Prospective analysis of radiofrequency denervation in patients with chronic low back pain
Introduction
Low back pain is currently a major health problem that represents a significant socioeconomic cost in Western societies and is associated with higher rates of disability than any other disorder (1).
Although the majority of cases are treated successfully at a primary care level, it is estimated that around 15% become chronic, resisting conservative treatment (low back pain is considered to be chronic after 3 months) (2).
Numerous potential causes of low back pain are known, including facet joints (prevalence of 15–45%) (3) sacroiliac joints, intervertebral discs or paravertebral muscles, although the cause is often mixed (2). The origin of this pain is therefore an essential step when treating patients with low back pain.
The success of the numerous therapeutic options available for managing low back pain, including intra-articular corticosteroid injections, anaesthetic nerve block, or radiofrequency denervation, also known as rhizolysis, which is the subject of this review, varies widely (4).
Rhizolysis, which is a minimally invasive treatment, is increasingly being used for chronic low back pain, as illustrated by the fact that, in the USA, the number of such interventions increased markedly from 425,000 in 2000 to 2.2 million in 2013 (1), thus representing the second most common procedure performed at centres specialising in pain treatment (3).
The aim of radiofrequency denervation is to generate small lesions in the nerves responsible for transmitting pain impulses from the site where low back pain originates to the central nervous system. These lesions are produced by inserting a radio frequency cannula percutaneously, under fluoroscopy control, which, after coming into contact with the nerve structure responsible for transmitting the pain impulse, generates a thermal lesion. Prior to performing this procedure, those patients with a greater probability of benefiting from it must be selected on the basis of a full physical examination, complementary imaging tests and/or the performance of an anaesthetic nerve block (1).
Despite its widespread use, the majority of studies and reviews have only a low to moderate evidence level as regards effectiveness, safety and need for a prior anaesthetic block, and quality studies that provide a high evidence level are lacking. Our study has a bigger sample size and longer follow-up than most of the revised bibliography. Besides, it provides a deeper analysis of the evolution OS the patients throughout their follow-up.
We present the following article/case in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jss-20-599).
Methods
A prospective analytical study involving a series of 100 patients who underwent a radiofrequency procedure for facet joint-related chronic low back pain at the Hospital Universitario de Cabueñes (Spain) between May 2016 and February 2019.
The inclusion criteria were adult patients who were able to understand the procedure to be performed, with low back pain for at least 12 months (including cases refractory to outpatient treatment and resistant to rehabilitation or physiotherapy treatment) originating in the facet joints, as confirmed by a physical examination and magnetic resonance (MR).
Chronic low back pain originating in the facet joints was defined by Pérez-Cajaraville et al. (5) as low back pain radiating to the buttocks, groin or hips in a non-specific manner to lower limbs but never to the feet, this pain increasing upon prolonged standing and sitting, sharp pain upon palpation of the zygapophyseal joint (ZPJ), decreased lumbar mobility in all planes, especially extension and extension plus lumbar rotation, and neurological examination and Valsalva manoeuvre negative. The lumbar fact sign defined by Acevedo, which is performed in the following 6 phases, is also useful for diagnosis:
- Phase I. Patient lying down in a supine position, with the lower limbs in a resting position.
- Phase II. Forced flexion of the hip joint is performed, with the leg extended, using the lowest part of the leg as support.
- Phase III. The patient is asked to exert a downwards force and, with the hand resting on the lower part of the leg, the examiner exerts an opposing force.
- Phase IV. The examiner suddenly interrupts the counterforce, resulting in a sudden fall of the limb.
- Phase V. Before the leg falls onto the surface of the examination table, the examiner prevents this contact by supporting it again.
- Phase VI. The sign is considered to be positive if localised pain appears in the lumbar paravertebral region close to the fact joints inflamed when performing the manoeuvre.
The exclusion criteria for our study were refusal of the patient to participate, a history of malignancy, acute spinal fractures, uncontrolled medical disease, and clotting disorders.
All patients were asked to complete a questionnaire prior to the intervention, at two and six months, and at one and two years. The questionnaire involved the degree of involvement, as measured using the Oswestry Disability Index (ODI), which evaluates the following 10 variables: pain intensity, standing, personal care, sleep habits, carrying objects, sexual activity, walking, social life, sitting and ability to travel; the visual analogue scale (VAS) for pain, both lumbar and radiating to the lower limb, and evolution of the analgesia used.
