Total subaxial reconstruction
Introduction
The cervical spine protects the cervical spinal cord, enables normal neurological function and is fundamental for maintenance of horizontal gaze. Normal sagittal alignment is also essential for associated neck functions such as phonation, breathing, swallowing and cerebral blood flow. Under normal conditions, the cervical spine has a wide range of motion requiring low muscle energy expenditure. When cervical alignment departs from normal, there is increased energy expenditure by the extensor muscles to support the center of mass of the head and maintain horizontal gaze. Moreover, cervical kyphosis leads to gradual spinal cord stretching which in turn causes an alteration in microcirculation eventually resulting in cord ischemia and, potentially, myelopathy (1). Surgical treatment of cervical pathology has been traditionally focused on decompression of neural elements and ensuring arthrodesis. However, there is increasing evidence that correction of deformity leads to superior clinical outcomes for pain, fusion and construct durability.
Cervical deformity can be broadly defined as a departure from normal cervical alignment and occurs primarily as kyphosis. Pure coronal deformity and kyphoscoliosis can also occur in the cervical spine but are much more rate. Cervical deformity can occur as a local (single segment), regional (purely cervical) or global process (2). An estimated 2 to 35% of patients presenting with cervical myelopathy will have associated cervical kyphosis. Even within the cervical spine, surgical plans may vary vastly for deformities occurring at the craniocervical junction (O-C2), subaxial spine (C2-T1) or as a result of upper thoracic kyphosis.
Cervical deformity can have multiple causes and may be essentially divided into congenital or acquired. Primary causes such as segmentation errors are rare and more common in the O-C2 segment. Genetic syndromes such as Larsen Syndrome, Diastrophic Dysplasia, osteogenesis imperfecta are also rare. By far, the most common form of cervical deformity is secondary cervical kyphosis. This can happen due to myriad reasons such as disc degeneration, neuromuscular disorders, trauma, infection, rheumatological, post-radiation and post-surgical (iatrogenic). The most common of them are the degenerative and iatrogenic forms. Kyphosis is the prototypical deformity secondary to disc degeneration due to a decrease in disc and anterior column height and is thus more common in adults. Post-laminectomy kyphosis is the most common form of deformity in children and young adults, with a highly variable reported incidence ranging from 9% to 95%, with the higher range usually involving follow-up longer than 10 years or associated occipital decompression (3,4). Particularly with subaxial cervical kyphosis, the vast majority of patients referred for surgical treatment tend to have degenerative or iatrogenic deformity.
The purpose of this article is to review the clinical presentation, radiological assessment and surgical correction of deformity involving the subaxial cervical spine.
Clinical presentation and radiological assessment
Many patients with cervical deformity are asymptomatic: the cord compression is not clinically apparent and mobile segments compensate for the kyphotic area in order to maintain horizontal gaze and cervical function. Kyphosis is, however, a proven contributor to myelopathy: the spinal cord is stretched and pushed against the posterior border of the vertebral bodies but at the same time is tethered by the dentate ligament and roots. There is compromise of the anterior vascular supply through direct compression as well. Spinal cord damage then ensues as a multifactorial process, including ischemia, demyelination, neuronal loss and ultimately formation of a fibrous or cystic scar (myelomalacia). Patients may also present with neck pain from the increased energy expenditure by the posterior cervical muscles, myelopathy, radiculopathy, failure to maintain horizontal gaze and in extreme cases, chin on chest deformity with symptoms due to compromise of other cervical structures such as dysphagia or dysphonia.
Clinical evaluation includes thorough history-taking and a neurological and orthopedic exam. History is targeted at determining the etiology of the deformity and whether a patient is symptomatic from it. Associated cervical complaints are noted and whether the patient has difficulty maintaining horizontal gaze. The clinical exam should include both an upright and a supine exam to assess flexibility. The chin to brow angle (CBVA) was descripted as a clinical evaluation tool that is also measured on full-length scoliosis radiographs. Head to chest alignment is noted; purely cervical deformities typically present with the head aligned over the shoulders while patient with thoracic hyperkyphosis will have anterior offset of the head in relation to T1. Extreme deformity cases may present with thinning skin over the lower cervical spinous processes or a submental ulcer. In thoracic hyperkyphosis, patients will often compensate in the sitting position by slumping on the chair with correction of head position and horizontal gaze.
