
Soft Landing technique as a possible prevention strategy for proximal junctional failure following adult spinal deformity surgery
Introduction
Proximal junctional kyphosis (PJK) continues to be a challenging complication following adult spinal deformity (ASD) surgery with an incidence ranging from 17% to 39% (1-3). PJK refers to the development of kyphosis at the segments immediately cephalad to a spinal fusion construct. PJK manifests as a spectrum of disease severity, ranging from asymptomatic to significant pain and deformity. Most cases of PJK occur within 3 months of the postoperative period (4), and a second peak is seen after the 12-month postoperative period (5).
There is currently no consensus radiographic definition of PJK. Glattes et al. originally defined PJK as a sagittal Cobb angle between the uppermost instrumented vertebra (UIV) with two pedicle screws and two levels above the UIV (UIV+2) of 10° or greater and at least 10° greater than the preoperative measurement (6). To date, this is the most repeatedly used definition of PJK in the literature (1,7,8). There are authors who use 15° (7) or 20° (8) to define PJK, however, in this paper we used a stringent cut off of greater than 10°.
Within the spectrum of PJK, proximal junctional failure (PJF) is a more serious complication characterized by an acute structural failure such as vertebral fracture, implant failure, posterior ligament complex failure, or vertebral subluxation resulting in revision surgery (4). Its incidence was reported between 1.4% and 35% (9,10). PJF is defined in this paper as a PJK that requires extension of the construct.
The causes of PJK/PJF are not fully understood but are believed to be multifactorial. They can be categorized into surgical, radiographic, and patient-related risk factors. The surgical risk factors include among others, injury of the posterior soft tissues and variability among pedicle screw constructs. Previous investigators reasoned that ligamentous failure of the posterior interspinous ligament and paraspinal musculature damage may contribute biomechanically to increased rates of PJK (11,12). The exclusive usage of pedicles screws from the pelvis to the highest level of instrumentation results in overly rigid and stiff constructs and has been definitively shown to be a risk factor for PJK/PJF (13-15).
The purpose of this study is to report our results with the “Soft Landing” technique for ASD. This technique includes a combination of unilateral preservation of the soft tissue sleeve and contralateral instrumentation with a single hook or multiple hooks. We hypothesize the “Soft Landing” may reduce the risk of PJK/PJF by creating a less rigid transition between the pedicle screw construct and the non-instrumented upper level of the spine when compared to rates in the literature. In this study we also report a novel classification system for describing the spectrum of PJK/PJF.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jss-20-622).
Methods
Data collection
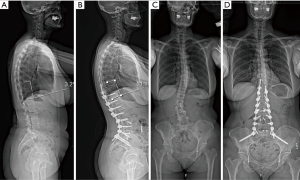
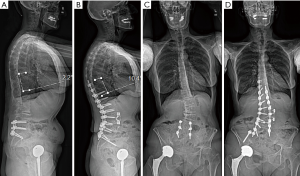
A consecutive series of 39 ASD patients undergoing instrumented fusion were included in this study. Preoperative standard standing 36-inch radiographs were utilized for radiographic measurements. Surgeries were performed from 2012 to 2018 at a single institution by the senior surgeon. Patient demographics including age, sex, BMI, indication for surgery, number of levels fused posteriorly and anteriorly, anterior and posterior approaches, bone density, use of vertebroplasty, use of cement, hook fixation type at the UIV, and 3-column osteotomy were collected. The proximal junctional angle (PJA) was measured preoperatively and at the last follow-up on standing 36-inch radiographs. Preoperative imaging was not available for 5 patients, so immediate postoperative imaging in the operating room or the post anesthesia care unit (PACU) was utilized as the reference image for PJA comparison. PJA was measured from the caudal endplate of the upper instrumented vertebra (UIV) to the cranial end plate of the vertebra two levels cranial to the upper instrumented level (UIV+2) (Figures 1,2). Two independent reviewers performed the measurements in order to minimize bias. PJK was defined as a difference in the preoperative and postoperative PJA of greater than 10°. PJF was defined as PJK that resulted in revision surgery as a direct consequence of the PJK, other causes for revision surgery such as trauma, were not considered PJF. PJF was further subdivided into two cohorts: patients requiring construct extension and those who did not. Spinopelvic parameters of sagittal alignment were measured on preoperative and most recent postoperative imaging. Measurements included pelvic tilt (PT), sagittal vertical axis (SVA), pelvic incidence-lumbar lordosis (PI-LL) mismatch, and T1 pelvic angle (TPA).
