
Early experience of single level full endoscopic posterior cervical foraminotomy and comparison with microscope-assisted open surgery
Introduction
Cervical radiculopathy is known as a common disease-causing neck and arm pains, and arm weakness, typically due to nerve root compression by intervertebral disc herniation or foraminal stenosis (1,2). Surgical decompression may become necessary if conservative managements fail or if there is severe arm weakness.
Posterior cervical foraminotomy (PCF) was initially described in 1940s (3), and various modifications were developed such as microscope-assisted or endoscope-assisted keyhole foraminotomy (4,5). Although satisfactory relief of symptoms can be achieved by these conventional methods, there are some disadvantages due to traumatization of surgical access, such as postoperative neck and shoulder pain (6).
With minimally invasive theories and techniques evolving in the field of spine surgery, full endoscopic PCF (FEPCF) has been introduced by Ruetten et al. in 2007 (7). They stated the advantages of FEPCF: facilitation for surgeons by excellent presentation of the anatomic structures, good illumination and expanded field of vision, reduced traumatization and bleeding, monitor image as the basis for training of assistants, rapid rehabilitation and high patient acceptance. However, there are some significant disadvantages: limited possibilities to expand the operation in the event of unforeseen hindrances and steep learning curve (7,8).
The objective of this study to examine the technical feasibility of FEPCF for beginners of full endoscopic spine surgeries and comparison the outcomes of FEPCF with those of microscope-assisted open PCF (OPCF).
Methods
This study was conducted in accordance with the Declaration of Helsinki and the Harmonized Tripartite Guideline for Good Clinical Practice from the International Conference on Harmonization. The study was approved by the ethical committee of Sapporo Teishinkai Hospital, approval number 2020-03. All patients enrolled completed the informed consent form.
Fourteen patients, diagnosed as single level cervical spondylotic radiculopathy, using symptoms, physical examinations and findings of plain X-rays, magnetic resonance (MR) imagings and neurograms, and computed tomographies (CT), were included in this study. All patients failed with conservative managements including such as pain medications, neck collar orthoses, epidural and/or nerve root block, or developed deteriorating arm weakness, which led to surgical interventions. Nerve root blocks were added to confirm the affected nerve root level, if it was difficult to determine from physical examination and radiographic findings. Patients were assigned to OPCF before January 2019 and to FEPCF after February 2019 (seven cases each) because of the surgeon’s technical feasibility. OPCFs were performed by the single surgeon (MA) without assistants, and FEPCFs were carried out by the first author (MA) under the supervision of the second author (HK).
Operative technique
OPCF
Under general anesthesia, the head was fixed in place with Mayfield clamps in prone position. A 2.5 cm midline incision was made, paravertebral muscles were detached from spinous processes to expose affected facet level. After confirmation of correct surgical level with portable X-ray image, the caudal side of the inferior articular process of the upper vertebra and the cranial side of the superior articular process were resected using high-speed surgical electric motor drills (NSK-Nakanishi Japan, Tokyo, Japan) under magnification of surgical loupes and microscope. Decision of optimal nerve root decompression was made by smooth insertion of Penfield dissectors. Skin closure was performed with a drainage tube. The patients were allowed to walk 6 hours after surgery without any cervical orthoses.
FEPCF
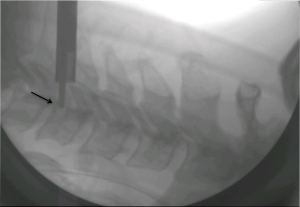
Under general anesthesia, the head was fixed with tape without using Mayfield clamps in prone position and C arm fluoroscopy was placed. An 8-mm longitudinal skin incision was done approximately 15 mm lateral to the midline of the vertebral level operated. A 7-mm-diameter outer sheath was placed on the cervical lamina after splitting paravertebral muscles. Under a 7-mm diameter spinal full-endoscopic system (Richard Wolf GmbH, Knittlingen, Germany) with continuous irrigation (set at 180 cmH2O), and the same procedure as OPCFs was carried out using high-speed drill with a diameter of 3.5 mm (NSK-Nakanishi Japan, Tokyo, Japan). Decision of optimal nerve root decompression was made when Penfield dissector went over to the posterior border of vertebral body with lateral fluoroscopy (Figure 1). Skin closure was performed without a drainage tube. The patients were allowed to walk 3 hours after surgery without any cervical orthoses.
