
Factors influencing upper-most instrumented vertebrae selection in adult spinal deformity patients: qualitative case-based survey of deformity surgeons
Introduction
The upper-most instrumented vertebrae (UIV) for a spinal construct is an important decision for surgeons treating patients with adult spinal deformity (ASD). The health of adjacent segments to the UIV may determine long-term survival of a construct (1). Patients may become impaired from proximal junctional kyphosis (PJK), vertebral fracture, limitations of activities of daily living (ADLs) and worse clinic outcomes depending in part on the UIV chosen in multi-level fusions for ASD (2-5).
There are a variety of risks/benefits that are potentially determined by UIV selection. If the top of a construct ends in the upper thoracic (UT) spine it allows for more powerful correction of larger spinal deformities, may reduce the overall rate of proximal junctional failure and enhance the maintenance of radiographic correction of ASD, but it is also may negatively impact ADLs, including personal hygiene (5-10). In contrast, when the UIV is in the lower thoracic (LT) spine, there is less operating room time, less blood loss, lower cost, less chance of iliac screw loosening and clinical outcomes are still positive (4,11,12).
The goal of the present study is to better understand why surgeons choose a specific UIV for ASD patients. Typically, clinical experience drives surgeons to either go up to the UT spine versus the LT spine. This decision-making process might be unique to each patient and surgeon, however the authors hypothesized that there is likely a pattern to this decision making process. We sought to define this decision-making process through case presentations to a group of experienced surgeons and to apply this defined pattern of care prospectively to a group of ASD patients. We further hypothesized that patients who had been previously treated for ASD with a UIV selection consistent with the decision making algorithm defined in this study would have a lower rate of PJK compared to patients with a UIV that differed from the UIV selection algorithm.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jss-20-598).
Methods
Clinical case presentations
We began our study by first selecting eleven patients from a single-surgeon database of patients with ASD. Eleven patients were selected based on previous studies. We used an internal database in order to obtain all pertinent imaging studies (supine radiographs, MRIs, CT scans) and to obtain detailed clinical information on this select group of patients. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Hospital for Special Surgery (IRB #: 2014-357) and informed consent was taken from all the patients. The inclusion criteria for this database was presence of spinal deformity defined as a coronal Cobb angle of >20 degrees, sagittal vertical axis (SVA) of >5 cm, pelvic tilt (PT) of >25 degrees and/or thoracic kyphosis >60 deg. These 11 patients were presented to 14 experienced spinal deformity surgeons who were asked what level they would select as the UIV for correction of the spinal deformity. The surgeons were blinded from the hypothesis of the study and we did not share with results amongst surgeons until the drafting of our manuscript. The selection of these 11 patients was based upon a random selection of patients that had fusion to the pelvis and up to L1 or higher. Surgeons were presented the cases between 2017–2018.
The cases for each patient were summarized in a slideshow for the surgeons. Data from the patient’s clinical records, including history of present illness (HPI) and pain descriptors such as location, intensity, aggravating or relieving factors (Table 1). Any paresthesia or areas of weakness were included. A detailed history of previous treatments was included. Physical examination data, comprising general and specific spine examination (motor, sensory exam), were provided to the surgeons (Table 2).