The following demographic and descriptive data were also collected for each patient: age, sex, body mass index (BMI), date of intervention, surgical history, time to progression of low back pain, mental health history, physical examination, lumbar MR findings, employment status, subsequent visits to accident and emergency (A&E) during follow-up and subsequent need for a new surgical intervention. Satisfaction with the treatment received was also evaluated by asking whether patients would undergo the intervention again knowing the results obtained a posteriori.
Description of the lumbar radiofrequency technique
The first step when carrying out this technique involves precise placement of the patient and checking that the bone structures concerned can be correctly visualised.
The patient must be lying down on a radiotransparent table, in a comfortable position that can be maintained throughout the procedure without moving. The surgeon normally stands on the left side of the patient if right-handed, or on the other side if left-handed.
With the arm of the image intensifier in the posteroanterior (PA) axis, a clear image of the lumbar vertebra should be obtained. If required, the position thereof must be adjusted to possible deviations of the spine until the lower edge of the vertebra is a single line, avoiding the possible appearance of double end plates as far as possible. If there is no marked vertebral deformity, a centred image of the spinous processes for the segments to be operated on must be obtained.
According to the recommendations of the Spanish Pain Society, which adheres to the guidelines of the International Spine Intervention Society, the medial branch of the posterior primary division of the segments concerned is located.
The image intensifier is first moved in an oblique direction from the initial PA axis, approaching the facet joint and spinous process from the contralateral side, to obtain a good view of the so-called “Scotty dog”. A needle with calibre 25 Gauge (G) is normally used to infiltrate only the surface tissues, taking care not to reach the bone due to the danger of anaesthetising the medial branch itself, thus preventing the subsequent localisation thereof by stimulation.
A radiofrequency needle with a calibre of 20 G and 100 millimeters (mm) in length, with an active tip measuring 10 mm, is then inserted along the angle of the X-ray beam to touch the “dog’s eye” in tunnel view. Once located in the correct position, this is checked using a hyperbolique projection and the depth regulated using a complete lateral projection (not exceeding the articular pillar).
The nerve passes through the junction between the transverse process and the upper articular pillar. The needle is guided to the appropriate point in “tunnel view” using an oblique view.
In summary, the radiological movements that must be carried out are those described in the article by Pérez-Cajaraville et al. (5):
- PA X-ray (XR): location of region to be treated.
- Axial XR: remove double contour. The double contour of the lower part of the vertebral body is removed using a movement of the fluoroscopy arc in a craniocaudal direction.
- Oblique XR: location of target point. View between 10° and 30°.
- Lateral XR: check final location of needle.
- PA XR: to locate L5–S1. The posterior branch of L5 is approached using the same references, although in this case, the upper internal region of the transverse process is substituted by the same position of the sacral ala.
The needles are inserted and their correct placement checked by sensory stimulation (50 hertz at around 0.5 volts) and motor stimulation of the multifidus with no contraction in the legs at 2 hertz (Hz). Anaesthesia (0.5–1.0 mL per level) is then administered and, after waiting for 2 minutes, the lesional radiofrequency is applied at 80 °C for 60 seconds.
Statistical analysis
Variables were described using conventional statistical techniques. Categorical variables were summarised using frequency tables (absolute and relative) and quantitative variables using the mean and standard deviation, although the median and quartiles are also presented.
Analysis was carried out by Bayesian inference using a repeated measures model with random effects for each of the three result variables evaluated (pure lumbar VAS, radiated VAS and ODI). The posterior means of the parameters and 95% credibility intervals (95% credI) are given in all cases. These are the Bayesian equivalent to the confidence interval in classical statistics but have the advantage of being able to be interpreted directly in probabilistic terms. In the case of differences, the posterior probabilities that the difference is greater than 0 are also given.
With regard to the multivariate analysis, this was fitted to a random effects model with covariables to estimate the effect there of on the changes in the variables over time.
Analyses were carried out using the R 3.5.2 statistical software package and MCMC (Markov Chain Monte Carlo) simulations of the posterior distribution were carried out using JAGS 4.3.0.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional investigation committee of Cabueñes University Hospital. Informed consent was taken from all patients for their data to be collected and to receive the analysed treatment.
