
The relationship between measures of spinal deformity and measures of thoracic trunk rotation
Introduction
The term scoliosis describes a deformity of the spine and is defined by a lateral bend of the spine greater than 10° (1) with associated vertebral rotation (2). The magnitude of a scoliosis is measured using the Cobb angle (3) and the measurement of vertebral body rotation (VBR) can be performed using both two-dimensional (2D) radiographs or three-dimensional (3D) cross-sectional imaging (4-6). The most prevalent subtype of scoliosis is adolescent idiopathic scoliosis (AIS) seen between the ages of 10 and 18 years (7). AIS can present with asymmetry of the torso and it is recognised that AIS may have a significant impact on the patient’s emotional and mental state (8-10). It is thought that the rib hump, a difference in the size of the posterior hemithorax between the left and right sides, is partly a consequence of axial rotation of the vertebral body (11).
A method that is used to investigate the shape of the posterior torso is the scoliometer, which is a device similar to a spirit level, that measures the angle of trunk rotation (12) when the patient is in the Adams’ forward bending position. The scoliometer was first described by Bunnell who, after a review of 1,065 children, identified 5° as the angle of trunk rotation (ATR) which indicated the possibility of an underlying scoliosis, with a curvature of 20° or more (12). Surface topography is another method of analysing torso asymmetry, giving the 3D locations of a wide range of points on the back. This information then allows a quantitative assessment of asymmetry and shape. One such surface topography system used for assessment of back shape is the Integrated Shape Imaging System 2 (ISIS2) (13). It is a radiation free system, using Fourier transform profilometry to analyse a 2D photograph which generates a 3D surface from which the shape of both the spine and the torso are assessed. ISIS2 has been used for both research and clinical management of scoliosis over the past decade (13-15). One of the parameters generated by ISIS2 is the ‘maximum skin angle (MSA)’. The MSA is a measure of the asymmetry of the back, much in the same way as measured by scoliometer. The difference is that the scoliometer measure is taken in the forward bend position, whereas MSA is a measure taken in upright stance.
The aims of scoliosis surgery in AIS include limiting the progression of the curve together with providing the patient with as symmetrical a torso as possible through the maximum ‘safe’ correction of the deformity (16,17). Surgery for scoliosis correction uses techniques that can include vertebral column de-rotation (8,18). It remains unclear how de-rotating vertebral bodies during scoliosis surgery affects the shape and size of the rib hump.
In this paper, it is hypothesised that there is a relationship between the size of the rib hump and the amount of VBR. We present the following article in accordance with the STROBE reporting checklist (available at: http://dx.doi.org/10.21037/jss-20-562).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical approval for this study was received from NRES committee East Midlands, Northampton (15/EM/0283). Because of the retrospective nature of the research, the requirement for informed consent was waived.
This is a retrospective analysis of prospectively collected data of patients undergoing investigation for AIS from one specialist centre. The cohort of patients collected had not undergone any prior spinal surgical intervention at the time of presentation and the individuals reported on here had all measurements taken before any surgery was considered.
As is standard care for this group in this institution, all patients had both radiographs and surface topography imaging at each planned attendance to the hospital. Also, it is the protocol of the hospital that all patients with AIS undergo an MRI scan (unless contra-indicated) of the whole spine and neural axis to confirm the diagnosis of AIS and rule out any intra-dural anomalies that could be associated with scoliosis (19,20). As part of this imaging, axial slices of the apex of the deformity are a routine imaging series, specifically performed to look for the presence of a syrinx in the spinal cord at the apex.
The inclusion criteria for this study were a diagnosis of AIS, aged between 10 and 18 years of age, with a minimum 2-year follow up from initial consultation and a contemporaneous set of radiographs, ISIS2 surface topography and axial imaging. All three imaging modalities were required to be taken within a 6-week period of one another for inclusion in this study. To prevent any error that might occur from the combination of data from both right and left sided deformities, only patients with a rib hump more prominent on the right, as indicated by a positive MSA, a convex to the right scoliosis curve and VBR to the right were included. Patients were also included based on their Lenke curve classification coronal subtype. Only Lenke curve coronal subtypes one to four were analysed, as those curve types include the presence of a significant major thoracic component, while curve types five and six were excluded as they do not.
