Biportal endoscopic spine surgery (BESS): considering merits and pitfalls
Introduction
Fully-endoscopic spine surgery has been developed and reported with good results. But still there are some limitations in handling surgical instruments around the neural structures due to the small working space and corridor. With the uniportal endoscopic procedure, direct targeted posterior decompression of the lamina and medial part of the junction of the inferior articular process and superior articular process can be tried with posterior or posterolateral approach. But it is difficult to use conventional instruments such as nerve root retractor and other microscopic instruments through the uniportal endoscopic corridor. The author describes and shows a step-by-step biportal endoscopic techniques for performing a fully endoscopic lumbar laminectomy and discectomy and discuss the advantages and pitfalls involved in this procedure.
Case presentation (Figures 1-3, Video 1)

Case 1 (Figure 1)
A 69-year-old male patient complained chronic back pain and neurogenic claudication in both legs after 10-minute walk for 2 years medication and physical therapy. The patient underwent unilateral laminectomy and bilateral flavectomy with muscle preserving paramedian biportal endoscopic spinal surgery (BESS) technique. The operation time was 70 minutes. The patient presented regression of neurological deficit after operation.
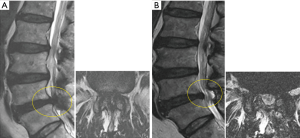
Case 2 (Figure 2)
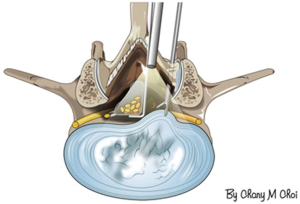
A 76-year-old woman with a history of chronic low back pain presented with 40 days of severe right leg pain, tingling and claudication. The magnetic resonance imaging (MRI) demonstrated severe stenosis at L4–5 foramen with herniated disc. Utilizing extraforaminal BESS technique, L5 superior articular process was partially resected less than 50% and allowed for preservation of the facet joint and stability. The biportal endoscope and assistant nerve retractor helped avoid neural injury. The operation time was 120 minutes. Postoperatively, the patient was neurologically intact, and no instability was demonstrated.
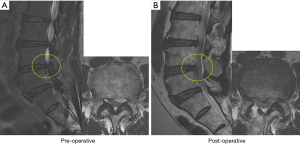
Case 3 (Figure 3)
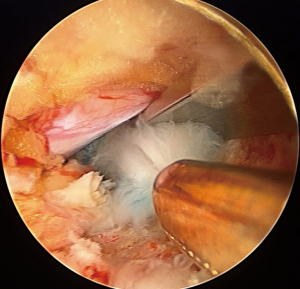
A 66-year-old man with a history of low back pain presented with several days of severe right leg pain, lower extremity numbness, tingling and limping gait. The MRI showed ruptured migrated disc fragment impinging L4 nerve root at the L4–5 lateral recess. With the posterior approach a small laminotomy was made and the ligamentum flavum was resected partially and the impinged nerve root was relieved successfully after targeted fragmentectomy with preservation of the nerve root with the retractor. The operation time was 90 minutes. After operation his neurologic symptom was relieved dramatically.
Description of the surgical techniques
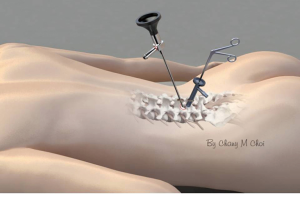
The patient is placed in the prone position over the radiolucent frame in a flexed position. Fluoroscopic confirmation of the operation level is made. Skin entry points are chosen considering the pathological lesion site and the patient’s anatomical variation. Usually two entry points are made about 1 cm above and below the disc space at the interpedicular line for the posterior approach (Figure 4). For the foraminal lesion, we decide entry points along the imaginary line connecting the tips of the transverse processes above and below the foramen lesion for the posterolateral approach (Figure 5). In order to make free outflow of irrigation fluid, a linear fascial opening is made wide more than 7 mm in length with a 15-blade scalpel along the skin crease. Multifidus muscle is separated atraumatically by the blunt muscle-splitting technique with a serial dilator touching the lamino-facet junction and separated with a blunt muscle detacher. Correct position of the instrument is confirmed with the biplanar fluoroscopic image guidance (1).