Results
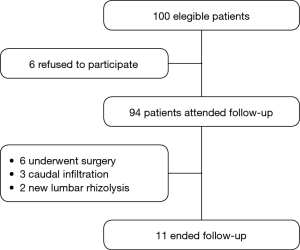
Six of the 100 patients enrolled in the study were excluded from follow-up due to a refusal of the patient to collaborate or a failure to attend. Six of the remaining 94 patients underwent surgery (5 arthrodesis and 1 vertebroplasty), three underwent caudal infiltration by the Pain Unit (PU) and two underwent a new lumbar rhizolysis, all of which resulted in an end to follow-up (Figure 1).
The mean age of our sample was 57.8 years (27.0–85.5), with a BMI of 27.09 (16.14–46.22), and 63.8% of subjects were female. The mean duration of the symptoms prior to the intervention was 8.7 years, with 28.7% of subjects having a history of spinal surgery, including discectomy, arthrodesis, interspinous device, etc.
With regard to their employment status, 23% of patients were in work, almost 20% were on sick leave and 36% were retired or incapacitated.
As for symptomatology, 93% of patients presented low back pain as their main symptom, 48% pain in overextension, 39% pain upon palpation of the spinous processes, 38% radiating pain and 20% neurogenic claudication, with two or more of these symptoms being found simultaneously in 81% of patients.
As far as analgesia is concerned, 3.2% of patients were not taking any pain medication, 31.9% were taking non-opioid analgesics, 56.4% minor opioids and 8.5% major opioids.
Similarly, 85.11% of patients exhibited facet joint degeneration in the lumbar resonance and 47.87% presented a history of mental health problems.
The mean VAS for pure low back pain pre-intervention was 7.9 and 5.4 for pain radiating to the lower limb, with a pre-intervention disability measured using the ODI of 43.19%.
The lumbar radiofrequency technique was carried out by the same surgeon in all patients, and the intervention was bilateral in 92.6% of cases.
A significant reduction in analgesics consumption was observed after rhizolysis, with the percentage of patients who did not require any such drug increasing by 25% and the consumption of minor opioids decreasing by 26%. There were no changes in the major opioids and non-opioid drug sub-groups.
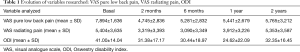
A statistically significant reduction in pure low back pain of 3.143 (3.753–2.536) points in the VAS at 2 months, 2.609 (3.217–1.999) points at 6 months, 2.434 (3.099–1.765) points at 1 year and 1.579 (2.713–0.426) points at 2 years was achieved versus baseline. In absolute terms, this represents a VAS score of 4.7 at 2 months, 5.3 at 6 months, 5.4 at 1 year and 5.8 at 2 years.
As for radiating low back pain, a significant reduction of 2.081 (2.753–1.405) points in the VAS at 2 months, 2.227 (2.937–1.535) points at 6 months and 1.503 (2.263–0.751) points at 1 year was observed versus baseline, with this corresponding to absolute values of 3.3 at 2 months, 3.1 at 6 months and 3.9 at 1 year. There was no variation with respect to the prior VAS at 2 years.
A statistically significant reduction in ODI of 11.7 points (14.5–8.8) at 2 months, 12.6 (15.5–9.7) points at 6 months, 18.4 (21.2–15.6) points at 1 year and 10.2 (15.5–4.9) points at 2 years was observed with respect to baseline, corresponding to absolute values of 31.38% at 2 months, 30.44% at 6 months, 24.62% at 1 year and 32.35% at 2 years (Table 1).
Full table
The multivariate analysis showed that these reductions are statistically significant, with none of the nine variables studied (age, sex, BMI, prior surgical intervention, time with low back pain in years, number of vertebral levels affected, prior analgesia ladder, history of mental health problems or existence of arthropathy) being confounding factors.
Female patients exhibited a mean increase of 4.616 (0.083–9.110) points with respect to the prior baseline ODI for males. An increase of 7.984 points (2.700–13.274) was also observed for a history of lumbar surgery, 0.307 points (0.044–0.569) for each year that the symptoms had presented and 6.030 points (2.850–9.174) for each step required on the analgesia ladder. This may mean that the presence of these factors (female or prior surgery) represents an increased risk of exhibiting a higher level of disability.
Only three complications were observed in this study. These represented 3.2% of the sample and consisted of two cases of lower limb weakness and one case of increased radiating pain, all of which were transient.
We also found that 84% of patients treated had no need to attend A&E for low back pain during the follow-up period for this study and that 69.1% (65 of 94 patients) were satisfied with the results of the intervention and would repeat the treatment knowing the results a posteriori.
Discussion
Demographic analysis
There are a large number of papers in the literature mainly dealing with the short-term clinical results (improvement in pain and function) and the selection of patients candidates for rhizolysis, some of which present contradictory findings (6-9).