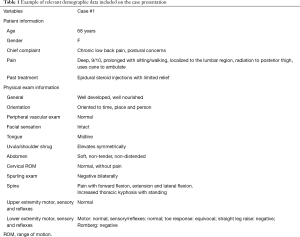
Full table

Full table
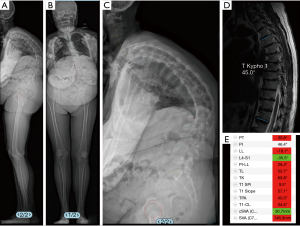
Relevant radiographs were included in our presentation for each patient. These included full-length free-standing antero-posterior and lateral spine radiographs (36” minimum) or full body EOS radiographs. These radiographs were analyzed using a validated and dedicated software (Surgimap, Nemaris Inc., USA) (13). Preoperative supine radiographs were also collected to determine the flexibility of the spine. When supine radiographs were not available, MRI or CT images were used as a substitute to measure lumbar lordosis or thoracic kyphosis (Figure 1). Radiographic parameters for spinal alignment investigation were extracted from the analysis and presented to the reviewers including PT and pelvic incidence (PI). Regional curvatures were analyzed using the Cobb method and were evaluated at the lumbar level between L1 and S1 (lumbar lordosis) and between T4 and T12 (thoracic kyphosis). Global alignment was assessed using the SVA. Radiographs were also evaluated for accompanying antero or lateral listhesis. When available, preoperative MRI and CT images were also collected. Axial images at each vertebral level were assessed for the presence of central spinal stenosis, foraminal spinal stenosis and disc-degeneration.
Survey to surgeons
The data for each patient was collected and collated into a slideshow. These slideshows included all information that should be necessary for an operative decision. Each case was followed by a questionnaire. All cases were assumed to have a fusion from at least L1 to the pelvis. This survey was sent to 14 surgeons to review cases and answer framed questions. The surgeons were asked to pick the best-suited UIV (any level: cervical, thoracic, or lumbar) for each case. The questionnaire contained 6 questions and encompassed the choice of the level of UIV and reasons for the avoidance of adjacent vertebral levels. The questionnaire asked (I) what would be your UIV level? (II) If the UIV was in the UT, why not the LT? (III) If the UIV was in the LT, why not the UT? (IV) Within the UIV region you selected what were the key determinants against a more proximal level? (V) Within the UIV region you selected what were the key determinants against a more distal level? Finally, the surgeons were asked to rank the most relevant reason for UIV selection amongst the following reasons: fear of proximal junctional kyphosis, junctional disease over the long term, patient function, trade-off in terms of surgical time/bleeding and reaching alignment goal, other. All surgeons in our study provided complete answers for each of the 11 cases in the survey. Every surgeon that was asked to participate in this study had at least 5 years of experience performing spinal deformity surgery. Each was fellowship trained in spine surgery. Furthermore, all surgeons included in this study are members of an international society of specialists devoting time to the advancement/study of principles for treating patients with spinal deformity.
Surgeon selection of UIV
The answers from the survey, including UIV selection and reasoning behind UIV choice, were collected and organized. We first categorized each UIV chosen into either the UT (T1-T6), LT (T7-T12), lumbar or cervical region. We defined a disagreement when there were more than 2 surgeons who differed from the group on UT or LT UIV location. The specific level at which the UIV was selected was collected for each surgeon/case. We grouped descriptive answers together based on common language used amongst surgeons. Surgeons were blinded to other surgeon’s responses.
Development and application of algorithm for UIV selection
Once all the answers from surgeons were collected and organized, an algorithm was created based on a qualitative assessment of reasons for the UIV of a construct. This algorithm was then applied to a prospective database of ASD patients that underwent an operation for their deformity. This database is a prospective collection of clinical/radiographic data from 11 centers across the United States. All patients were enrolled into an Institutional Review Board-approved protocol by each site. The inclusion criteria for this International database were: patients over 18 years old, presence of spinal deformity defined as a coronal Cobb angle of >20 degrees, SVA of >5 cm, PT of >25 degrees and/or thoracic kyphosis >60 deg. We only included patients with at least 2 years of follow up information, were fused to the pelvis, had pre- and post-operative radiographs to 2 years out from surgery and had no previous fusion above L1.
Statistical analyses
The selected UIV was compared to the predicted UIV. A chi-square analysis was used to compare the rate of PJK in patients fused to the LT spine when the algorithm predicted better PJK outcomes with UT spine as the UIV. A similar chi-square analysis was done to compare the rate of PJK in patients that went to the UT spine when the algorithm stated no change in PJK when going to the LT spine. The definition of PJK was proximal junction sagittal Cobb angle greater than 10 degrees and proximal junction sagittal Cobb angle at least 10 degrees greater than preoperative measurement (14). All statistical analysis was performed with SPSS (IBM SPSS, NY). If there was missing data for any patient they were excluded from the analysis.