Radiological assessment is performed with lateral static, flexion and extension radiographs in the upright position; we highly recommend that full spine radiographs are obtained when a cervical deformity is suspected. Radiology technicians may frequently rotate a focal cervical radiograph to make it fit the film or the computer field of view; this will affect measurements such as the T1 slope and C2–7 SVA. Additionally, advanced imaging such as MRI is used to visualize the cord and neural elements. In select cases with severe deformity or prior implants, a CT myelogram may be preferred due to thin cuts and minimization of instrumentation artifact. Advanced imaging may also offer an assessment of the flexibility of the deformity when the patient is supine and a more exact comparison can be performed with supine radiographs.
There are several radiographic parameters measured on cervical and full-spine radiographs that assess form and alignment. The first measurement, classically performed off a lateral photograph of the patient and now on full spine radiographs, is the chin to brow vertical angle (CBVA). With the standing upright patient, a line is drawn from the forehead to chin and then the angle with another line perpendicular to the floor is measured. Horizontal gaze is ideally directed slightly downward, +5° to 10° particularly in rigid patients such as ankylosing spondylitis or post occipito-cervical fusion. Superiorly-directed gaze might not only compromise ambulation (inability to look at the floor) but also cause dysphagia.
Cervical lordosis has historically been measured in a variety of different ways; with the popularization of electronic imaging, the Cobb method has become virtually universal (2,5). This angle is measured from C1–C7 or typically from C2–C7. The inferior and perpendicular endplates of both vertebral bodies are used. The amount of cervical lordosis that is considered normal is variable and increases with age. In an attempt to extrapolate the spinopelvic correlations to the cervical area, in 2012 Lee et al. described the thoracic inlet angle (TIA), cervical tilt (CT) and T1 slope (T1sl) (6). Similarly to the lumbar spine sitting atop the static pelvic ring, the head and the cervical spine sit on a relatively immobile bone ring, limited by T1 behind, the first ribs on the sides, and the anterior aspect of the sternum in front—the TIA, which would be the cervical equivalent of pelvic incidence. The cervical tilt is an angle formed by a line from the upper end of the sternum to the center of the superior endplate of T1 and a vertical line from this point perpendicular to the floor. The T1 slope (T1sl) is an angle formed by a line parallel to the superior endplate of T1 and a horizontal line parallel to the floor. These three parameters are interrelated so that TIA = T1sl + CT. While spinopelvic correlations have been found to strongly influence outcome following lumbar fusions, the same has not yet been proven for the cervical spine. While these are geometric analogs to the spinopelvic parameters, the correlations are not as strong with outcome. The T1sl in particular has been used to attempt to predict the amount of cervical lordosis with variable success. One fundamental difference is that the pelvic incidence remains relatively stable during adult life while T1sl is a dynamic measurement directly influenced by thoracolumbar anatomy (6,7) (Figure 1).
Cervical sagittal imbalance so far has been a stronger correlation with PRQOL (patient-reported quality of life). C2-7 sagittal vertical axis is the most commonly used of the several options: it uses a line from the centromere of C2 and perpendicular to the floor and the distance from this line to the postero-superior border of the C7 vertebral body is measured. Tang et al. have correlated a distance greater than 40mm in post-fusion patients with worse outcomes. Just like any measurement utilizing lines perpendicular to the floor, it is important to utilize full-spine radiographs to ensure the image is not artificially rotated (8).
Surgical treatment
Goals for successful correction of kyphosis are maintenance of comfortable horizontal gaze, decompression of neurological elements, restoration of the normal function of other cervical structures (i.e., swallowing) and achievement of stable fusion with the head aligned with the pelvis and thoracic inlet ring.