There is also an important systematic review (2,8), which was initiated in 2003 and last updated in 2014 with the inclusion of more studies studying the effectiveness of radiofrequency in comparison with other treatments or placebo. This update only included randomised clinical trials involving patients with low back pain for more than three months and diagnostic block or positive diskography. After carrying out a search in various databases, a total of 36 studies were analysed, with 21 of these being included in the review and the remainder being excluded for various reasons (some were still ongoing at the time of said review). In total, the studies included had a sample size of 1,309 patients, with a mean age of 50.6 years.
The mean age of the patients included in our study is similar to those for the MINT study (52.2 years) (1) and those reported by Lakemeier et al. (56–58 years) (4), Nath et al. (53 and 56 years in the placebo and experimental groups, respectively) (10) and Cohen et al. (51, 58 and 61 years for each of the three sites participating in that study) (11).
The mean BMI in our study (27.09; 16.14–46.22) was also similar to that in the MINT study (26.43–27.62) (1). As far as sex is concerned, the percentage of females in our study was 63.8%, which is also similar to the value obtained in the latter study (61.8%) (1). However, these values contrast with those for the studies reported by Cohen et al. and Lakemeier et al., where the male population predominated (3,4). One possible explanation for this, and the fact that the mean age in Cohen’s study was 40 years, is that one of the sites at which data were collected was the Walter Reed Army Medical Center, the population of which is mainly active members of the armed forces (3).
The duration from the onset of the first symptoms to the intervention exhibits more variability, with a mean of 8.7 years in our study, 3–4 and 5–6 years in the two studies by Cohen et al. (3,4) and 11–12 reported by Nath et al. (10).
A history of prior spinal surgery was more prevalent in our study (29%) than in others, such as that by Cohen and Williams (4–9.8%) (3).
A comparison of the employment status for the patients in our study found higher values for subjects in work in the study by Cohen et al. (60–67%) (3) and in the MINT study, although the percentage of patients in paid work ranged between 48% and 61% in the latter (1). These demographic differences are directly related to the type of population in which lumbar radiofrequency was performed, as noted above.
Given the large number of radiofrequency denervations currently being carried out, and the associated cost (estimated at more than 50,000 million dollars in the USA) (11), very few studies have analysed which factors are associated with a better or worse response to treatment. In this regard, we should highlight the study by Cohen et al. (11), who analysed the data for several variables in 192 patients. After a statistical analysis of their data, these authors concluded that the factor most closely related to the outcome of denervation was the presence of exacerbation of low back pain upon extension and/or rotation of the spine. The presence of sensitivity to paraspinal palpation is one factor associated with a satisfactory response, even in obese patients, where this is more difficult to obtain during the examination as such patients tend to present a larger number of potentially pain-causing structures. Finally, it should be noted that a close relationship was found between prior spinal surgery and failure of rhizolysis, which is in agreement with our findings, which show that female sex, prior lumbar surgery, a longer duration of symptoms or greater consumption on the analgesic ladder represent a greater degree of disability prior to administration of the radiofrequency.
As for the location of the symptoms, the values obtained for spinal pain in our study are higher than those reported by Cohen et al. (45–58%) (11). The prevalence of facet joint arthropathy in the MR is also higher than that reported by Cohen et al. (66–68% for the various groups in that study) (11).
As mentioned above, correct selection of the patient is a key factor affecting the success of radiofrequency denervation. With regard to the paradigm of the need for an anaesthetic diagnostic block prior to performing rhizolysis, the study by Cohen et al. (3), who carried out a multicentre, randomised trial in 151 patients with low back pain due to degeneration of the facet joints, comparing three treatment options, namely radiofrequency denervation with no prior diagnostic block, guided only by the compatible physical examination, radiofrequency after a positive diagnostic block, and radiofrequency after two diagnostic blocks, is of particular interest. These authors defined a reduction in symptoms of 50% of more after three months as a positive outcome. They concluded that the most cost-effective option was not to perform a prior diagnostic block as a higher percentage of patients (33%) from the group in which no such block was performed obtained a positive response, compared with 16% and 22% from the groups receiving one and two blocks, respectively. The results of that study are considered to be a very important contribution to the current controversy regarding the selection of patients and the need for prior diagnostic blocks (12).