Results
UIV selection summary
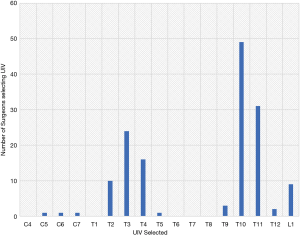
All 14 surgeons responded to all 11 cases and indicated their desired UIV (Figure 2). The UIV selected at each individual level is shown in Figure 2. Figure 2 reflects the number of surgeons that selected each UIV level. The top three UIV selected were T10, T11 and T3. The UT, LT, lumbar and cervical regions were selected in 36.2%, 55.9%, 5.9% and 2.0% of cases respectively for these 11 cases. In 8/11 cases (73%) there was agreement amongst the spine surgeons regarding the region of the UIV.
Justifications of UIV region selected
The LT region was selected as UIV for a variety of reasons. The most common reason was small TK (less than 55 degrees) or lack of sagittal deformity in the proximal thoracic spine. Less common reasons or reasons that were lower in priority for UIV selection for the surgeons were limitations to function with proximal fusions and potential comorbidity of extending a fusion to the UT or cervical spine.
The most common reason for selecting UT was increased kyphosis through the thoracic spine. This led to concerns of increased risk of proximal junctional failure. Less common or reasons lower in priority for UIV selection for the surgeons included a desire to achieve a more complete correction, presence of coronal deformity, and age of the patient/osteoporosis. In all cases, the most common reason for selection of the region for UIV was the amount of kyphosis in the thoracic spine. The local selection of UIV was based largely on the local kyphosis above a potential UIV selection.
Justifications for individual UIV selected
There were common reasons for selecting individual levels for the UIV. T1 and T12 were often not selected in order to avoid the cervicothoracic or thoracolumbar junctions, respectively. T6-T8 was avoided because the thoracic apex tended to be at T6-T8. L1 was avoided in one case because of degenerative changes at the L1/L2 level.
Reasons for UIV disagreement
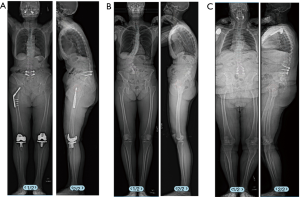
In three cases there was substantial disagreement among surgeons regarding the UIV region. These discrepancies were between UT and LT regions in all three cases. In one case of disagreement there did not appear to be significant thoracic deformity, but several surgeons were concerned about stopping in the LT due to perceived worse bone health based on radiographs. Also, a subset of surgeons was concerned regarding the patient’s overall medical health to survive a larger surgery to the UT spine. Similarly, the second case of disagreement was based on the patient’s relatively younger age and better bone health based on bone quality on radiographs which convinced several surgeons that PJK might be avoided by simply fusing to the LT region. Other surgeons were concerned about stopping in the LT because of the high TK for the case. In the last case of disagreement, the surgeons differed on the global sagittal alignment of the patient and the risk of PJK perhaps being higher due to BMI of a patient. The radiographs for the three cases where there was substantial disagreement are shown in Figure 3.
Creating an algorithm for UIV selection
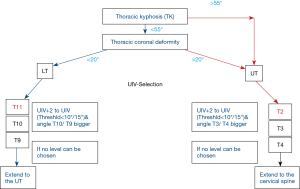
After synthesizing the responses provided by the 14 surgeons for UIV selection in 11 cases, the group arrived at an algorithm for selection of UIV. From survey responses we felt the most important factor to delineate UIV was whether there was significant thoracic coronal curve. If so, one was obligated to fuse to the UT. The 2nd most important consideration from several surgeons was whether there was a significant amount of thoracic kyphosis. If there was a large thoracic kyphosis most surgeons would fuse up to the UT. Deciding which precise level within the UT or LT was based on the Cobb angle between the UIV and the UIV+2. The algorithm is shown in Figure 4. All surgeons included in this study agreed with our algorithm.