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional review board of The University of Pennsylvania (#827321) and individual consent for this retrospective analysis was waived.
Soft Landing technique
The goal of Soft Landing is to create a gradual transition from the rigid segmental instrumentation (using pedicle screws) to the native spine at the top of the construct in order to reduce the quantity of junctional stress. After deciding which levels would be the UIV, a unilateral subfascial approach of the spine is performed above the UIV. The soft tissues, including muscle and ligament attachments, are left intact on the controlateral side (Figure 3). On the spinal exposure side, one or several supralaminar (SL), infralaminar (IL) or transverse process (TP) hooks were used. A claw construct made up of a pedicle screw and hooks was also used was in some instances. The spinal tension band must always be preserved on the contralateral side when creating the contruct.

Proximal junctional classification system
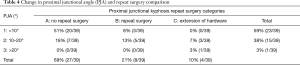
The proximal junctional classification system describes changes in PJA (UIV+2) as well as outcomes following ASD surgery at most recent follow up. Type 1 are patients with less than 10°, type 2 are patients with 10°–20° and type 3 are patients with over 20°. Modifiers A, B, or C describe whether they needed repeat surgery. Modifier A did not require repeat surgery, B required a repeat surgery but no extension, and C required an extension. Therefore patients can be 1A, 2A, 3A, 1B, 2B, 3B, 1C, 2C, 3C. According to this new classification system any patient with types 2 and 3 met the criteria for PJK. Finally, patients in group 2C and 3C met the traditional criteria for PJF.
Statistical analysis
Student t-test was utilized to perform univariate analysis of continuous variables. Chi-square test was utilized to perform univariate analysis of categorial variables. Linear regression and binary logistic regression was performed for multivariate analyses. Variables were included in the multivariate model if they were found to demonstrate a statistically significant relationship or were known factors associated with PJK and PJF. For purposes of the multivariate analysis, the UIV was categorized as upper thoracic (T1–T5) or lower thoracic (T6–T12). Statistical significance was defined as P<0.05. All analyses were performed using IBM SPSS (version 24, IBM Corp.).
Results
Patient and surgical demographics
Thirty-nine patients were included in this analysis. The mean age and BMI at the time of surgery were 61 years (range, 41–83 years) and 26.5 (range, 19–43), respectively. There were 4 men and 35 women. Twenty-five out of 39 patients had a documented Dual-energy X-ray absorptiometry (DEXA) scan in their chart, 21/25 (84%) had osteopenia/osteoporosis according to their T-score. Indications for surgery varied, with many patients having more than one diagnosis. These indications included meeting all the criteria for the ASD (scoliosis with significant coronal decompensation and/or neurogenic claudication, significant sagittal imbalance, iatrogenic flat back, adjacent-segment disease, PJK, and an extensive degenerative spinal disease). Over half (54%) of the patients underwent previous spine surgeries, and a combined anterior/lateral and posterior approach was used in 27 patients. Staged approaches were utilized in 33% of cases, with an average of 2.1 days separating the anterior/lateral and posterior surgeries. Three out of the 13 patients had the second stage after 5, 7, and 11 months due to their medical condition and were excluded from the calculation of average days between staged procedures. The mean number of levels fused posteriorly was 10 (range, 7–15), excluding the pelvis. Thirty-seven out of 39 cases were fused to the pelvis, the other two patients were both fused to L5. The UIV was upper thoracic (T1–5) in 10 cases and lower thoracic (T6–12) in 29 cases. A three-column osteotomy was performed in one case (L4 level). Sixty-nine percent of patients had anterior lumbar interbody fusion (ALIF). Vertebroplasty of the UIV was used in 9 cases. Demographics, presurgical, and surgical data are summarized in Tables 1,2. The composition of the unilateral Soft Landing at the top of the construct was diverse and is summarized in Table 3.