Cohen et al.’s study led us to the cost-effectiveness analysis performed by Bogduk and Holmes (13). According to that study, a high percentage of patients with chronic low back pain who underwent a diagnostic block of the facet joints presented a false positive to this treatment (estimated false-positive rate of 25–38%) (11). Indeed, these authors concluded that single diagnostic blocks may lead to an incorrect diagnosis, and therefore treatment, in a large percentage of cases.
The absence of a consensus (12) concerning the specific technique to be used to perform facet joint blocks, the medication to be administered and the dose to be used, or whether the nerves responsible also need to be blocked in addition to the facet joints, should also be taken into consideration. This may lead to confusion as regards patient selection and, therefore, their subsequent treatment. As an example, the study by Novak and Nemeth (12), which found marked variations in the selection patients with facet joint blocks, which were positive in 10–92% of cases, a range that does not agree with the prevalence of facet joint arthropathy of around 10–15% (13), should be noted.
In light of these conclusions, and given the lack of availability of operating theatres for carrying out these procedures, a diagnostic block was not performed in any case.
We conclude this section with a demographic analysis of analgesia consumption. In our study population, 3.2% of subjects were not taking any medication, almost a third was using anti-inflammatories and more than 60% had been prescribed opioids. This higher consumption of opioids than in other studies, such as those by Cohen et al. (3,11), is in agreement with information published by the Spanish Agency for Medicines and Medical Devices (AEMPS), which shows that the consumption of these drugs in Spain increased by 83.59% between 2008 and 2015 (14).
Analysis of results
The studies by Gallagher et al. (15) [1994], Leclaire et al. (16) [2001] and Tekin et al. (17) [2007] analysed the level of pain using a visual analogue scale and compared the results obtained for patients who underwent radiofrequency to those receiving placebo, finding a greater effectiveness of radiofrequency in the short term (less than one month), with significant differences and with a moderate level of evidence. However, other studies that performed the same analysis in the medium and long term, (between 1 and 6 months and longer than 6 months, respectively) found no greater effectiveness of the radiofrequency treatment [Leclaire et al. (16), van Kleef et al. (18), van Wijk et al. (19), Tekin et al. (17) and Nath et al. (10)].
With regard to discogenic low back pain, three studies have compared radiofrequency denervation treatment and placebo in terms of improved functional status and pain levels in the short [Kapural et al. (20)], medium [Barendse et al. (21) and Kapural et al. (20)] and long term [Kvarstein et al. (22) and Kapural et al. (20)]. Significant differences were only found in the long term, with a moderate degree of evidence for a greater effectiveness of radiofrequency treatment with respect to placebo. No differences were found in the short- or medium-term, although this only had a low degree of evidence.
Finally, with regard to pain arising in the sacroiliac joints, two low-quality studies [Cohen et al. (23) and Patel et al. (24)] also compared radiofrequency with placebo, finding no short-term differences in terms of pain and function. Patel et al. (24) also analysed the differences in the medium term, finding a greater benefit for radiofrequency although with only a low degree of evidence.
The values obtained in our analysis of low back pain prior to rhizolysis, as measured using the VAS, are slightly higher than those reported for the MINT study (7.06–7.43) (1), and those reported by Lakemeier et al. (6.6–7) (4) and Nath et al. (4.38–5.98) (10). With regard to pain radiating to the lower limbs, we again obtained values higher than those reported by Nath et al., who reported values of 2.68 for the placebo group and 4.33 for the intervention group (10). Similarly, when evaluating the degree of disability pre-intervention using the ODI, the mean values in our study are higher than those reported for the MINT study [34-39] (1) and by Cohen et al. (30, 34 and 36 in the three study groups) (3). However, they are similar to the values reported by Lakemeier et al. (41 and 39 for the two groups analysed) (4).
In terms of the evolution of low back pain measured using the VAS, the reduction found in our study is similar to that reported in the MINT study (4.50–4.92 at 6 months in the intervention group) (1) or by Lakemeier et al. (VAS of 4.7 in the group receiving radiofrequency treatment at 6 months), although the reduction in this latter study was not statistically significant (4). The reduction obtained in our analysis (2.6 points) is also similar to, although slightly better than, the value reported by Nath et al., who found a reduction of 2.1 points in the experimental group at 6 months (10).
These same authors obtained a reduction of 1.6 points on the VAS for radiating pain in the experimental group (10), with our improvement again being somewhat better (2.2 points).