For the posterior approach, a working sheath is inserted through one portal for the scope and the other wider working portal is made with splitting of the erector spinae and multifidus muscles for the instruments. The multifidus muscle is detached and separated from the lamina to prepare a working space. Serial dilator is inserted into the intermuscular septum and then multifidus muscle is separated from the lamina by muscle detacher (Figure 6). Minor muscle bleeding is well controlled by low voltage radiofrequency electrode (Delphi 1000 professional endoscopic radiofrequency generator and electrode tip, C&S Medical Co., Ltd.). One of the main advantages of this technique is creating an atraumatic working space in the potential fatty space between the multifidi muscles by avoiding crushing and over-retraction injuries made by other conventional minimally invasive surgeries. Furthermore, we can achieve a clear and wide visual field in the epidural working space preserving epidural fat and vessels. This clear view is obtained from the working space made by the biportal endoscopic spine surgery which serves as cavity-like joint space in the arthroscopic surgery.
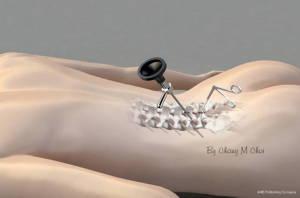
Through the skin opening portal, conventional surgical instruments, such as drill, Kerrison rongeur, curette and pituitary forceps are inserted and can be used freely in various access angle like open surgery. Ipsilateral decompression is performed first on the pathological lesion site. Hypertrophied facet joints, lamina and thickened ligamentum flavum compressing the neural structures are selectively removed in a safe manner by drilling and then a curette or a punch can be used to relieve the neural structures. Bilateral decompression can be performed through the unilateral lamina opening. For bilateral decompression, wide laminotomy is made beginning at the spinolaminar junction undercutting the base of the spinous process. Partial resection of the base of the spinous process allow free passage of the scope into the contralateral side in the spinal canal. After exposure, the ligamentum flavum is separated from the contralateral lamina with a blunt dissector. When we go through the contralateral side for the endoscopic procedure, the scope is inserted dorsal to the ligamentum flavum being kept intact to the dura for the protection of the neural structures. After full exposure of the contralateral side, the ligamentum flavum is detached from the dura and removed with a curette and a Kerrison rongeur. When there is a dense adhesion between the ligamentum flavum and the dura, we do not aggressively remove it because dural tear may occur during the procedure. Bony decompression of the facet joint and lateral recess is performed cranially or caudally again using with a diamond drill or an ultrasonic bone cutter. Medal partial facetectomy is performed by undercutting manner to keep the dorsal part intact to preserve the facet joint integrity. After sufficient bony decompression, further delicate resection of the remained ligamentum flavum is done with curette or curved punch to fully relieve the neural structures (2-4) (Figure 7). Meticulous manipulation of the Kerrison rongeur is required to decompress the lateral recess to avoid dural tear. A small diameter high-speed drill or an ultrasonic bone cutter can be used for the safer decompression of the lateral recess stenosis. Complete decompression is made until the outer edges of the bilateral nerve roots are exposed (5). We can get the clear surgical view and the intact epidural fat and vessels by the continuous saline irrigation below or about 30 mmHg by use of a retractor or cannula for free outflow of the saline. Usually epidural fat and vessels are damaged during the microscopic, microendoscopic and uniportal endoscopic surgeries which lead to postoperative scar formation and dural adhesion resulting in the postlaminectomy syndrome. We can avoid the over-increase of the epidural hydrostatic pressure and the subsequent over-increase of the intracranial pressure (ICP) by maintaining the continuous free outflow of the irrigation fluid through the working portal (6). Laminotomy and flavectomy can be done in the same manner as the microscopic surgery and the epidural bleeding can be more effectively managed by the low-voltage radiofrequency bipolar system under clear vision and by the continuous saline irrigation.

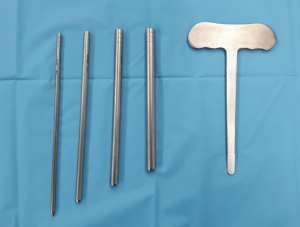
For the foraminal lesion, a working space should be made by the meticulous dissection with a blunt dissector and a low voltage radiofrequency electrode to avoid neuralgia of the dorsal root ganglion and the exiting nerve. Clear visual field and variable access angle by this procedure make the surgeon more comfortable to manage the foraminal lesion. For the beginner, anatomical orientation of the foraminal structures is important. Targeting on the superior articular process is one of the main keys for the orientation at the initial step. This area is the safe zone for the extraforaminal procedures. By the sufficient decompression of the superior articular process using drill or osteotome, we can make enough room for the exiting nerve root to be relieved without much manipulation. Getting more clear and wide view of the exiting nerve by the out-in decompression of the facet joint and foraminal ligament is paramount importance (7). Unlike other endoscopic procedures, the benefit of this surgical technique is the protection of the nerve during the manipulation around the neural structures with use of the specially designed nerve root retractor by an assistant (Figures 8-10). Biportal endoscopic surgical technique allow us to avoid injury to the normal structures and nerves and decompress the contralateral side and remove the pathologic lesion safely with free handling of the assistant nerve protector (Figures 9,11).