Applying the algorithm to a retrospective database of ASD patients
Out of a database of 1,654 patients, there were 236 patients that met our inclusion criteria. Mean age was 64.1±9.5 years old. When the algorithm predicted going up to the UT spine and the surgeon selected a UIV in the LT spine there was a statistically significantly higher rate of PJK at 2-year follow up (76.9% vs. 38.9%, P=0.025). Conversely, when the algorithm predicted better outcomes with going to the LT spine and the surgeon went up to the UT spine, there was no difference in rate of PJK (P>0.05).
Discussion
Our study was able to outline the decision-making process of 14 surgeons for UIV selection in long spinal constructs for ASD patients. We found the most important factor in determining UIV for patients was the magnitude of thoracic kyphosis at the UIV+2 to UIV. Furthermore, there were certain favored vertebrae for UIV selection, including T3 for the UT spine T10 for the LT spine.
Our cohort agreed that any severe coronal curve greater than 20 degrees would make it difficult to correct with a UIV in the LT. Similarly, any patient with an extreme hyperkyphosis (>50 degrees) was favored to have a UIV in the UT. This is because the curve might not be completely corrected with a UIV in the LT or stopping in the LT may lead to ending a construct at a kyphotic level. When deciding between individual levels in the UT/LT, local kyphosis at the UIV+2 to UIV dictated the precise level to end the construct.
In one of the cases where there was disagreement amongst surgeons, there was concern amongst several surgeons regarding the safety of achieving appropriate correction in a medically complex patient. Several reports detail the substantial rate of medical complications for patients undergoing extensive ASD surgery (15,16). Furthermore, Schwab et al. demonstrated that increased invasiveness of a surgery is associated with higher complication rates (17). Surgeons using the algorithm reported in this study should take care to ensure that a patient can tolerate a larger surgery when deciding between the UT versus the LT spine for the UIV.
One insight that came from our discussions regarding ASD cases was the clinical importance of objective measurements of bone health when deciding the UIV. The fact that we did not specifically include these data within our case descriptions is a substantial limitation. Osteoporosis can make appropriate surgical treatment of ASD difficult given the propensity of instrumentation failure (18) and higher risk for PJK (19). Strategies to augment bone health prior to surgical treatment for this cohort of patients may help in maintaining post-operative correction,
Surgeons in our analysis frequently cited potential “loss of function” postoperatively as a reason to avoid fusing to the UT. Sciubba et al. showed that there could be significant impairment associated with personal hygiene while toileting amongst ASD patients when a fusion was brought up to the UT spine (5,20). This decrease in function should provide surgeons pause when contemplating extension of spinal fusion to the UT spine.
The results of this study show that local and regional thoracic kyphosis are important factors that should be considered when selecting a UIV for a construct. Previous studies have shown that the rate of PJK isn’t different when comparing groups of patients with fusions that have UIV in the UT versus the LT (21), but there is a higher rate of pseudarthrosis when fusing to the UT (22). Our analysis studied the differences in proximal kyphosis that might better show why some constructs with a UIV in the LT spine develop PJK.
It is important to recognize the learning curve required to perform extensive ASD surgery and that the surgeons involved in this study have had numerous years of experience performing surgery for ASD. Therefore, they might have chosen to proceed to the UT or cervical spine based on their efficiency in the operating room with instrumentation and correction of large spinal deformities. Surgeons should be aware of their capabilities as well as the risks associated with larger procedures for ASD (17,23-25).
Our results are consistent with previous literature regarding UIV selection in the LT spine. T10 was the most common LT UIV selected amongst our surgeons. This was consistent with previous studies and is likely due to the fact the T10 is typically the lowest immobile vertebrae in the thoracic spine (3,26). There is likely little benefit to proceeding higher in the LT spine as long as the ASD curve does not extend more proximally.