With regard to the evolution of post-rhizolysis disability during follow-up using the ODI, the values obtained at 6 months in our study (mean of 30.44 points) are slightly higher than those reported for the MINT study (mean of 25.38, 25.99 and 30.24 for the three intervention groups receiving radiofrequency treatment) (1). Similarly, Lakemeier et al. reported a mean ODI score of 28 at 6 months, which is again lower than our value. However, these differences disappear at one year of follow-up, where the mean for our study (24.62 points) is similar to, and even lower than, the values obtained for the groups in the MINT study who underwent rhizolysis (24.59, 27.29 and 31.20) (1). The absence of subsequent controls at 12 and 24 months in the study of Lakemeier et al., and at 24 months in the MINT study, means that we are unable to compare the trend in the ODI at these time points. It should be noted that the mean reduction at 6 months in our study is greater than that reported by Lakemeier, which was 2 points for the group receiving rhizolysis, although that difference was not statistically significant (4), whereas the reduction in our analysis is statistically significant, with a mean value of 12.6 points.
Our analysis of the variation in analgesia consumption after the intervention showed that our findings are similar to those reported by Cohen et al., although slightly better than in this latter study (3).
The use of corticosteroids to treat facet joint osteoarthritis remains controversial as the studies reported in the literature present contrasting results. Thus, although Lilius et al. (25) found no differences with respect to placebo, Carette et al. (26) reported a significant improvement in the group receiving corticosteroids at 6 months. However, literature reviews, such as those published by Manchikanti et al. (27) or Boswell et al. (28) assigned a mild to moderate degree of evidence to these findings.
The study reported by Lakemeier et al. (4) is of particular interest as it was the first to compare the effectiveness of radiofrequency and intra-articular corticosteroid injections. This randomized, controlled, double-blind trial was carried out in Germany and included 89 patients, who were followed-up for a period of 6 months. Analysis of the results showed no significant differences between the two procedures for any of the measurements performed, although the pain level decreased more in the group receiving radiofrequency.
Similarly, the studies of Civelek et al. (29), Duger et al. (30) and Lakemeier et al. (4) show that radiofrequency is more effective at improving pain, as measured using the visual analogue scale, that corticosteroid injections in the short-, medium- and long-term, although the degree of evidence of very low to low.
In our study, in the absence of contraindications such as allergies or uncontrolled diabetes, a dose of corticosteroid (1 mL betamethasone) was administered locally at each of the points where lesional radiofrequency was applied.
The number of complications observed during our study was similar to that reported by Cohen et al. (3). In that study, two patients experienced a worsening in low back pain, as measured using the VAS, and another patient developed radiating pain in the lower limbs that was not present previously. These findings are similar to the complications observed in our study, which also consisted of the presence of new pain in the lower limbs, or weakness in them.
Various studies have compared the effectiveness of the different techniques and approaches used for radiofrequency denervation (31-33). Thus, Kroll et al. (31) compared the effectiveness of applying continuous or pulsed radiofrequency in terms of improvements in pain, finding no differences in this regard, although with a very low degree of evidence.
With regard to the studies included in this review (2) and their relevance, it should be noted that reductions in the pain VAS and NRS of 30%, and improvements in the ODI of 8–12%, were considered to be clinically relevant. Only 7 of the 21 studies analysed reported relevant changes from a clinical viewpoint. In this regard, many of these studies involved small sample sizes, thus preventing conclusions applicable to clinical practice from being reached, or where concerned with the safety or possible complications of radiofrequency treatment.
As far as limitations of our study are concerned, we would like to point out the fact that 11 patients from the initial population were lost, which may represent a selection bias. These patients presented a baseline ODI 3.0 points higher than the mean and exhibited a lesser response in the ODI at two months, with a reduction of 5.1 points. Furthermore, the absence of a control group is another limitation of our article.
This finding may represent a new line of research aimed at attempting to predict whether a score of more than 45% on the ODI scale may be a predictive factor for poor outcome.
Conclusions
Lumbar rhizolysis produces a statistically significant reduction in pain and functional disability in patients with chronic low back pain, with this reduction being maintained for the first two years post-treatment, thus significantly reducing analgesia consumption.
Female patients with a prior history of surgery, whose symptoms prior to treatment had lasted for longer and with greater consumption on the analgesics ladder presented the worst disability scores prior to the administration of radiofrequency treatment.
The fact that 11 patients from the initial population were lost may represent a selection bias. These patients presented a baseline ODI 3.0 points higher than the mean and exhibited a lesser response in the ODI at two months, with a reduction of 5.1 points.