Surgical indications
- Spinal stenosis: central, lateral and foraminal, moderate to severe, with or without herniated nucleus pulposus (HNP);
- Herniated disc: central, lateral, migrated, small to large;
- Neural decompression only for stenosis with or without instability;
- Instability: neural decompression combined with the other minimally invasive fusion surgeries.
Limitations
- Decompression of the exiting nerve is difficult in the foraminal stenosis with the narrow disc space and bony spur;
- Decompression alone is not adequate for the unstable stenotic spine. Instrumentation for distraction and stabilization is required.
Avoiding pitfalls and managing complications of biportal endoscopic spine surgery
- Increased ICP: a pressure-controlled arthroscopy irrigation pump must be used carefully for this procedure. This equipment may induce too much increase of the epidural hydrostatic pressure and subsequent over-increase of the ICP which may result in headache and seizure. Continuous free outflow of irrigating saline is important to prevent the over-increase of ICP. If you want to use controlled pressure keep the pressure below 30 mmHg (6).
- Thermal injury of the nerve: use low voltage radiofrequency coagulators instead of the conventional arthroscopic radiofrequency coblator which may cause thermal damage to the neural structures.
- Dural tear: a dense adhesion of the ligamentum flavum to the dura may be encountered in the cases of severe spinal stenosis. Meticulous gentle tractions of the ligamentum flavum from the dura with a punch or forceps may be helpful for safe detachment. Under the continuous saline irrigation, careful insertion of a blunt dissector into the epidural space between the dura and the overlying ligamentum flavum may leads to smooth adhesiolysis with a hydrodissection effect. Specially designed curved curette is helpful for detaching the ligamentum flavum from the lamina insertion site. If there is a dense adhesion between the dura and the ligamentum flavum, we peel off only the outer layer of the ligamentum flavum and the adhesed area is left over to keep the dura intact.
- Instability: instability may be caused by an iatrogenic destruction of the normal facet joint and isthmic portion of the lamina during the procedure. The drawback of the minimally invasive surgery is an accidental destruction of the important normal structures due to the small incision and the narrow operation field. Frequent intraoperative fluoroscopic imaging of the operation site is mandatory to avoid unnecessary resection of the normal structures especially facet joint and isthmic portion of the lamina. These structures should be preserved by cautious undercutting the thick bony structures with drills and ultrasonic bone cutter. Then a small curette or a sharp Kerrison rongeur can be used to remove the remaining thin bony structures compressing the nerves.
- Vascular injury: to prevent vascular injury and unnecessary copious bleeding during the operation of a foraminal lesion, the out-in approach starting at the extraforaminal area avoiding radicular artery under wide and clear view is recommended. Careful management of the inadvertent tear of the radicular artery is required to avoid retroperitoneal hematoma.
If dural tear less than 5 mm occurs small patching with collagen patch will be helpful. If dural opening or tear is too large to be spontaneous healing, I prefer to use fascial graft and small autoclips for dural closure.
Preoperative considerations
Preoperative computed tomography (CT) scan and MRI should be reviewed to find out the availability of this technique in an individual patient.
Intraoperative considerations
- Keep open the out flow of the irrigation fluid and be careful not to increase perithecal pressure below 30 mmHg if possible. Personally, I prefer natural drainage of the outflow of the irrigation water and do not use irrigation pump. Keep in mind the fact that the increase of the epidural hydrostatic pressure may result in the increase of the ICP due to overloading of saline in the epidural space (5). Increase of epidural hydrostatic pressure and subsequent increase of ICP may induce severe headache or seizure.
- Dural tears should be prevented by meticulous detachment of the ligamentum flavum free from the adhesed dura with gentle tractions and saline irrigation by the hydrodissection effect (8).