Patients were excluded if there was an identifiable cause for scoliosis that ruled out the diagnosis of AIS. Exclusion was also performed if there was an intra-dural anomaly on the MRI scan or an incomplete data set, including where axial imaging did not include the apex of the main curve.
For all identified patients, whole spine radiographs had been taken in a standardised weight-bearing position. The radiograph was used to measure the Cobb angle (3) and to classify the scoliosis using the Lenke classification (21) (Table 1).
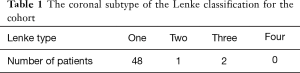
Full table
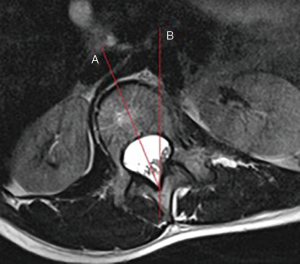
All MRI axial imaging was performed in the supine position. Maximal VBR was measured using the technique described by Aaro and Dahlborn (5). This measures the amount of rotation of the vertebral body from the anatomical position in the axial plane (Figure 1).
ISIS2 surface topography was carried out at each clinic visit using a standardised method as described by Berryman et al. (13). The surface topography image was taken in upright stance in the same fashion as the radiograph. The parameter of MSA is automatically generated and recorded as part of that assessment (Figure 2).

Data were analysed using the statistical programme R (22). Linear regression was used to identify the relationship between the variables. The coefficient of determination (R2) was used to assess the amount that one variable affected the other. Also, P values were calculated to assign statistical significance to the relationship. A P value of <0.05 was pre-defined as statistically significant. All data sets were examined for normality using the Kolmogorov-Smirnov test (23) calculated using SPSS Statistics Version 25 (2017, IBM Corporation).
Results
The ISIS2 database contained 1,548 individual images. There were 51 datasets from 51 patients that met our inclusion criteria. The majority of these exclusions were because of the time between the topographic and radiographic imaging and the cross-sectional imaging was greater than six weeks.
There were 45 females and 6 males. The mean age of the cohort was 14.6 years (SD 1.4, range, 11.2 to 17.7).
The mean, median, standard deviation, interquartile range and range of the Cobb angle from the radiographs, the MSA from ISIS2 surface topography and the angle of VBR from the axial imaging are shown in Table 2.

Full table
Kolmogorov-Smirnov test showed that all continuous data was normally distributed. The R2 and P values for the relationships examined between Cobb angle, MSA and VBR are shown in Table 3.
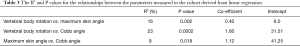
Full table
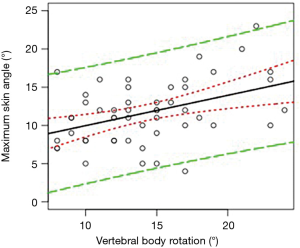
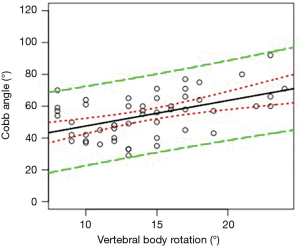
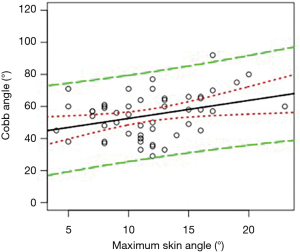
Figures 3-5 demonstrate the linear regression lines of best fit along with the outer 95% confidence limits of prediction and the inner 95% confidence limits of the line of best fit. Figure 3 is a regression of VBR against MSA, Figure 4 VBR against Cobb angle and Figure 5 MSA against Cobb angle. The R2 and p values for all of the relationships are also quoted.