This finding may represent a new line of research aimed at attempting to predict whether a score of more than 45% on the ODI scale may be a predictive factor for poor outcome.
Acknowledgments
We wish to thank the Principado de Asturias’ Health Research Institute (ISPA) (Spain) for assisting in the statistical analysis, and Tradelia for their assistance in translating the article and language editing. We want to thank the orthopaedics department chairperson Manuela Riera Campillo for providing general support. Another contributors who we wish to thank for their technical support: Ángel Ramón Piñera Parrilla, Diego Velasco Villa, Lucía Lanuza Lagunilla, Pablo José Suárez-Anta Rodríguez.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jss-20-599
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jss-20-599
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss-20-599). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional investigation committee of Cabueñes University Hospital. Informed consent was taken from all patients for their data to be collected and to receive the analysed treatment.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Juch JNS, Maas ET, Ostelo RWJG, et al. Effect of Radiofrequency Denervation on Pain Intensity Among Patients With Chronic Low Back Pain: The Mint Randomized Clinical Trials. JAMA 2017;318:68-81. [Crossref] [PubMed]
- Maas ET, Ostelo RW, Niemisto L, et al. Radiofrequency denervation for chronic low back pain. Cochrane Database Syst Rev 2015.CD008572. [Crossref] [PubMed]
- Cohen SP, Williams KA, Kurihara C, et al. Multicenter, randomized, comparative cost-effectiveness study comparing 0, 1, and 2 diagnostic medial branch (facet joint nerve) block treatment paradigms before lumbar facet radiofrequency denervation. Anesthesiology 2010;113:395-405. [Crossref] [PubMed]
- Lakemeier S, Lind M, Schultz W, et al. A comparison of intraarticular lumbar facet joint steroid injections and lumbar facet joint radiofrequency denervation in the treatment of low back pain: a randomized, controlled, double-blind trial. Anesth Analg 2013;117:228-35. [Crossref] [PubMed]
- Pérez-Cajaraville J, Sancho-de Ávila A, Cabrera I, et al. Radiofrecuencia de facetas lumbares y cervicales. Rev SocEspDolor 2011;18:249-58.
- Van Zundert J, Hartrick C, Lataster A, et al. Evidence-Based Interventional Pain Practice: According to Clinical Diagnoses. Oxford, UK: Wiley-Blackwell, 2011.
- Koes BW, van Tulder M, Lin CW, et al. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J 2010;19:2075-94. [Crossref] [PubMed]
- Niemistö L, Kalso E, Malmivaara A, et al. Radiofrequency denervation for neck and back pain: a systematic review within the framework of the cochrane collaboration back review group. Spine (Phila Pa 1976) 2003;28:1877-88. [Crossref] [PubMed]
- Henschke N, Kuijpers T, Rubinstein SM, et al. Injection therapy and denervation procedures for chronic low-back pain: a systematic review. Eur Spine J 2010;19:1425-49. [Crossref] [PubMed]
- Nath S, Nath CA, Pettersson K. Percutaneous lumbar zygapophysial (facet) joint neurotomy using radiofrequency current, in the management of chronic low back pain. A randomized double-blind trial. Spine 2008;33:1291-7. [Crossref] [PubMed]
- Cohen SP, Hurley RW, Christo PJ, et al. Clinical predictors of success and failure for lumbar facet radiofrequency denervation. Clin J Pain 2007;23:45-52. [Crossref] [PubMed]
- Novak S, Nemeth WC. RE. cost-effectiveness of diagnostic medial branch blocks before radiofrequency denervation. Spine J 2008;8:412-3. [Crossref] [PubMed]
- Bogduk N, Holmes S. Controlled zygapophysial joint blocks: the travesty of cost-effectiveness. Pain Med 2000;1:24-34. [Crossref] [PubMed]
- Agencia Española de Medicamentos y Productos Sanitarios [internet]. Madrid: Agencia Española del Medicamento y Productos Sanitarios; 2018 [acceso 9 de Marzo de 2018]. Utilización de medicamentos opioides en España durante el periodo 2008-2015; 3 páginas. Available online: https://www.aemps.gob.es/medicamentosUsoHumano/observatorio/docs/opioides-2008-2015.pdf
- Gallagher J, Petriccione di Vadi PL, Wedley JR. Radiofrequency facet joint denervation in the treatment of low back pain: a prospective controlled double-blind study to assess its efficacy. Pain Clinic 1994;7:193-8.