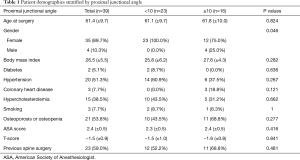
Full table
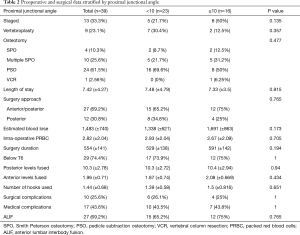
Full table

Full table
Surgical outcomes
The mean change in PJA was 8° (SD 7.4°); 23 patients had a change of less than 10°. Fifteen patients had a change in PJA of 10°–20°, and 1 patient had a change in PJA of greater than 20°. Given the accepted criteria of greater than 10° of change in PJA, 16/39 (41%) patients had radiographic PJK at most recent follow up (Table 4). Therefore there were 23 type 1 patients, 15 type 2 patients, and 1 type 3 patient. The mean time of follow-up was 2.2 years (range, 118–2,640 days). Thirty-five patients and 30 patients had at least 6 months and one-year follow-up, respectively.
Full table
The majority of patients (69%) did not require any return to the OR following soft landing procedure, including patients who met the radiographic definition of PJK. These patients who did not require repeat surgery fall into modifier A. Eight patients (21%) had modifier B and needed to return to the OR because of various complications but did not require extension of construct (broken instrumentation =4, hook removal =3, lumbar stenosis =1). Four patients (10%) required a return to the OR with extension of construct past the original level of instrumentation as well as radiographic PJK, therefore meeting the criteria for PJF (Table 4) and warranted the most serious modifer, C. The breakdown of patients into their respective classifications is demonstrated in Table 4. Mean time from index surgery to revision was 404 days.
Compression fractures at the UIV were seen in 2 cases and at the UIV+1 in 1 case for a total of 3 cases out of 39 (7.7%). Two of patients with compression fracture were asymptomatic and did not require revision surgery. The third patient with a compression fracture also had a concurrent pseudomeningocele, which required revision surgery. Spondylolisthesis was observed in one case (T2/T3 level).
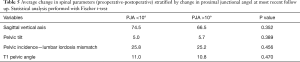
There was no statistically significant difference in the change of spinopelvic parameters between patients with PJK and patients without PJK. Average change in SVA, PT, PI-LL mismatch, and TPA are reported in Table 5.
Full table
Conclusions
The Soft Landing technique warrants further study to evaluate its impact on PJK and PJF. The use of hooks in lieu of pedicle screws at the UIV is a well-recognized PJK prevention strategy (16). Hooks provide a theoretical biomechanical advantage since they require less violation of the facet joint and provide more dynamic fixation at the cranial aspect of the construct (17,18). However, most of the hooks currently inserted in the literature are TP hooks. Because of weakened TPs in patients with pseudoarthrosis, sublaminar (SL) hooks were utilized in most cases. TP and IL hooks were utilized for 8 patients in this study only when SL hooks could not be inserted for technical reasons. Several studies have compared PJK rates in patients with spinal hooks to those with pedicle screws at the UIV (7,15,19). For example, Kim et al. reported improved rates of PJK in procedures that included hooks as compared to pedicle screws, however they did not comment on rates of PJF (15). Additionally, Helgeson et al. found a trend towards decreased rates of PJK when using hooks but never achieved significance (7). The limitations of these studies demonstrate the need for more conclusive evidence. These studies also did not utilize the technique of unilateral soft tissue dissection at the cranial end of the construct, as described in the present study. Ultimately, the make-up of the construct was determined by the senior surgeon based on clinical judgement. In future studies, a more defined methodology for construct composition will allow for more robust conclusions to be made on the benefits of Soft Landing.