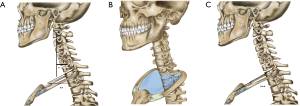
Following full-spine and cervical dynamic films and advanced imaging, deformity correction goals are established. While there are no well-established normative parameters, based of Tang et al. we generally strive to maintain T1sl-CL <15°, cervical SVA <4 cm and CBVA to be between 0 and +20° although this may be occasionally different for each patient (9). In 2014, Hann et al. described an algorithm for selecting a surgical approach in cervical deformity correction (10), which is very similar to that adopted by the senior author (Figure 2). An initial determining factor is whether the deformity is fixed (not passively correctable) or nonfixed (passively correctable), based on preoperative evaluation (flexion/extension X-rays) and comparison with supine imaging. If the deformity is nonfixed, the preferred approach is a 360° fusion starting with multiple anterior cervical discectomy and fusions (ACDFs) or anterior corpectomy and fusions (ACCFs) and then posterior fixation. Exceptionally, patients who are elderly, medically complex, mild or especially mobile deformities and those with contraindications for anterior approach (e.g., radiation therapy to anterior neck) may be treated posteriorly only (Figure 3).
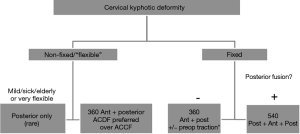
In the case of a fixed deformity, the posterior elements are assessed for fusion. If there is no posterior fusion, an anterior-posterior approach is adopted. With the presence of prior posterior instrumentation or other form of posterior fusion, a posterior release with osteotomies is the necessary first step, resulting in a 540° approach. Ankylosing spondylitis is a special situation that will not be discussed here; if the spine is circumferentially fused, a single extension osteotomy at the base of the neck is utilized.
Anterior techniques
The three main anterior techniques described for patients requiring anterior reconstruction are ACDFs, ACCFs and anterior osteotomy (ATO). Most of patients can be treated with multiples ACDFs, which is a common surgical procedure done by spinal surgeons, less morbid, and allows satisfactory corrections and decompressions. Traynelis described an average 25° correction in his series using predominantly multiple ACDFs and no posterior osteotomies were necessary (11). The use of corpectomies is primarily indicated for decompression (when the worst cord compression is ventral and directly posterior of the vertebral body) and not for correction. The ATO is used for fixed deformities and fused vertebral bodies. This technique promotes a more powerful correction: it involves a complete anterior release from foramen transversarium to foramen transversarium. It is more technically challenged, rarely performed by most surgeons and is associated with more complications.
ACDF
Every spine surgeon should be familiar with this technique. We normally employ a left-sided approach although there is no high-quality study favoring one side or another (12). The position of the left inferior laryngeal nerve is usually more caudal on the left; additionally, a nonrecurrent inferior laryngeal nerve is present on the right in ~0.7% of patients (13). The overall incidence of recurrent laryngeal nerve (RNL) injury has been reported between 1% and 11% in initial operations and 14.1% in reoperations (14,15). Any patient with prior anterior cervical surgery should be assessed for vocal cord function by an otolaryngologist before any new cervical procedure. If any lesions could be detected we prefer the approach by the left side, but if any abnormality is detected then the same approach must be used in order to prevent the possibility of bilateral injury to the RNL.
Positioning is supine with a roll under the scapulae and slight extension. Gardner-Wells tongs and vector traction can be helpful in positioning and correction. Usually a transverse incision can expose from C2 to T1 but 4 or more levels must be accessed we prefer a longitudinal “carotid type” incision. The usual Smith-Robinson approach, between the tracheoesophageal bundle and the carotid sheath is used to expose the midline raphe of the longus colli muscles. Preoperatively, we note the distances between the vertebral arteries and utilize that to determine our lateral extent of dissection. This distance is normally around 25 mm in most patients and at least 20 mm can be safely exposed. We find that a table-mounted retractor is useful for deformity cases and access cranial to C3. Distractor pins positioned in a convergent manner or a Cloward spreader can be utilized after release to segmentally correct kyphosis. A large interspace graft is used to maximize reconstruction of the anterior column.