Oral acetaminophen and muscle relaxant were given three times a day for 3 days, and non-steroid anti-inflammatory drugs (NSAIDs), which were given in intravenous, suppository or oral, were used as patients needed.
Data collection and statistical analysis
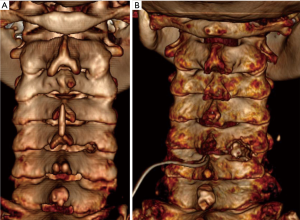
Oswestry neck disability index (ONDI) was examined by a written form before and 1 month after surgery, and was evaluated by improvement ratio. Operating time, numerical rating scale (NRS) of postoperative neck and arm pain at day 1–3, and usage of postoperative PRN pain medications were collected from medical records. Foraminotomy areas were calculated with 3D reconstruction of postoperative CT images using Horos DICOM viewer software (Figure 2A,B). Descriptive statistics were presented as means and standard deviation and Mann-Whitney U-test was applied for the comparison of two groups (FEPCF vs. OPCF). A positive significance level was assumed at probability of less than 0.05.
Results
Fourteen patients, single level PCFs underwent, were included in this study. Mean age was 52.5 [35–78] and 28.6% were female and 71.4% were male. The surgical level was 4 cases for C5/6, 3 cases for C6/7 in the FEPCF group, and 3 cases for C4/5, 3 cases for C5/6, and 1 case for C6/7 in the OPCF group.
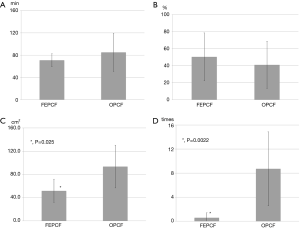
The mean operating time was 70.9±11.6 minutes in the FEPCF group, 85.0±34.1 minutes in the OPCF group, and statistically not different (P=0.37) (Figure 3A). Improvement ratio of ONDI was 50.4±28.2 in the FEPCF group, 41.0±28.2 in the OPCF group, and statistically not different (P=0.72) (Figure 3B). Foraminotomy area in the FEPCF group (51.67±20.07 cm2) was significantly smaller (P=0.025) than that in the OPCF group (93.47±36.82 cm2) (Figure 3C). NRS of postoperative neck and would pain at day 1–3 in the FEPCF group (3.1±1.5) was significantly smaller (P=0.019) than that in the OPCF group (6.4±2.1), meanwhile, postoperative arm pain was not significantly different between the groups (2.3±0.8 vs. 2.1±0.7, P=0.69). PRN medication usage after surgeries in the FEPCF group (0.57±0.82) was significantly less (P=0.0022) than that in the OPCF group (8.71±6.15) (Figure 3D). There were no serious complications like postoperative bleeding, injury to the nerve or dura, damage to the spinal cord with paresis or paralysis of upper extremities.
Discussion
In this study, we presented our early experience of FEPCF and compared the results with microscope assisted OPCF. FEPCF has been introduced to reduce traumatization of surgical access in the treatment of lateral disc herniation first (8), and then, extended its application to bony stenosis of intervertebral foramen (9), as effective as conventional, microscope- or endoscope- assisted PCF. FEPCF is technically feasible and minimally invasive treatment option for lateral pathologies of cervical spine, however, steep learning curve has been pointed out as one of the disadvantages. To overcome this steep learning curve, the first author (MA) has mastered microscope-assisted OPCF, practiced full endoscopic spine surgeries including lumbar discectomy (transforaminal and interlaminar approach) and PCF with cadavers several times, assisted 15 full endoscopic spine surgery of an expert endoscopic spine surgeon (HK), started full endoscopic spine surgery as a surgeon, first three cases for lumbar pathologies and then applied to FEPCF, under supervision of HK.
Duration of operating time was not statistically different between the two methods, there were no serious complications in both ways, and FEPCF was as effective as OPCF in terms of neck and arm pain relief at 1 month after surgery. These results suggest that although learning curve of FEPCF is steep, it could be feasible and as effective as OPCF in the beginning stage of full endoscopic spine surgery career under supervision of an expert surgeon.