There are several important limitations to the present study. We did not examine clinical complication rates amongst patients. This might have further demonstrated the potential problems with aggressive fusions up to UT even if PJK might be avoided. We did not include flexion/extension radiographs within the survey provided to surgeons. This might have shown better flexibility in the lumbar/thoracic spine which could have influenced the UIV selection amongst surgeons. Our analysis was based on responses from a small group of surgeons. We cannot state that these opinions reflect the larger community of spine surgeons as a whole. Our panel, however, does constitute a group of surgeons from around the world with a broad range of surgical experiences. There may be inherent biases within our group of deformity surgeons which we cannot control for within our study design. The authors also acknowledge the limitation of using PJK as a measure of possible poor selection of UIV. PJK may not be symptomatic and therefore our results may not accurately reflect clinical failure of a UIV level selected but rather only a radiographic finding for a patient (27). Still, PJK is associated with proximal junctional failure and this is why it was selected for analysis. Finally, this is a retrospective review of a database of patients with cases from surgeons that decided the algorithm of UIV selection. Therefore, there is a degree of confirmation bias that is inherent in our study design.
In conclusion, we have provided a simplified algorithm for picking UIV amongst patients requiring surgery for ASD. When applied to a retrospective database of patients treated with surgery for ASD, those that did not fuse to the UT but rather stopped at the LT spine had higher rates of PJK than those that followed our algorithm and fused to the UT. We recommend close examination of local and regional kyphosis when deciding UIV to help avoid possible development of PJK.
Acknowledgments
Funding: The International Spine Study Group (ISSG) is funded through research grants from DePuy Synthes (current), Nuvasive (current), K2M (current), Innovasis (past), Biomet (past), and individual donations.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jss-20-598
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jss-20-598
Peer Review File: Available at http://dx.doi.org/10.21037/jss-20-598.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss-20-598). Dr. SB reports personal fees from K2M, from Medtronic, personal fees from Nuvasive, from Orthofix, personal fees from Stryker, outside the submitted work; Dr. DB reports grants from Bioventus, grants from Depuy, grants from Pfizer, grants from Progenerative Medical, outside the submitted work; Dr. PP reports other from Allosource, personal fees from Globus Medical, personal fees from Medicrea, personal fees from Royal Biologics, personal fees from SpineWave, personal fees from Terumo, personal fees from Zimmer, outside the submitted work; Dr. MG reports grants from Depuy, personal fees from Globus, grants from Innomed, personal fees from Johnson and Johnson, personal fees from Medtronic, other from Proctor and Gamble, personal fees from Wolters Kluwer Health, outside the submitted work; Dr. TP reports other from Altus, personal fees from Globus Medical, personal fees from Medicrea, personal fees from Nuvasive, other from Spine Align, personal fees from Stryker, other from Torus Medical, outside the submitted work; Dr. HJK reports personal fees from Alphatec, other from K2M, other from Zimmer, outside the submitted work; Dr. JSS reports other from Alphatec, personal fees from Carlsmed, personal fees from Cerapedics, grants from Depuy, other from Nuvasive, personal fees from Styker, other from Zimmer, outside the submitted work; Dr. RE reports personal fees