It is thought that preserving the soft tissues with the Soft Landing technique as well as utilizing hooks may lower the rate of PJF. In this case series, the rate of PJF was 10% with an average follow up of 2.2 years. The senior author also performed the Soft Landing technique on patients considered to be high risk for PJK/PJF who had poor bone quality or high levels of spinal deformity preoperatively. Although, according to the literature there are certain drawbacks; similar published cases report PJF in 1.4–35% of cases (9,10,19). The difference between PJF and PJK highlights the importance of clinical outcomes as compared to radiographic outcomes. Although many of these patients had PJK as defined as PJA >10°, they did not meet the criteria for PJF, which is the more clinically relevant. A technique that has the potential to prevent reoperation warrants close inspection and further evaluation, as the complication rate following reoperation for ASD remains high.
In this paper we propose a new classification system to define the spectrum of PJK/PJK, which we call The Proximal Junctional Classification System. This system allows authors to more rigorously define PJK and PJF. The system stratifies patients based off of change in the UIV+2 and the type of repeat surgeries required. We felt that this system was necessary because patients often need to return to the OR but those return trips do not fall into the category of PJF. Many of these surgeries were outpatient surgeries that are not as difficult or time intensive as traditional PJF surgeries with an extension of the construct. According to this new classification system any patient with types 2 and 3 met the criteria for PJK. Finally, patients in group 2C and 3C met the traditional criteria for PJF. A full explanation of the system appears in the methods section. We propose that this new system will allow improved investigation, greater transparency, and clarity.
Several other surgical techniques have been proposed to help reduce the rates of PJK including utilization of cemented vertebroplasty, combined anterior and posterior approach, fusion constructs extending above T6, and the use of an ALIF. The use of vertebroplasty has demonstrated advantageous biomechanical properties but also leads to issues such as adjacent level collapse (20-24). A combined anterior and posterior approach was theorized to increase construct stability but failed to reduce the rates of PJK (25). Similarly, it was theorized that extending fusion constructs to the more rigid vertebral segments above T6 would help prevent PJK, but these results never met statistical significance (26). More recently, the use of ALIFs to restore overall alignment was thought to help reduce PJK but this technique also failed to achieve improvement (27). As has been concluded in several studies, our data demonstrated that these techniques did not have a significant effect on PJK or PJF.
The optimum number and combination of hooks utilized for the Soft Landing technique still needs to be identified. In our current cohort the average number of hooks was 1.5 in patients with PJK and 1.4 in patients who did not meet the criteria for PJK. The number of hooks utilized was determined intraoperatively and occasionally included a combination of pedicles screws and hooks. Ten different types of constructs were utilized in this case series, although the majority of cases (54%) utilized only 1 supralaminar hook. Establishing a framework for determining the optimal construct requires further investigation. It is the senior author’s belief that the soft tissue landing may work best if the unilateral soft tissue sleeve is left intact for the two contiguous upper instrumented levels and that on the instrumented sides two hooks should probably be inserted. Future studies should focus on one variation of the fusion construct, with a specific number of hooks in a particular conformation in order to determine efficacy.
There are several limitations to this study, most notably the retrospective case series study design lacking a control group, modest follow-up, and diversity of the patient population and surgical techniques. Future studies should include longer follow-up, but we believe it is important to note that most cases of PJK occur within 3 months from surgery (4). Furthermore, as the study is a case series, there is no control group without the Soft Landing technique to compare our results to. Prospective controlled trials including a larger number of patients comparing traditional constructs to the novel Soft Landing technique, described here, will help to elucidate the benefits of reducing construct rigidity at the UIV in order to prevent PJK/PJF. Because of the study design, we are unable to draw conclusions from these data, but they provide evidence that Soft Landing warrants further investigation. Other limitations of this study included the diversity of the patient population. Over half of the patients (54%) had osteoporosis, which often complicates surgical procedures in the spine. Additionally, the Soft landing was not the index procedure for over half of the patients because 54% of patients were undergoing revision surgery. Finally, the variability in surgical technique demonstrates the need for a more rigorous algorithm for treatment. Twenty-seven of these patients had combined anterior/lateral and posterior approaches and 33% of these cases were staged between the two approaches. Several different hook constructs were included in this study as well, which limits its wider applicability until a definition of Soft Landing is formalized. Future studies should occur in a more uniform patient population with a specific approach, hook construct, use of interbody, and other variables determined prior to study inclusion.