A multiple linear regression model was created using all the parameters measured; however, this did not increase the statistical significance of the model and was therefore not felt helpful in explaining the relationships seen.
Examining the data using orthogonal regression techniques did not reveal a better fit for the regression equation in any of the relationships.
Discussion
This paper examines the relationship between vertebral rotation and rib hump in AIS. Whilst statistically significant, the low R2 values demonstrate that there is a poor relationship between VBR and the size of the rib hump (24). The relationship between VBR and the size of the scoliosis is also poor (24). The work here also shows that the relationship between rib hump size and the size of the scoliosis is poor (24).
These results suggest that the size of the rib hump and the amount of VBR have little dependence on one another. If VBR is not well associated with rib hump size, doubt is then cast as to the efficacy of surgical de-rotation of the vertebral column at reducing the size of the rib hump, and suggests that there are other, yet to be defined, factors to be accounted for.
The strengths of this work are the use of the MSA and maximum VBR, irrespective of the anatomical level, with respect to the spine, of either parameter. Whilst it would be wrong to claim that these are always the same anatomical spinal level, if the notion that one leads to the other is true, then anatomical difference should not matter.
The use of the fully automated ISIS2 surface topography for the measurement of MSA has removed the measurement error associated with manual measurement (13). All individuals in this series had undergone axial imaging and had 2 year follow up, so there was no loss due to incomplete data or loss to follow up.
It is accepted that one of the limitations of the study is the fact that only 51 of a possible 1548 were included for final analysis. This was directly related to the stringent inclusion criteria pertaining to timing between radiograph, ISIS2 topography and cross-sectional imaging. This was because of concern that a greater time period for the imaging studies risked iatrogenic error where the curve may have changed in shape and size. This may have led to erroneous conclusions. Despite this we believe that the conclusions drawn here are broadly applicable to the wider AIS population. It is also noted that the axial imaging is in the supine position and this may have an effect on the degree of VBR when compared to the amount in the upright position (5,25,26). It is not possible to routinely obtain cross sectional imaging in the upright position in our institution.
Currently there is sparsity in the literature as to whether or not a relationship exists between the rib hump and VBR. In 1976, Thulbourne et al. (27) examined the linear relationships between rib hump and axial rotation of the vertebrae. Axial rotation was measured using radiographs and the authors determined that there was no linear relationship between the rib hump and the rotation of the vertebral body, although the authors did comment on a “minor irregular relationship” existing.
In his 2007 paper, Grivas et al. (28) described the development of the rib hump which may occur prior to the development of scoliosis and indicated that these features may have less association than had previously been thought.
Reduction of the size of the hump is felt to be important by the patient, as reported by Smith et al. (29), Howard et al. (30) and Misterska et al. (31). Modern techniques for the posterior correction of scoliosis can use de-rotation manoeuvres of the vertebral column to affect a correction (32). This can be performed through a variety of methods that are described by Chang and Lenke (33). Through manipulation of the spine, an attempt is made to reduce the size of the rib-hump, thus reducing asymmetry and improving cosmesis (29,34). The work presented here raises the question of whether or not current surgical methods involving de-rotation of the vertebral column actually address the problem that can affect the patient—namely the thoracic rib hump. If surgery is going to reduce the size of the rib-hump through spinal de-rotation then it would be important to demonstrate that VBR is associated with thorax asymmetry and rotation.
This study leads on to further investigations in this field. First would be to assess the association between rib hump and vertebral body rotation through serial measures over time of the same individual with AIS who had not undergone surgery, to allow analysis in a longitudinal fashion. Second would be to compare the relationship of scoliosis correction with the size of the rib hump, measured both pre and post-operatively, using surgical techniques that do or do not include vertebral column de-rotation and then correlation with the use of established outcome scores such as the Scoliosis Research Society-22 questionnaire (35). An assessment of the patient’s own view of their own shape using a tool such as the Spinal Assessment Questionnaire (10) or the Trunk Appearance Perception Scale (36) would also be of use, in order to establish whether or not thoracic rib hump correction, or lack thereof, impacts the patient’s perception of their deformity.