Following segmental reconstruction, we normally finish anterior correction by utilizing a plate with variable-angle screws and three-point bending maneuvers. If a circumferential procedure is performed, one can use stand-alone cages anteriorly (9) but these are biomechanically weaker and associated with more long-term subsidence and loss of cervical lordosis (9,16,17). The plate is kept as short as possible to prevent adjacent-level ossification (18,19). The most cranial and caudal screw holes are made at the corners of the adjacent level body. The screw insertion is guided by fluoroscopy and bicortical whenever possible; the intervening vertebral bodies are then reduced to the lordotic plate as described by Traynelis (11). The number of additional intermediate reduction points is the main reason ACDFs is preferred over ACCF. A correction of approximately 25° can be achieved with this technique (11).
ACCF
When compared to multilevel ACDFs, anterior cervical corpectomy and fusion (ACCF) has greater blood loss and longer operation times, generates higher bone-screw stress, are more expensive and associated with smaller correction of kyphosis (20,21). Instrumentation failure rates in standalone multi-level ACCFs high, up to 9% in two-level and 50–71% in three-level corpectomies (22,23). For those reasons, we prefer multi-level ACDFs for anterior reconstructions and corpectomies are used when the compression of the spinal cord is behind the vertebral body or in cases that the pathology results in vertebral destruction (e.g., spondylodiscitis).
The approach for ACCF is similar of that described for ACDF and the vertebral body is removed using Leksell rongeur and a high-speed drill. We constantly reassess corpectomy width to ensure both an adequate decompression and adherence to the midline. Before placing the cage, additional distraction can be applied with pins, traction or an intervertebral spreader. We avoid using multiple corpectomies: when greater decompressions are necessary, a hybrid corpectomy-discectomy construct provides better deformity correction and are able to resist axial, rotational and translational forces better (24).
AO
AO can be applied in those fixed deformities due ankylosis of multiple vertebral bodies. The procedure consists in perform a osteotomy at fused vertebral bodies at the level of the previous disc and provides excellent corrections, up to 23° (without posterior fixation) to 32° (with posterior fixation) (25).
The approach is the same that described before for ACDF but can be challenging if the neck is extremely kyphotic. Usually the head of the patient is placed above multiple folded sheets and traction is applied with Gardner-Wells tongs (18). When a coronal deformity is associated the approach is done from the convex side because it is easier to expose those levels. The vertebral artery anatomy is studied and particularly important here because the osteotomy includes both lateral uncinate process, from transversarium to transversarium. Following longus colli release and retraction, blunt dissection is performed lateral to uncinate process with a penfield 2 dissector. This maneuver allows identification of the lateral limits of the osteotomy. The bone resection is done at the same level as previous disc space with a 3mm high-speed drill and reaches posteriorly until the PLL and complete removal of the uncinate process. If coronal correction is necessary, asymmetrical drilling can be done. Vertebral body pins or a vertebral body spreader can be used to improve correction. After the osteotomy is attained the anesthesiology can remove the folded sheets behind patient head and downward force is applied on patient forehead. A cage is then placed in the osteotomy site and plated; posterior fixation is usually performed as well.
Posterior techniques
From the biomechanical standpoint, modern screw-rod posterior fixation is much stronger than any anterior instrumentation (26). In addition, a wide decompression can be achieved including the posterior elements. It is rare in our practice that a patient with cervical deformity will not have a posterior approach either for additional correction, decompression or supplementary fixation. The posterior techniques include posterior fixation and fusion, posterior complex osteotomy (PCO–Ponte osteotomy/“Smith-Petersen”) and pedicle subtraction osteotomy (PSO).
In patients with mild flexible kyphotic deformities or those with compromised posterior band (e.g., post-laminectomy kyphosis or neuromuscular disease) a conventional posterior approach alone may be performed (27). For these cases flexible cases, fixation normally encompasses at least C2-T1. Our preferred techniques are C2 pars screws, C3-6 lateral mass fixation and thoracic pedicle screw placement. The anatomical parameters for these techniques are very reliable and in the absence of a malformation or destructive lesion will work for almost 100% of patients. C7 is usually spared to avoid transitioning the rod from the lateral mass fixation to pedicle fixation. Positioning is highly variable; we employ the Jackson frame for ease of positioning (allows inline rotation from supine to prone), fluoroscopy use and ability to incorporate both a Mayfield head holder or Gardner-Wells tongs. We prefer Gardner-Wells tongs to allow for gentle lordotic correction during final rod locking, following laminectomy and posterior release. Bivector traction is also a possibility with this setup although greater corrections are only achieved with PCO or PSO.
