-21. [Crossref] [PubMed]
- Dahdaleh NS, Wong AP, Smith ZA, et al. Microendoscopic decompression for cervical spondylotic myelopathy. Neurosurg Focus 2013;35:E8. [Crossref] [PubMed]
- Kim CH, Shin KH, Chung CK, et al. Changes in cervical sagittal alignment after single-level posterior percutaneous endoscopic cervical diskectomy. Global Spine J 2015;5:31-8. [Crossref] [PubMed]
- McAnany SJ, Qureshi SA. Minimally invasive cervical foraminotomy. JBJS Essent Surg Tech 2016;6:e23. [Crossref] [PubMed]
- Ross DA, Bridges KJ. Technique of Minimally Invasive Cervical Foraminotomy. Operative Neurosurgery 2017;13:693-701. [Crossref] [PubMed]
- Ye ZY, Kong WJ, Xin ZJ, et al. Clinical Observation of Posterior Percutaneous Full-Endoscopic Cervical Foraminotomy as a Treatment for Osseous Foraminal Stenosis. World Neurosurgery 2017;106:945-52. [Crossref] [PubMed]
- Gerard CS, O'Toole JE. Current techniques in the management of cervical myelopathy and radiculopathy. Neurosurg Clin N Am 2014;25:261-70. [Crossref] [PubMed]
- Ahn J, Tabaraee E, Bohl DD, et al. Minimally invasive posterior cervical foraminotomy. J Spinal Disord Tech 2015;28:295-7. [Crossref] [PubMed]
- Ryan J, McGowan JE, Voyadzis JM. Treating cervical radiculopathy for a one-level disc herniation using a posterior foraminotomy. Semin Spine Surg 2014;26:148-53. [Crossref]
- Shih P, Slimack NP, Fessler RG. Cervical Microendoscopic Discectomy and Decompression. Semin Spine Surg 2011;23:14-9. [Crossref]
- Wagner R, Telfeian AE, Iprenburg M, et al. Minimally invasive fully endoscopic two-level posterior cervical foraminotomy: technical note. J Spine Surg 2017;3:238-42. [Crossref] [PubMed]
- Lee YS, Kim YB, Park SW, et al. Preservation of motion at the surgical level after minimally invasive posterior cervical foraminotomy. J Korean Neurosurg Soc 2017;60:433-40. [Crossref] [PubMed]
- Zhang C, Wu J, Xu C, et al. Minimally Invasive Full-Endoscopic Posterior Cervical Foraminotomy Assisted by O-Arm-Based Navigation. Pain Physician 2018;21:E215-23. [PubMed]
- McAnany SJ, Kim JS, Overley SC, et al. A meta-analysis of cervical foraminotomy: open versus minimally-invasive techniques. Spine J 2015;15:849-56. [Crossref] [PubMed]
- Wu PF, Li YW, Wang B, et al. Posterior Cervical Foraminotomy Via Full-Endoscopic Versus Microendoscopic Approach for Radiculopathy: A Systematic Review and Meta-analysis. Pain Physician 2019;22:41-52. [PubMed]
- Wu PF, Liu BH, Wang B, et al. Complications of Full-Endoscopic Versus Microendoscopic Foraminotomy for Cervical Radiculopathy: A Systematic Review and Meta-Analysis. World Neurosurg 2018;114:217-27. [Crossref] [PubMed]
- Wang TY, Lubelski D, Abdullah KG, et al. Rates of anterior cervical discectomy and fusion after initial posterior cervical foraminotomy. Spine J 2015;15:971-6. [Crossref] [PubMed]
- Lubelski D, Healy AT, Silverstein MP, et al. Reoperation rates after anterior cervical discectomy and fusion versus posterior cervical foraminotomy: a propensity-matched analysis. Spine J 2015;15:1277-83. [Crossref] [PubMed]
- Kang MS, Choi KC, Lee CD, et al. Effective cervical decompression by the posterior cervical foraminotomy without discectomy. J Spinal Disord Tech 2014;27:271-6. [Crossref] [PubMed]
- Young RM, Leiphart JW, Shields DC, et al. Anterior cervical fusion versus minimally invasive posterior keyhole decompression for cervical radiculopathy. Interdiscip Neurosurg 2015;2:169-76. [Crossref]