All of FEPCF patients were allowed and able to walk 3 hours after surgery. All of OPCF patients were allowed to walk 6 hours after surgery, however, some of them started to walk at day 1 with help of PRN pain medications. NRS of postoperative wound pain in the FEPCF group was 3.1 (ranged, 2–6), significantly smaller than that in the OPCF group, 6.4 (ranged, 2–8). Postoperative PRN pain medication usage in the FEPCF group was only 0.57 (ranged, 0–2) times far less than that in the OPCF group, 8.71 [2–20] times. Early ambulation and least surgery related neck pain are considered to be huge advantage of FEPCF due to less surgical access traumatization over OPCF.
Calculated foraminotomy areas in the FEPCF group were approximately 45% (51.67 vs. 93.47 cm2) smaller than those in the OPCF group. FEPCF had clear and expanded surgical field vision, which led to super key-hole foraminotomy, start drilling from the crossing point (X-point) of facet joints. In addition, FEPCF had clear end point of decompression, which a dissector went over the posterior margin of vertebral body in the lateral fluoroscopy shot (Figure 1), rather than surgeon’s feeling of smooth insertion of a dissector in the case of OPCF, which led to avoid unnecessary bone removal.
In conclusion, FEPCF is technically feasible and as effective as OPCF with early rehabilitation and smaller foraminotomy, for surgeons in the early stage of full endoscopic spine surgery under well-prepared conditions. We suggest that full endoscopic surgery beginners should practice basic endoscopic manipulations with cadavers, start from transforaminal and interlaminar lumbar pathologies for first several cases, and then advance to FEPCF with an expert endoscopic surgeon. However, the surgeons must have mastered open and maximally invasive procedures in order to deal with problems or complications in full endoscopic surgery. In addition, this method is rather a supplement and alternative option than replacing standard surgeries (7).
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Hisashi Koga and Alf Giese) for the series “Full-endoscopic Spine Surgery” published in Journal of Spine Surgery. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss-20-491). The series “Full-endoscopic Spine Surgery” was commissioned by the editorial office without any funding or sponsorship. HK served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Journal of Spine Surgery from Oct 2018 to Oct 2020. The other author has no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki and the Harmonized Tripartite Guideline for Good Clinical Practice from the International Conference on Harmonization. The study was approved by the ethical committee of Sapporo Teishinkai Hospital, approval number 2020-03. All patients enrolled completed the informed consent form.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Woods BI, Hilibrand AS. Cervical radiculopathy: epidemiology, etiology, diagnosis, and treatment. J Spinal Disord Tech 2015;28:E251-9. [Crossref] [PubMed]
- Iyer S, Kim HJ. Cervical radiculopathy. Curr Rev Musculoskelet Med 2016;9:272-80. [Crossref] [PubMed]
- Spurling RG, Scoville WB. Lateral rupture of the cervical intervertebral discs. A common cause of shoulder and arm pain. Surg Gynecol Obstet 1944;78:350-8.
- Maroon JC. Current concepts in minimally invasive discectomy. Neurosurgery 2002;51:S137-45. [Crossref] [PubMed]
- Chiu JC, Clifford T, Princenthal R, et al. Junctional disc herniation syndrome in post spinal fusion treated with endoscopic spine surgery. Surg Technol Int 2005;14:305-15. [PubMed]
- Hosono N, Yonenobu K, Ono K. Neck and shoulder pain after laminoplasty. A noticeable complication. Spine (Phila Pa 1976) 1996;21:1969-73. [Crossref] [PubMed]
- Ruetten S, Komp M, Merk H, et al. A new full-endoscopic technique for cervical posterior foraminotomy in the treatment of lateral disc herniations using 6.9-mm endoscopes: prospective 2-year results of 87 patients. Minim Invasive Neurosurg 2007;50:219-26. [Crossref] [PubMed]
- Ruetten S, Komp M, Merk H, et al. Full-endoscopic cervical posterior foraminotomy for the operation of lateral disc herniations using 5.9-mm endoscopes: a prospective, randomized, controlled study. Spine (Phila Pa 1976) 2008;33:940-8. [Crossref] [PubMed]
- Ohmori K, Ono K, Hori T. Outcomes of full-endoscopic posterior cervical foraminotomy for cervical radiculopathy caused by bony stenosis of the intervertebral foramen. Mini-invasive Surg 2017;1:63-8. [Crossref]