from Aesculap, other from Alphatec, personal fees from Baxter, personal fees from Biederman-Motech, personal fees from Carevature, other from Globus, other from Invuity, personal fees from Medtronic, other from Nocimed, personal fees and other from Nuvasive, personal fees from Radius, other from Seaspine, personal fees and other from SI Bone, other from Spine Innovations, outside the submitted work; Dr. KK reports personal fees and other from Depuy, personal fees and other from Orthofix, other from Strykler, outside the submitted work; Dr. GM reports personal fees from Carlsmed, other from K2M, other from Nuvasive, personal fees from Seaspine, personal fees from Stryker, personal fees from Viseon, outside the submitted work; Dr. CS reports grants from Depuy, grants from Globus, grants and other from Medtronic, other from Nuvasive, other from SI Bone, outside the submitted work; Dr. JG reports grants and other from Accuity, other from Cingulate, personal fees from Depuy, grants from Integra, personal fees from Intellirod, personal fees from K2M, personal fees from Mazor, personal fees from Medtronic, grants from Norton Healthcare, other from Nuvasive, personal fees from Pfizer, personal fees from Stryker, outside the submitted work; Dr. VL reports personal fees from Depuy, personal fees from Globus, other from Nuvasive, personal fees from Permanante Medical Group, outside the submitted work; Dr. FS reports grants from Depuy, personal fees from Globus, from K2M, personal fees from Medicrea, grants, personal fees and other from Medtronic, grants from Nuvasive, grants from Styker, grants, personal fees and other from Zimmer, outside the submitted work. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work and ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Hospital for Special Surgery (IRB #: 2014-357) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Shufflebarger H, Suk SI, Mardjetko S. Debate: determining the upper instrumented vertebra in the management of adult degenerative scoliosis: stopping at T10 versus L1. Spine (Phila Pa 1976) 2006;31:S185-94. [Crossref] [PubMed]
- Kim HJ, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis results in inferior SRS pain subscores in adult deformity patients. Spine (Phila Pa 1976) 2013;38:896-901. [Crossref] [PubMed]
- Cho KJ, Suk SI, Park SR, et al. Selection of proximal fusion level for adult degenerative lumbar scoliosis. Eur Spine J 2013;22:394-401. [Crossref] [PubMed]
- Kim HJ, Boachie-Adjei O, Shaffrey CI, et al. Upper thoracic versus lower thoracic upper instrumented vertebrae endpoints have similar outcomes and complications in adult scoliosis. Spine (Phila Pa 1976) 2014;39:E795-9. [Crossref] [PubMed]
- Sciubba DM, Scheer JK, Smith JS, et al. Which daily functions are most affected by stiffness following total lumbar fusion: comparison of upper thoracic and thoracolumbar proximal endpoints. Spine (Phila Pa 1976) 2015;40:1338-44. [Crossref] [PubMed]
- Zou L, Liu J, Lu H. Characteristics and risk factors for proximal junctional kyphosis in adult spinal deformity after correction surgery: a systematic review and meta-analysis. Neurosurg Rev 2019;42:671-82. [Crossref] [PubMed]
- Yagi M, Fujita N, Okada E, et al. Fine-tuning the Predictive Model for Proximal Junctional Failure in Surgically Treated Patients With Adult Spinal Deformity. Spine (Phila Pa 1976) 2018;43:767-73. [Crossref] [PubMed]
- Luo M, Wang P, Wang W, et al. Upper Thoracic versus Lower Thoracic as Site of Upper Instrumented Vertebrae for Long Fusion Surgery in Adult Spinal Deformity: A Meta-Analysis of Proximal Junctional Kyphosis. World Neurosurg 2017;102:200-8. [Crossref] [PubMed]
- Scheer JK, Osorio JA, Smith JS, et al. Development of Validated Computer-based Preoperative Predictive Model for Proximal Junction Failure (PJF) or Clinically Significant PJK With 86% Accuracy Based on 510 ASD Patients With 2-year Follow-up. Spine (Phila Pa 1976) 2016;41:E1328-35. [Crossref] [PubMed]