- Çağlar YS, Bozkurt M, Kahilogullari G, et al. Keyhole Approach for Posterior Cervical Discectomy: Experience on 84 Patients. Minim Invasive Neurosurg 2007;50:7-11. [Crossref] [PubMed]
- Korinth MC, Kruger A, Oertel MF, et al. Posterior foraminotomy or anterior discectomy with polymethyl methacrylate interbody stabilization for cervical soft disc disease: results in 292 patients with monoradiculopathy. Spine (Phila Pa 1976) 2006;31:1207-14; discussion 1215-6. [Crossref] [PubMed]
- Selvanathan SK, Beagrie C, Thomson S, et al. Anterior cervical discectomy and fusion versus posterior cervical foraminotomy in the treatment of brachialgia: the Leeds spinal unit experience (2008-2013). Acta Neurochir (Wien) 2015;157:1595-600. [Crossref] [PubMed]
- Wirth FP, Dowd GC, Sanders HF, et al. Cervical discectomy. A prospective analysis of three operative techniques. Surg Neurol 2000;53:340-6; discussion 346-8. [Crossref] [PubMed]
- Cho TG, Kim YB, Park SW. Long term effect on adjacent segment motion after posterior cervical foraminotomy. Korean J Spine 2014;11:1-6. [Crossref] [PubMed]
- Tumialán LM, Ponton RP, Gluf WM. Management of unilateral cervical radiculopathy in the military: the cost effectiveness of posterior cervical foraminotomy compared with anterior cervical discectomy and fusion. Neurosurg Focus 2010;28:E17. [Crossref] [PubMed]
- Jagannathan J, Sherman JH, Szabo T, et al. The posterior cervical foraminotomy in the treatment of cervical disc/osteophyte disease: a single-surgeon experience with a minimum of 5 years' clinical and radiographic follow-up. J Neurosurg Spine 2009;10:347-56. [Crossref] [PubMed]
- Deukmedjian AJ, Jason Cutright ST, Augusto Cianciabella PC, et al. Deuk Laser Disc Repair((R)) is a safe and effective treatment for symptomatic cervical disc disease. Surg Neurol Int 2013;4:68. [Crossref] [PubMed]
- Ahn Y, Moon KS, Kang BU, et al. Laser-assisted posterior cervical foraminotomy and discectomy for lateral and foraminal cervical disc herniation. Photomed Laser Surg 2012;30:510-5. [Crossref] [PubMed]
- Jeon HC, Kim CS, Kim SC, et al. Posterior Cervical Microscopic Foraminotomy and Discectomy with Laser for Unilateral Radiculopathy. Chonnam Med J 2015;51:129-34. [Crossref] [PubMed]
- Tay B, Jho D. Minimally Invasive Cervical Foraminotomies. Operative Techniques in Orthopaedics 2019. [Crossref]
- Kim KT, Kim YB. Comparison between open procedure and tubular retractor assisted procedure for cervical radiculopathy: results of a randomized controlled study. J Korean Med Sci 2009;24:649-53. [Crossref] [PubMed]
- Winder MJ, Thomas KC. Minimally invasive versus open approach for cervical laminoforaminotomy. Can J Neurol Sci 2011;38:262-7. [Crossref] [PubMed]
- Eicker SO, Steiger HJ, El-Kathib M. A Transtubular Microsurgical Approach to Treat Lateral Cervical Disc Herniation. World Neurosurgery 2016;88:503-9. [Crossref] [PubMed]
- Uehara M, Takahashi J, Kuraishi S, et al. Mini Open Foraminotomy for Cervical Radiculopathy: A Comparison of Large Tubular and TrimLine Retractors. Asian Spine J 2015;9:548. [Crossref] [PubMed]
- Kim CH, Kim KT, Chung CK, et al. Minimally invasive cervical foraminotomy and diskectomy for laterally located soft disk herniation. Eur Spine J 2015;24:3005-12. [Crossref] [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [Crossref] [PubMed]
- Clark JG, Abdullah KG, Steinmetz MP, et al. Minimally Invasive versus Open Cervical Foraminotomy: A Systematic Review. Global Spine J 2011;1:9-14. [Crossref] [PubMed]