PCO consists in complete removal of the posterior elements including the superior and inferior articulating processes. This has been incorrectly termed a “Smith-Petersen” osteotomy: the PCO relies on an open anterior disc to promote the ability to compress posteriorly while the original Smith-Petersen osteotomy is an anterior extension osteotomy described in a rigid spine (ankylosing spondylitis) (28). It can be more appropriately compared to the Ponte osteotomy described in the thoracic spine for Scheuermann kyphosis (29). The posterior gap generated by the wide resection allows posterior compression to reduce the posterior column and generate lordosis. A PCO also provides complete foraminal decompression and multiple PCOs can also be performed: care must be exerted to preserve the lateral mass for screw fixation if PCOs are being performed cranial and caudal to a single level. The original Smith-Petersen osteotomy can still be performed in highly-selected rigid cases at C6-7 or C7-T1 complemented with posterior instrumentation.
Pedicle subtraction osteotomy (PSO) is a posterior technique that was originally described at C7 to provide significant lordosis and correction of cervical sagittal imbalance. This technique is rarely performed and is more recent. A very significant amount of correction can be generated but when originally described, significant neurological morbidity was described (30). Most authors are still determining the fine parameters for its application: we have reserved this osteotomy for cases with elevated T1sl (reflecting a thoracic kyphotic deformity) and relocated it to T2 with less neurologic morbidity and the ability to perform a vertebral column resection if the anterior column collapses during the osteotomy or closure.
Case illustrations
Case 1
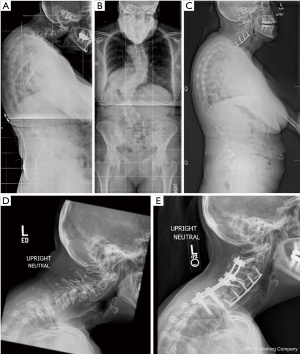
A 57-year-old female with adolescent idiopathic scoliosis, now inability to maintain horizontal gaze. Long cassette films demonstrating double thoracolumbar curve and subaxial kyphosis with increased CBVA. A limited subaxial treatment plan was offered to avoid C2-pelvis fusion while patient is relatively young. C3-7 ACDF with correction of listheses and kyphosis was performed (Figure 4A,B). Normal CBVA with maintained increased cervical sagittal balance. Patient then underwent reinforcement with posterior cervical fusion for stabilization (Figure 4C). Preoperative lateral cervical XR (Figure 4D) and final result (Figure 4E). It is anticipated that full correction will eventually be necessary with osteotomy to correct elevated T1 slope.
Case 2
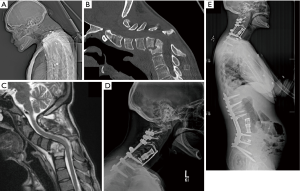
A 32-year-old female victim of domestic abuse and involuntary IV drug use with subacute discitis/osteomyelitis C5–7 and L3–4 and both cervical and lumbar kyphosis. CT topogram with rigid kyphosis while lying supine (Figure 1A); ankylosis present at C4–6 (Figure 1B); this fusion extended circumferentially to involve the lateral masses; MRI with active osteomyelitis (Figure 1C). Per protocol in Figure 1, she underwent a 540 approach with posterior osteotomies, C5–7 corpectomies and C2-T3 reconstruction, followed 2 weeks later by T12-pelvis posterior-only reconstruction. Final result 6 months later (Figure 1D,E).