- Avoid the thermal damage of the neural structures (nerve root and ganglion). At first, we used a conventional radiofrequency probe and generator designed for arthroscopic equipment which generates too much voltage for the spine surgery and result in ganglion damage such as complex regional pain syndrome (CRPS) like sequelae. Now we replaced the generator from the conventional arthroscopic equipment to the low voltage generator which result in decrease of the chance of the thermal damage to the neural structures.
- Frequent intraoperative fluoroscopic imaging for the precise operation site is mandatory. We may go wrong site because slight change of the insertion angle may lead to the wrong level or a wrong site far away from the lesion site.
Postoperative considerations
- The hemovac drain is kept in negative pressure until the hemovac drain is removed;
- Ambulation is recommended with a semi-rigid back brace;
- Specific information is given to the patient about the surgery & potential risks;
- Patients should be informed that there may be some numbness or tingling sense over the dermatome of the nerve operated on, and neuroleptics are taken until the symptoms disappear.
Discussion
Many endoscopic procedures have been introduced as a minimally invasive surgical modality to preserve the overall spinal structures. Too often preservation of the normal bony structures is over-emphasized and the importance of ligaments and muscular structures in the spine are neglected. We may neglect the fact that the multifidus muscle is very important in its function as a stabilizer of joints within the spine. Even recent endoscopic procedures might damage the important medial multifidus muscle because even though the skin opening is small there might be too much destruction of these muscles, ligaments and bony structures inside the small opening (9). We adopted the biportal endoscopic spine surgery system which allows free handling and make it possible for us to use the instruments in the delicate area protecting neural structures preserving normal structures (Figures 6,7). This biportal endoscopic approach going through spatium intermuscular can prevent the injury of the erector spinae from the damage caused by the conventional procedures debriding and crushing important muscles. Otherwise variable access angles provide the surgeon the wider and further detail view of the contralateral side. The paraspinal extraforaminal approach with this technique gives wider view of the foraminal lesion and we can avoid the possible injury of the exiting nerve and the radicular artery. For the foraminal lesion, the superior articular process is decompressed first and then the herniated disc and bony spurs around the foramen are decompressed later to acquire the enough working space around the nerve. Meticulous care should be made for possible thermal and mechanical injury of the ganglion and the exiting nerve during the whole procedure.
The goal of the fully-endoscopic spine surgery is expanding the indications of percutaneous endoscopic lumbar surgery in the management of lumbar canal stenosis via endoscopic approach. Development of the endoscopic instruments especially endodrill [burr], and endoscopic punch allow the spine surgeons to take the opportunity to try lumbar decompression in more minimally invasive approaches (10). But much care should be taken during the procedure for the drill to remain constantly in the centre of the endoscopic view. For this goal, the surgeon should move the endoscope and the endo-drill synchronously. We cannot see the lesion and adjacent neural structures altogether in the narrow corridor with this uniportal system (11,12). There are also limitations of using the conventional spinal surgical instruments through the one portal scope system through the narrow corridor. We introduce the biportal endoscopic system which provides wide angle view and free access of surgical instruments in the limited area in the uniportal approach. Unlike the uniportal system we can manipulate the pathological lesion protecting neural structures with a nerve root retractor when the ligamentum flava protecting the neural structures were removed. For the discectomy procedure alone, we do not remove all the ligament flavum and ligamentum flavum flap is made and keep intact with only partial peripheral resection of the ligament. With root retractor the ligament and neural structures are retracted altogether and the pathological lesion is seen clearly under wide angle view. The neural structures are covered again with the intact ligamentum flavum after discectomy. When the irrigation pump is used the hydrostatic pressure should be closely monitored and kept below 30 mmHg to prevent over-increase of epidural hydrostatic pressure and resultant over-increase of ICP which may induce severe headache or seizure.
Key points of biportal endoscopic spine surgery considering merits of this procedure
- Lamina and spinal foramen are distracted and opened in prone, flexed position;
- Two entry points are properly selected in each case depending on the pathological lesion under fluoroscopic guidance;
- Two approaches are possible depending on the patient’s pathology:
- For the central and lateral stenosis, the posterior approach is chosen;
- The posterolateral approach is adopted for foraminal stenosis.