PJK and PJF are well-reported complications following ASD surgery. A new classification system has been developed to describe different grades of PJK/PJF based on PJA and need for repeat surgery. The Soft Landing technique, described here, demonstrated a mean change in PJA of 8° with 23 patients experiencing a change of less than 10° (type 1). 10% of patients included in the study required revision surgery for PJF (type 2C and 3C) with a mean follow up of 813 days. Authors believe that this new classification system has enabled them to better categorize and treat PJK/PJF. Although further evaluation is required, the Soft Landing technique represents a potential and effective prevention strategy for PJK and PJF.
Acknowledgments
Abstract was previously presented at North American Spine Society 34th Annual Meeting, September 25–28, 2019, Chicago, IL.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jss-20-622
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jss-20-622
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss-20-622). CS has stock ownership of Vertera Spine. VA is a paid consultant for Depuy, Zimmer, Nuvasive, Medtronic, and Camber. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional review board of The University of Pennsylvania (#827321) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hostin R, McCarthy I, O’Brien M, et al. Incidence, mode, and location of acute proximal junctional failures after surgical treatment of adult spinal deformity. Spine (Phila Pa 1976) 2013;38:1008-15. [Crossref] [PubMed]
- Yagi M, Akilah KB, Boachie-Adjei O. Incidence, risk factors and classification of proximal junctional kyphosis: Surgical outcomes review of adult idiopathic scoliosis. Spine (Phila Pa 1976) 2011;36:E60-8. [Crossref] [PubMed]
- Kim YJ, Bridwell KH, Lenke LG, et al. Proximal Junctional Kyphosis in Adult Spinal Deformity After Segmental Posterior Spinal Instrumentation and Fusion. Spine (Phila Pa 1976) 2008;33:2179-84. [Crossref] [PubMed]
- Yagi M, King AB, Boachie-Adjei O. Incidence, risk factors, and natural course of proximal junctional kyphosis: Surgical outcomes review of adult idiopathic scoliosis. minimum 5 years of follow-up. Spine (Phila Pa 1976) 2012;37:1479-89. [Crossref] [PubMed]
- Daniels AH, Bess S, Line B, et al. Peak Timing for Complications After Adult Spinal Deformity Surgery. World Neurosurg 2018;115:e509-e515. [Crossref] [PubMed]
- Glattes RC, Bridwell KH, Lenke LG, et al. Proximal Junctional Kyphosis in Adult Spinal Deformity Following Long Instrumented Posterior Spinal Fusion. Spine (Phila Pa 1976) 2005;30:1643-9. [Crossref] [PubMed]
- Helgeson MD, Shah SA, Newton PO, et al. Evaluation of proximal junctional kyphosis in adolescent idiopathic scoliosis following pedicle screw, hook, or hybrid instrumentation. Spine (Phila Pa 1976) 2010;35:177-81. [Crossref] [PubMed]
- Bridwell KH, Lenke LG, Cho SK, et al. Proximal junctional kyphosis in primary adult deformity surgery: Evaluation of 20 degrees as a critical angle. Neurosurgery 2013;72:899-906. [Crossref] [PubMed]
- Yang J, Khalifé M, Lafage R, et al. What Factors Predict the Risk of Proximal Junctional Failure in the Long Term, Demographic, Surgical, or Radiographic?: Results from a Time-dependent ROC Curve. Spine (Phila Pa 1976) 2019;44:777-84. [Crossref] [PubMed]
- Lau D, Clark AJ, Scheer JK, et al. Proximal junctional kyphosis and failure after spinal deformity surgery: A systematic review of the literature as a background to classification development. Spine (Phila Pa 1976) 2014;39:2093-102. [Crossref] [PubMed]
- Cammarata M, Aubin CÉ, Wang X, et al. Biomechanical risk factors for proximal junctional kyphosis: A detailed numerical analysis of surgical instrumentation variables. Spine (Phila Pa 1976) 2014;39:E500-E507. [Crossref] [PubMed]