Conclusions
The work presented here shows that there are only poor relationships between the size of the curve, the amount of vertebral body rotation and the size of the rib hump in AIS.
Acknowledgments
Funding: Funding was received from the Birmingham Orthopaedic Charity for the completion of this study.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at: http://dx.doi.org/10.21037/jss-20-562
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jss-20-562
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss-20-562). The authors have no conflict of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical approval for this study was received from NRES committee East Midlands, Northampton (15/EM/0283). Because of the retrospective nature of the research, the requirement for informed consent was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kane WJ. Scoliosis prevalence: a call for a statement of terms. Clin Orthop 1977.43-6. [PubMed]
- Janicki JA, Alman B. Scoliosis: Review of diagnosis and treatment. Paediatr Child Health 2007;12:771-6. [Crossref] [PubMed]
- Cobb J. Outline for the study of scoliosis. AAOS Instr Cours Lec 1948;5:261-75.
- Nash CL, Moe J. A study of vertebral rotation. J Bone Joint Surg Am 1969;51:223-9. [Crossref] [PubMed]
- Aaro S, Dahlborn M. Estimation of vertebral rotation and the spinal and rib cage deformity in scoliosis by computer tomography. Spine 1981;6:460-7. [Crossref] [PubMed]
- Lam GC, Hill D, Le L, et al. Vertebral rotation measurement: a summary and comparison of common radiographic and CT methods. Scoliosis 2008;3:16. [Crossref] [PubMed]
- James JI. Idiopathic scoliosis: the prognosis, diagnosis, and operative indications related to curve patterns and the age at onset. J Bone Joint Surg Br 1954;36-B:36-49. [Crossref] [PubMed]
- Sheehan DD, Grayhack J. Pediatric scoliosis and kyphosis: an overview of diagnosis, management, and surgical treatment. Pediatr Ann 2017;46:e472-80. [Crossref] [PubMed]
- Talić G, Ostojić L, Bursać SN, et al. Idiopathic scoliosis from psychopathological and mind-body medicine perspectives. Psychiatr Danub 2016;28:357-62. [PubMed]
- Sanders JO, Harrast J, Kuklo T, et al. The Spinal Appearance Questionnaire: results of reliability, validity, and responsiveness testing in patients with idiopathic scoliosis. Spine 2007;32:2719-22. [Crossref] [PubMed]
- Aaro S, Dahlborn M. The longitudinal axis rotation of the apical vertebra, the vertebral, spinal, and rib cage deformity in idiopathic scoliosis studied by computer tomography. Spine 1981;6:567-72. [Crossref] [PubMed]
- Bunnell WP. An objective criterion for scoliosis screening. J Bone Joint Surg Am 1984;66:1381-7. [Crossref] [PubMed]
- Berryman F, Pynsent P, Fairbank J, et al. A new system for measuring three-dimensional back shape in scoliosis. Eur Spine J 2008;17:663-72. [Crossref] [PubMed]
- Brewer P, Berryman F, Baker D, et al. Influence of Cobb angle and ISIS2 surface topography volumetric asymmetry on Scoliosis Research Society-22 outcome scores in scoliosis. Spine Deform 2013;1:452-7. [Crossref] [PubMed]
- Gardner A, Berryman F, Pynsent P. A description of three-dimensional shape of the posterior torso comparing those with and without scoliosis. Symmetry 2019;11:211. [Crossref]
- The Scoliosis Research Society. E-Textbook [Internet]. Scoliosis Research Society, 2015.