Case 3
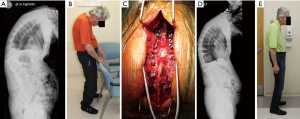
A 65-year-old dentist with ankylosing spondylitis had sustained a ground level fall with C5 fracture five years prior to presentation, having undergone a C3-7 posterior fusion then. He was forced to retire due to inability to maintain horizontal gaze. Now presents two weeks after a ground level fall with a T12–L1 osseous Chance fracture (Figure 5A,B). He underwent percutaneous T10–L2 fixation of fracture in the lateral decubitus position, followed two weeks later by a C7–T1 Smith-Petersen osteotomy and C3-T3 posterior fusion in the sitting position (Figure 5C). Significant improvement in horizontal gaze and function, able to resume full time dentistry practice despite residual global positive sagittal malalignment and refused further correction of deformity (Figure 5D,E). The Radiology Technician has kindly provided a reminder that the patient is kyphotic in Figure 5A.
Conclusions
Cervical deformity is an evolving topic as our corrective techniques are further refined. An accurate understanding of the normal form of the spine and the conditions that deviate from it, is already necessary for every surgeon who operates in the cervical spine to ensure successful outcomes: a fused spine is much harder to correct than a flexible spine, especially if it has been locked incorrectly in place by surgery. Particularly the interaction between cervical and thoracolumbar deformity in the same patient is a fast-evolving topic and we should see more combined reconstructions in the future. Subaxial reconstruction techniques are a central piece to achieving successful lordotic and functional cervical form and we recommend that every surgeon be familiar with at least its diagnosis, assessment and basic corrective techniques of a thorough ACDF and PCO.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Lee A. Tan and Ilyas S. Aleem) for the series “Advanced Techniques in Complex Cervical Spine Surgery” published in Journal of Spine Surgery. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: The series “Advanced Techniques in Complex Cervical Spine Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tan LA, Riew KD, Traynelis VC. Cervical Spine Deformity—Part 1: Biomechanics, Radiographic Parameters, and Classification. Neurosurgery 2017;81:197-203. [Crossref] [PubMed]
- Ames CP, Blondel B, Scheer JK, et al. Cervical Radiographical Alignment: Comprehensive Assessment Techniques and Potential Importance in Cervical Myelopathy. Spine 2013;38:S149-60. [Crossref] [PubMed]
- McLaughlin MR, Wahlig JB, Pollack IF. Incidence of postlaminectomy kyphosis after Chiari decompression. Spine 1997;22:613-7. [Crossref] [PubMed]
- Deutsch H, Haid RW, Rodts GE, et al. Postlaminectomy cervical deformity. Neurosurg Focus 2003;15:E5. [Crossref] [PubMed]
- Scheer JK, Tang JA, Smith JS, et al. Cervical spine alignment, sagittal deformity, and clinical implications: a review. J Neurosurg Spine 2013;19:141-59. [Crossref] [PubMed]
- Lee SH, Kim KT, Seo EM, et al. The influence of thoracic inlet alignment on the craniocervical sagittal balance in asymptomatic adults. J Spinal Disord Tech 2012;25:E41-7. [Crossref] [PubMed]
- Oe S, Togawa D, Yamato Y, et al. Comparison of Postoperative Outcomes According to Compensatory Changes of the Thoracic Spine Among Patients With a T1 Slope More Than 40°. Spine 2019;44:579-87. [Crossref] [PubMed]
- Tang JA, Scheer JK, Smith JS, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery 2012;71:662-9; discussion 669. [Crossref] [PubMed]
- Tan LA, Riew KD, Traynelis VC. Cervical Spine Deformity—Part 2: Management Algorithm and Anterior Techniques. Neurosurgery 2017;81:561-7. [Crossref] [PubMed]