- Leclaire R, Fortin L, Lambert R, et al. Radiofrequency facet joint denervation in the treatment of low back pain: a placebo-controlled clinical trial to assess efficacy. Spine (Phila Pa 1976) 2001;26:1411-6; discussion 1417. [Crossref] [PubMed]
- Tekin I, Mirzai H, Ok G, et al. A comparison of conventional and pulsed radiofrequency denervation in the treatment of chronic facet joint pain. Clin J Pain 2007;23:524-9. [Crossref] [PubMed]
- van Kleef M, Barendse GA, Kessels A, et al. Randomized trial of radiofrequency lumbar facet denervation for chronic low back pain. Spine (Phila Pa 1976) 1999;24:1937-42. [Crossref] [PubMed]
- van Wijk RM, Geurts JW, Wynne HJ, et al. Radiofrequency denervation of lumbar facet joints in the treatment of chronic low back pain: a randomized, double-blind, sham lesion-controlled trial. Clin J Pain 2005;21:335-44. [Crossref] [PubMed]
- Kapural L, Vrooman B, Sarwar S, et al. A randomized, placebo-controlled trial of transdiscal radiofrequency, biacuplasty for treatment of discogenic lower back pain. Pain Med 2013;14:362-73. [Crossref] [PubMed]
- Barendse GA, van Den Berg SG, Kessels AH, et al. Randomized controlled trial of percutaneous intradiscal radiofrequency thermocoagulation for chronic discogenic back pain: lack of effect from a 90-second 70 C lesion. Spine (Phila Pa 1976) 2001;26:287-92. [Crossref] [PubMed]
- Kvarstein G, Måwe L, Indahl A, et al. A randomized double-blind controlled trial of intra-annular radiofrequency thermal disc therapy--a 12-month follow-up. Pain 2009;145:279-86. [Crossref] [PubMed]
- Cohen SP, Hurley RW, Buckenmaier CC 3rd, et al. Randomized placebo-controlled study evaluating lateral branch radiofrequency denervation for sacroiliac joint pain. Anesthesiology 2008;109:279-88. [Crossref] [PubMed]
- Patel N, Gross A, Brown L, et al. A randomized, placebo-controlled study to assess the efficacy of lateral branch neurotomy for chronic sacroiliac joint pain. Pain Med 2012;13:383-98. [Crossref] [PubMed]
- Lilius G, Laasonen EM, Myllynen P, et al. Lumbar facet joint syndrome. Significance of non-organic signs. A randomized placebo-controlled clinical study. Rev Chir Orthop Reparatrice Appar Mot 1989;75:493-500. [PubMed]
- Carette S, Marcoux S, Truchon R, et al. A controlled trial of corticosteroid injections into facet joints for chronic low back pain. N Engl J Med 1991;325:1002-7. [Crossref] [PubMed]
- Manchikanti L, Datta S, Derby R, et al. A critical review of the American Pain Society clinical practice guidelines for interventional techniques: part 1. Diagnostic interventions. Pain Physician 2010;13:E141-74. [PubMed]
- Boswell MV, Trescot AM, Datta S, et al. Interventional techniques: evidence-based practice guidelines in the management of chronic spinal pain. Pain Physician 2007;10:7-111. [PubMed]
- Civelek E, Cansever T, Kabatas S, et al. Comparison of effectiveness of facet joint injection and radiofrequency denervation in chronic low back pain. Turk Neurosurg 2012;22:200-6. [PubMed]
- Duger C, OzdemirKol I, Kaygusuz K et al. Effects of facet joint nerve block addition to radiofrequency in the treatment of low back pain. Journal of Society for Development of New Net Environment in B&H 2012;6:2052-6.
- Kroll HR, Kim D, Danic MJ, et al. A randomized, double-blind, prospective study comparing the efficacy of continuous versus pulsed radiofrequency in the treatment of lumbar facet syndrome. J Clin Anesth 2008;20:534-7. [Crossref] [PubMed]
- Moon JY, Lee PB, Kim YC, et al. An alternative distal approach for the lumbar medial branch radiofrequency denervation: a prospective randomized comparative study. Anesth Analg 2013;116:1133-40. [Crossref] [PubMed]
- Sanders M, Zuurmond WWA. Percutaneous intra-articular lumbar facet joint denervation in the treatment of low back pain: a comparison with percutaneous extra-articular lumbar facet denervation. Pain Clinic 1999;11:329-35.