- Lonstein JE, Carlson J. The prediction of curve progression in untreated idiopathic scoliosis. J Bone Joint Surg Am 1984;66:1061-71. [Crossref] [PubMed]
- Lee SM, Suk SI, Chung ER. Direct vertebral rotation: a new technique of three-dimensional deformity correction with segmental pedicle screws fixation in adolescent idiopathic scoliosis. Spine 2004;29:343-9. [Crossref] [PubMed]
- Dewan V, Gardner A, Forster S, et al. Is the routine use of magnetic resonance imaging indicated in patients with scoliosis? J Spine Surg 2018;4:575. [Crossref] [PubMed]
- Singhal R, Perry D, Prasad S, et al. The use of routine preoperative magnetic resonance imaging in identifying intraspinal anomalies in patients with idiopathic scoliosis: a 10-year review. Eur Spine J 2013;22:355-9. [Crossref] [PubMed]
- Lenke LG, Betz R, Harms J, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am 2001;83:1169-81. [Crossref] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing [Internet]. Vienna, Austria; 2016. Available online: https://www.R-project.org/
- Massey FJ Jr. The Kolmogorov-Smirnov test for goodness of fit. J Am Stat Assoc 1951;46:68-78. [Crossref]
- Jackson S. Research methods and statistics: A critical thinking approach. Cengage Learning; 2015.
- Yazici M, Acaroglu E, Alanay A, et al. Measurement of vertebral rotation in standing versus supine position in adolescent idiopathic scoliosis. J Pediatr Orthop 2001;21:252-6. [Crossref] [PubMed]
- Janssen MM, Vincken K, Kemp B, et al. Pre-existent vertebral rotation in the human spine is influenced by body position. Eur Spine J 2010;19:1728-34. [Crossref] [PubMed]
- Thulbourne T, Gillespie R. The rib hump in idiopathic scoliosis. Measurement, analysis and response to treatment. J Bone Joint Surg Br 1976;58:64-71. [Crossref] [PubMed]
- Grivas T, Vasiliadis E, Savvidou O, et al. Is the rib hump (thoracic/surface deformity) always in agreement with the Cobb angle (spinal/radiological deformity)? A study in school-screening referrals, with aetiological implications. Scoliosis 2007;2:S30. [Crossref]
- Smith PL, Donaldson S, Hedden D, et al. Parents’ and patients’ perceptions of postoperative appearance in adolescent idiopathic scoliosis. Spine 2006;31:2367-74. [Crossref] [PubMed]
- Howard A, Donaldson S, Hedden D, et al. Improvement in quality of life following surgery for adolescent idiopathic scoliosis. Spine 2007;32:2715-8. [Crossref] [PubMed]
- Misterska E, Glowacki M, Latuszewska J, et al. Perception of stress level, trunk appearance, body function and mental health in females with adolescent idiopathic scoliosis treated conservatively: a longitudinal analysis. Qual Life Res 2013;22:1633-45. [Crossref] [PubMed]
- Miller D, Cahill P, Vitale M, et al. Posterior correction techniques for adolescent idiopathic scoliosis. J Am Acad Orthop Surg 2020;28:e363-73. [Crossref] [PubMed]
- Chang M, Lenke L. Vertebral derotation in adolescent idiopathic scoliosis. Oper Techn Orthop 2009;19:19-23. [Crossref]
- Theologis TN, Jefferson R, Simpson A, et al. Quantifying the cosmetic defect of adolescent idiopathic scoliosis. Spine 1993;18:909-12. [Crossref] [PubMed]
- Haher TR, Gorup J, Shin T, et al. Results of the Scoliosis Research Society instrument for evaluation of surgical outcome in adolescent idiopathic scoliosis: a multicenter study of 244 patients. Spine 1999;24:1435. [Crossref] [PubMed]
- Bago J, Sanchez-Raya J, Perez-Grueso F, et al. The Trunk Appearance Perception Scale (TAPS): a new tool to evaluate subjective impression of trunk deformity in patients with idiopathic scoliosis. Scoliosis 2010;5:6. [Crossref] [PubMed]