- Determine biportal entry points to get variable access angle and appropriate view according to the lesion site, e.g., go more lateral for the contralateral lesion;
- Preserve multifidus muscles by going through the intermuscular septum without damage to this muscle by crushing or over-retraction injury;
- Clear vision can be obtained by continuous flow of saline irrigation;
- Keep the ligamentum flavum intact: for the discectomy alone, we preserve the ligamentum flavum as much as possible and by using assistant retractor we can see the neural structures clearly. We can prevent subsequent postoperative dural adhesion which may lead to post-laminectomy syndrome;
- Preserve epidural fat and vessels: intact epidural fat prevents scar formation and postoperative adhesion. Epidural fat can be preserved intact by the meticulous bleeding control with continuous saline irrigation and low voltage radiofrequency bipolar coagulation of the bleeding epidural vessels, without using suction tip over the epidural fat;
- Free handling of conventional surgical instruments through working portal like open microsurgery;
- Steep learning curve for the spine surgeon who is familiar with conventional microscopic spine surgery;
- Broad indication: spinal stenosis, type (central, lateral and foraminal), grade (moderate to severe) with or without HNP, decompression of the neural structures only for the mild instability.
Conclusions
BESS for treatment of degenerative lumbar diseases is a safe and innovative approach under the clear and wide endoscopic view which allows to preserve nerves and spinal structures. More attention is required for the beginner to use instruments carefully around the neural structures.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Hisashi Koga and Alf Giese) for the series “Full-endoscopic Spine Surgery” published in Journal of Spine Surgery. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss.2019.09.29). The series “Full-endoscopic Spine Surgery” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. It does not require any approval of the ethics committee, since it is a study only followed. Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Choi CM, Chung JT, Lee SJ, et al. How I do it? Biportal endoscopic spinal surgery (BESS) for treatment of lumbar spinal stenosis. Acta Neurochir (Wien) 2016;158:459-63. [Crossref] [PubMed]
- Hu ZJ, Fang XQ, Fan SW. Iatrogenic injury to the erector spinae during posterior lumbar spine surgery: underlying anatomical considerations, preventable root causes, and surgical tips and tricks. Eur J Orthop Surg Traumatol 2014;24:127-35. [Crossref] [PubMed]
- Wong AP, Smith ZA, Lall RR, et al. The microendoscopic decompression of lumbar stenosis: a review of the current literature and clinical results. Minim Invasive Surg 2012;2012:325095.
- Polikandriotis JA, Hudak EM, Perry MW. Minimally invasive surgery through endoscopic laminotomy and foraminotomy for the treatment of lumbar spinal stenosis. J Orthop 2013;10:13-6. [Crossref] [PubMed]
- Komp M, Hahn P, Oezdemir S, et al. Bilateral spinal decompression of lumbar central stenosis with the full-endoscopic interlaminar versus microsurgical laminotomy technique: a prospective, randomized, controlled study. Pain Physician 2015;18:61-70. [PubMed]
- Joh JY, Choi G, Kong BJ, et al. Comparative study of neck pain in relation to increase of cervical epidural pressure during percutaneous endoscopic lumbar discectomy. Spine (Phila Pa 1976) 2009;34:2033-8. [Crossref] [PubMed]
- Nomura K, Yoshida M. Microendoscopic Decompression Surgery for Lumbar Spinal Canal Stenosis via the Paramedian Approach: Preliminary Results. Global Spine J 2012;2:87-94. [Crossref] [PubMed]
- Choi DJ, Choi CM, Jung JT, et al. Learning Curve Associated with Complications in Biportal Endoscopic Spinal Surgery: Challenges and Strategies. Asian Spine J 2016;10:624-9. [Crossref] [PubMed]
- Birkenmaier C, Chiu JC, Fontanella A, et al. Guidelines for percutaneous endoscopic spinal surgery. Issue 2, ISMISS/, February 2010.www.ismiss.com
- Ahn Y, Oh HK, Kim H, et al. Percutaneous endoscopic lumbar foraminotomy: an advanced surgical technique and clinical outcomes. Neurosurgery 2014;75:124-33; discussion 132-3. [Crossref] [PubMed]
- Choi G, Deshpande K, Asawasaksakul A, et al. New Era of Percutaneous Endoscopic Lumbar Surgery: Lumbar Stenosis Decompression – A Technical Report. J Spine 2014;3:182.
- Choi G, Pophale CS, Patel B, et al. Endoscopic Spine Surgery. J Korean Neurosurg Soc 2017;60:485-97. Erratum in: J Korean Neurosurg Soc 2019;62:366. [Crossref] [PubMed]