- Scheer JK, Lafage V, Smith JS, et al. Maintenance of radiographic correction at 2 years following lumbar pedicle subtraction osteotomy is superior with upper thoracic compared with thoracolumbar junction upper instrumented vertebra. Eur Spine J 2015;24 Suppl 1:S121-30. [Crossref] [PubMed]
- Banno T, Hasegawa T, Yamato Y, et al. Prevalence and Risk Factors of Iliac Screw Loosening After Adult Spinal Deformity Surgery. Spine (Phila Pa 1976) 2017;42:E1024-30. [Crossref] [PubMed]
- Fujimori T, Inoue S, Le H, et al. Long fusion from sacrum to thoracic spine for adult spinal deformity with sagittal imbalance: upper versus lower thoracic spine as site of upper instrumented vertebra. Neurosurg Focus 2014;36:E9. [Crossref] [PubMed]
- Lafage R, Ferrero E, Henry JK, et al. Validation of a new computer-assisted tool to measure spino-pelvic parameters. Spine J 2015;15:2493-502. [Crossref] [PubMed]
- Glattes RC, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976) 2005;30:1643-9. [Crossref] [PubMed]
- Baron EM, Albert TJ. Medical Complications of Surgical Treatment of Adult Spinal Deformity and How to Avoid Them. Spine (Phila Pa 1976) 2006;31:S106-18. [Crossref] [PubMed]
- Daubs MD, Lenke LG, Cheh G, et al. Adult Spinal Deformity Surgery: Complications and Outcomes in Patients Over Age 60. Spine (Phila Pa 1976) 2007;32:2238-44. [Crossref] [PubMed]
- Schwab FJ, Hawkinson N, Lafage V, et al. Risk factors for major peri-operative complications in adult spinal deformity surgery: a multi-center review of 953 consecutive patients. Eur Spine J 2012;21:2603-10. [Crossref] [PubMed]
- Glassman SD, Alegre GM. Adult spinal deformity in the osteoporotic spine: options and pitfalls. Instr Course Lect 2003;52:579-88. [PubMed]
- Yagi M, Fujita N, Tsuji O, et al. Low Bone-Mineral Density Is a Significant Risk for Proximal Junctional Failure After Surgical Correction of Adult Spinal Deformity. Spine 2018;43:485-91. [Crossref] [PubMed]
- Choi JH, Jang JS, Yoo KS, et al. Functional Limitations Due to Stiffness After Long-Level Spinal Instrumented Fusion Surgery to Correct Lumbar Degenerative Flat Back. Spine (Phila Pa 1976) 2018;43:1044-51. [Crossref] [PubMed]
- Ha Y, Maruo K, Racine L, et al. Proximal junctional kyphosis and clinical outcomes in adult spinal deformity surgery with fusion from the thoracic spine to the sacrum: a comparison of proximal and distal upper instrumented vertebrae. J Neurosurg Spine 2013;19:360-9. [Crossref] [PubMed]
- O'Shaughnessy BA, Bridwell KH, Lenke LG, et al. Does a Long-Fusion “T3-Sacrum” Portend a Worse Outcome Than a Short-Fusion “T10-Sacrum” in Primary Surgery for Adult Scoliosis? Spine (Phila Pa 1976) 2012;37:884-90. [Crossref] [PubMed]
- Soroceanu A, Burton DC, Oren JH, et al. Medical Complications After Adult Spinal Deformity Surgery: Incidence, Risk Factors, and Clinical Impact. Spine (Phila Pa 1976) 2016;41:1718-23. [Crossref] [PubMed]
- Grabel ZJ, Hart RA, Clark AJ, et al. Adult Spinal Deformity Knowledge in Orthopedic Spine Surgeons: Impact of Fellowship Training, Experience, and Practice Characteristics. Spine Deform 2018;6:60-6. [Crossref] [PubMed]
- Lau D. 326 The Impact of Surgeon Experience on Outcomes Following 3-Column Osteotomy for Adult Spinal Deformity: Overcoming the Learning Curve and Implementing Better Practices. Neurosurgery 2018;65:131. [Crossref]
- Hey HWD, Tan KA, Neo CS, et al. T9 versus T10 as the upper instrumented vertebra for correction of adult deformity-rationale and recommendations. Spine J 2017;17:615-21. [Crossref] [PubMed]
- Cho SK, Shin JI, Kim YJ. Proximal junctional kyphosis following adult spinal deformity surgery. Eur Spine J 2014;23:2726-36. [Crossref] [PubMed]