- Hann S, Chalouhi N, Madineni R, et al. An algorithmic strategy for selecting a surgical approach in cervical deformity correction. Neurosurg Focus 2014;36:E5. [Crossref] [PubMed]
- Traynelis VC. Total subaxial reconstruction. J Neurosurg Spine 2010;13:424-34. [Crossref] [PubMed]
- Kilburg C, Sullivan HG, Mathiason MA. Effect of approach side during anterior cervical discectomy and fusion on the incidence of recurrent laryngeal nerve injury. J Neurosurg Spine 2006;4:273-7. [Crossref] [PubMed]
- Henry BM, Sanna S, Graves MJ, et al. The Non-Recurrent Laryngeal Nerve: a meta-analysis and clinical considerations. Peer J 2017;5:e3012. [Crossref] [PubMed]
- Beutler WJ, Sweeney CA, Connolly PJ. Recurrent Laryngeal Nerve Injury With Anterior Cervical Spine Surgery: Risk With Laterality of Surgical Approach. Spine 2001;26:1337-42. [Crossref] [PubMed]
- Erwood MS, Hadley MN, Gordon AS, et al. Recurrent laryngeal nerve injury following reoperative anterior cervical discectomy and fusion: a meta-analysis. J Neurosurg Spine 2016;25:198-204. [Crossref] [PubMed]
- Zhu D, Zhang D, Liu B, et al. Can Self-Locking Cages Offer the Same Clinical Outcomes as Anterior Cage-with-Plate Fixation for 3-Level Anterior Cervical Discectomy and Fusion (ACDF) in Mid-Term Follow-Up? Med Sci Monit 2019;25:547-57. [Crossref] [PubMed]
- Chen Y, Lü G, Wang B, Li L, et al. A comparison of anterior cervical discectomy and fusion (ACDF) using self-locking stand-alone polyetheretherketone (PEEK) cage with ACDF using cage and plate in the treatment of three-level cervical degenerative spondylopathy: a retrospective study with 2-year follow-up. Eur Spine J 2016;25:2255-62. [Crossref] [PubMed]
- Tan LA, Riew KD. Anterior cervical osteotomy: operative technique. Eur Spine J 2018;27:39-47. [Crossref] [PubMed]
- Park JB, Cho YS, Riew KD. Development of adjacent-level ossification in patients with an anterior cervical plate. J Bone Joint Surg Am 2005;87:558-63. [Crossref] [PubMed]
- Oh MC, Zhang HY, Park JY, et al. Two-Level Anterior Cervical Discectomy Versus One-Level Corpectomy in Cervical Spondylotic Myelopathy Spine 2009;34:692-6. [Crossref] [PubMed]
- Hussain M, Nassr A, Natarajan RN, et al. Corpectomy versus discectomy for the treatment of multilevel cervical spine pathology: a finite element model analysis. Spine J 2012;12:401-8. [Crossref] [PubMed]
- Sasso RC, Ruggiero RA, Reilly TM, et al. Early reconstruction failures after multilevel cervical corpectomy. Spine 2003;28:140-2. [Crossref] [PubMed]
- Vaccaro AR, Falatyn SP, Scuderi GJ, et al. Early failure of long segment anterior cervical plate fixation. J Spinal Disord 1998;11:410-5. [Crossref] [PubMed]
- Steinmetz MP, Stewart TJ, Kager CD, et al. Cervical deformity correction. Neurosurgery 2007;60:S90-7. [Crossref] [PubMed]
- Kim HJ, Piyaskulkaew C, Riew KD. Anterior Cervical Osteotomy for Fixed Cervical Deformities Spine 2014;39:1751-7. [Crossref] [PubMed]
- Singh K, Vaccaro A, Kim J, et al. Biomechanical Comparison of Cervical Spine Reconstructive Techniques After a Multilevel Corpectomy of the Cervical Spine. Spine 2003;28:2352-8. [Crossref] [PubMed]
- Dru AB, Lockney DT, Vaziri S, et al. Cervical Spine Deformity Correction Techniques. Neurospine 2019;16:470-82. [Crossref] [PubMed]
- Smith-Petersen MN, Larson CB, Aufranc OE. Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. Clin Orthop 1969.6-9. [PubMed]
- Geck MJ, Macagno A, Ponte A, et al. The Ponte procedure: posterior only treatment of Scheuermann’s kyphosis using segmental posterior shortening and pedicle screw instrumentation. J Spinal Disord Tech 2007;20:586-93. [Crossref] [PubMed]
- Wollowick AL, Kelly MP, Riew KD. Pedicle Subtraction Osteotomy in the Cervical Spine Spine 2012;37:E342-8. [Crossref] [PubMed]