- Arlet V, Aebi M. Junctional spinal disorders in operated adult spinal deformities: present understanding and future perspectives. Eur Spine J 2013;22:S276-S295. [Crossref] [PubMed]
- Kim YJ, Bridwell KH, Lenke LG, et al. Is the T9, T11, or L1 the more reliable proximal level after adult lumbar or lumbosacral instrumented fusion to L5 or S1? Spine (Phila Pa 1976) 2007;32:2653-61. [Crossref] [PubMed]
- Watanabe K, Lenke LG, Bridwell KH, et al. Proximal junctional vertebral fracture in adults after spinal deformity surgery using pedicle screw constructs: Analysis of morphological features. Spine (Phila Pa 1976) 2010;35:138-45. [Crossref] [PubMed]
- Kim YJ, Lenke LG, Bridwell KH, et al. Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: Incidence and risk factor analysis of 410 cases. Spine (Phila Pa 1976) 2007;32:2731-8. [Crossref] [PubMed]
- Matsumura A, Namikawa T, Kato M, et al. Effect of different types of upper instrumented vertebrae instruments on proximal junctional kyphosis following adult spinal deformity surgery: Pedicle screw versus transverse process hook. Asian Spine J 2018;12:622-31. [Crossref] [PubMed]
- Lange T, Schmoelz W, Gosheger G, et al. Is a gradual reduction of stiffness on top of posterior instrumentation possible with a suitable proximal implant? A biomechanical study. Spine J 2017;17:1148-55. [Crossref] [PubMed]
- Metzger MF, Robinson ST, Svet MT, et al. Biomechanical analysis of the proximal adjacent segment after multilevel instrumentation of the thoracic spine: Do hooks ease the transition? Global Spine J 2016;6:335-43. [Crossref] [PubMed]
- Hassanzadeh H, Gupta S, Jain A, et al. Type of anchor at the proximal fusion level has a significant effect on the incidence of proximal junctional kyphosis and outcome in adults after long posterior spinal fusion. Spine Deform 2013;1:299-305. [Crossref] [PubMed]
- Ghobrial GM, Eichberg DG, Kolcun JPG, et al. Prophylactic vertebral cement augmentation at the uppermost instrumented vertebra and rostral adjacent vertebra for the prevention of proximal junctional kyphosis and failure following long-segment fusion for adult spinal deformity. Spine J 2017;17:1499-505. [Crossref] [PubMed]
- Kayanja MM, Togawa D, Leiberman IH. Biomechanical changes after the augmentation of experimental osteoporotic vertebral compression fractures in the cadaveric thoracic spine. Spine J 2005;5:55-63. [Crossref] [PubMed]
- Kebaish KM, Martin CT, O’Obrien JR, et al. Use of Vertebroplasty to prevent proximal junctional fractures in adult deformity surgery: a biomechanical cadaveric study. Spine J 2013;13:1897-903. [Crossref] [PubMed]
- Verlaan JJ, Oner FC, Slootweg PJ, et al. Histologic changes after vertebroplasty. J Bone Jt Surg - Ser A 2004;86:1230-8.
- Fribourg D, Tang C, Sra P, et al. Incidence of subsequent vertebral fracture after kyphoplasty. Spine (Phila Pa 1976) 2004;29:2270-6. [Crossref] [PubMed]
- Kim HJ, Yagi M, Nyugen J, et al. Combined anterior-posterior surgery is the most important risk factor for developing proximal junctional kyphosis in idiopathic scoliosis. Clin Orthop Relat Res 2012;470:1633-9. [Crossref] [PubMed]
- Fu X, Sun XL, Harris JA, et al. Long fusion correction of degenerative adult spinal deformity and the selection of the upper or lower thoracic region as the site of proximal instrumentation: A systematic review and meta-analysis. BMJ Open 2016;6:e012103. [Crossref] [PubMed]
- Bae J, Theologis AA, Strom R, et al. Comparative analysis of 3 surgical strategies for adult spinal deformity with mild to moderate sagittal imbalance. J Neurosurg Spine 2018;28:40-9. [Crossref] [PubMed]


