Gait velocity (walking speed) is an indicator of spine health, and objective measure of pre and post intervention recovery for spine care providers
Walking is a fundamental part of living dependent on the function and interaction of the visual, mechanical and neurological health of the individual (1). Its importance is not limited by age, race or medical status. Reduced walking speed, or gait velocity (GV) is a sign of advancing age, poor response to rehabilitation, age-related diseases, cardiovascular disease, dementia, and early mortality (2). A deterioration in how we walk, including reduced GV, is associated with poor health outcomes, including spinal health (3). GV is of such importance that it has been dubbed “the 6th vital sign” (1).
There is nominal literature linking walking metrics, including GV, with assessment of disability and post intervention recovery of the spine patient. Walking serves as an important objective measure of our spine health, free of the subjective bias inherent in patient reported outcome measures (4). The importance of GV is well documented for general health outcomes, however is now gaining increased interest in the spine arena. This includes:
- Lumbar spinal stenosis (4-6). A number of articles have recently documented the use of GV as powerful metric in the assessment of the patient with Lumbar Spinal Stenosis, and identified this metric as a relevant tool for the objective measurement of outcome and recovery.
- Lumbar disc herniation (7). There is a significant correlation between gait parameters including GV, and functional disability in patients with Lumbar Disc Herniation. However, data is lacking on the use of this metric for post intervention recover following microdiscectomy, and this requires further investigation.
- Identification of complications post spinal surgery (8). Wearable devices measuring gait, including GV, have been used not only as a research tool, but in the remote monitoring of patients’ post-surgery for continuous assessment of recovery. There is a case report of remote monitoring to identify a complication post microdiscectomy with patient contact for relevant imaging and further intervention. This is a landmark publication and reveals the future of smart devices to assist in the automation of patient management.
- Low back pain (9). Pain intensity can negatively affect spatiotemporal gait parameters, in particular GV, in patients with Low Back Pain, such as discogenic or facetogenic pain generators. Further studies are required to document relevant improvements in gait metrics following interventions such as injection therapies, physical therapy or indeed surgery.
- Cervical myelopathy (10). Patients with cervical myelopathy have a slower GV and reduced cadence compared with healthy controls. Surgical decompression improves clinical outcomes and GV, and is a relevant indicator of recovery.
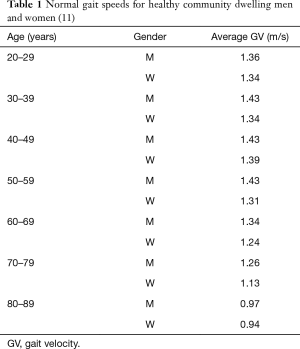
This commentary highlights the importance of GV to record decline and recovery of various common spinal disorders, and reveals why spine care providers should add this metric to the initial assessment, and ongoing care of the spine patient. Table 1 identifies the “normal” walking speeds of male vs. female at various age categories (11). This data can be used by the spine care provider to assist with identifying the degree of disability of a patient on initial presentation to the clinic. GV can be recorded using either observational tools (12) in the clinic setting (timed walk along a known distance with step count), or using wearable devices (3,4,6).
There are multiple stakeholders interested in objective, non-biased, patient assessment. These include governments, hospitals, insurance providers, medical companies, physicians, surgeons and the patients themselves. Traditionally the use of subjective assessment tools has been difficult and costly to administer; fraught with bias, compliance and timing issues to name a few. It is the responsibility of the spine care provider to demonstrate benefit of a given intervention. As spine surgeons and providers of spine care, we must accept the impending transition phase from the ‘subjective’ to the ‘objective’ era of patient assessment.
In addition to the above, future applications of objective gait assessment for the monitoring of spine patients will likely expand rapidly in a post COVID-19 world. The role of telehealth and remote patient monitoring using wearable devices to evaluate overall health and gait, to provide assessment and care of the spine patient (13), and assist with complex decision making (14), represents the next phase of patient care in our speciality. Based on these summarized findings and expanding literature on this topic, we encourage spinal surgeons to consider the addition of gait analysis to expand their outcome assessment and objectivity measure pre and post intervention progress.
How we walk is a summary index of our health, and key indicator of disability, decline and recovery.
Acknowledgments
The author would like to thank the WAGAR (Wearables and Gait Assessment Research Group) and the NSURG Research Group: Callum Betteridge, Luke Sy, Monish Maharaj, Wei Jie Choy, Kaitlin Rooke, Nicole Kah Mun Yoong, Lauren Simpson and Jordan Perring.
Funding: None.
Footnote
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss-20-602). RJM serves as an unpaid Editor-in-Chief of Journal of Spine Surgery from Sep 2015 to Sep 2025.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Fritz S, Lusardi M. White paper: "walking speed: the sixth vital sign J Geriatr Phys Ther 2009;32:46-9. [Crossref] [PubMed]
- Rasmussen LJH, Caspi A, Ambler A, et al. Association of neurocognitive and physical function with gait speed in midlife. JAMA Netw Open 2019;2:e1913123. [Crossref] [PubMed]
- Mobbs RJ. Wearables in spine surgery: Beginnings, research and real-world applications. Spinal News International, 2017. Available online: https://spinalnewsinternational.com/wearables/
- Mobbs RJ, Mobbs RR, Choy WJ. Proposed objective scoring algorithm for assessment and intervention recovery following surgery for lumbar spinal stenosis based on relevant gait metrics from wearable devices: the Gait Posture index (GPi). J Spine Surg 2019;5:300-9. [Crossref] [PubMed]
- Grelat M, Gouteron A, Casillas JM, et al. Walking speed as an alternative measure of functional status in patients with lumbar spinal stenosis. World Neurosurg 2019;122:e591-7. [Crossref] [PubMed]
- Chakravorty A, Mobbs RJ, Anderson DB, et al. The role of wearable devices and objective gait analysis for the assessment and monitoring of patients with lumbar spinal stenosis: systematic review. BMC Musculoskelet Disord 2019;20:288. [Crossref] [PubMed]
- Zheng CF, Liu YC, Hu YC, et al. Correlations of Japanese Orthopaedic Association Scoring Systems with gait parameters in patients with degenerative spinal diseases. Orthop Surg 2016;8:447-53. [Crossref] [PubMed]
- Mobbs RJ, Katsinas CJ, Choy WJ, et al. Objective monitoring of activity and Gait Velocity using wearable accelerometer following lumbar microdiscectomy to detect recurrent disc herniation. J Spine Surg 2018;4:792-7. [Crossref] [PubMed]
- Bonab M, Colak TK, Toktas ZO, et al. Assessment of spatiotemporal gait parameters in patients with lumbar disc herniation and patients with chronic mechanical low back pain. Turk Neurosurg 2020;30:277-84. [PubMed]
- Haddas R, Lieberman I, Arakal R, et al. Effect of cervical decompression surgery on gait in adult cervical spondylotic myelopathy patients. Clin Spine Surg 2018;31:435-40. [PubMed]
- Bohannon RW, Williams Andrews A. Normal walking speed: a descriptive meta-analysis. Physiotherapy 2011;97:182-9. [Crossref] [PubMed]
- Mobbs RJ, Katsinas CJ, Choy WJ, et al. Analysis of Gait metrics in the clinic setting, and comparison with normative values. Canberra: Proceedings of the Spine Society of Australia, 2019.
- Mobbs RJ, Phan K, Maharaj M, et al. Physical activity measured with accelerometer and self-rated disability in lumbar spine surgery: a prospective study. Global Spine J 2016;6:459-64. [Crossref] [PubMed]
- Mobbs RJ, Phan K, Malham G, et al. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg 2015;1:2-18. [PubMed]