
Spinal surgery during the COVID-19 pandemic: the experience in a tertiary referral centre
Introduction
Since December 2019, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has become one of the biggest global health issues seen, and is now commonly known as COVID-19 (1). It was declared a pandemic by the World Health Organisation on 11th March 2020 (2). Subsequently, the United Kingdom has been one of the worst affected countries, with over 47,742 COVID-19 related deaths, and over 1,099,059 confirmed cases up to November 2020 (3).
In an effort to cope with the pandemic, a consensus of expert opinion was sought in order to produce national guidelines for surgeons operating in the COVID-19 pandemic, which included the cessation of elective operating (4). The National Health Service produced guidelines for the organisation of spinal services in response to the pandemic on 20th March 2020, with the advice that “most elective spinal surgery can be delayed until further notice with minimal risk to the patient” (5). Further guidance from the Royal College of Surgeons aimed to stratify which emergency procedures should be carried out, and in what time frame. Their advice was for cauda equina syndrome, acute metastatic spinal cord compression or unstable spinal fractures with neurological deficit to be operated on within 24 hours, unstable spinal fractures without neurological compression within 72 hours, and progressive degenerative cases within one month (6).
The aim was to reduce elective procedures, thereby reducing the burden of care for post-operative patients, which freed up operating theatres to be used as higher care areas, ventilators for use, personal protective equipment (PPE) stocks, inpatient beds and medically trained personnel for re-deployment if needed (7).
Our unit is a tertiary referral centre for complex spinal surgery, and consists of both orthopaedic and neuro-surgical spinal Consultants, serving a population of approximately 3.2 million people (8). We aimed to assess the impact COVID-19 had on our spinal service, looking at the number of procedures performed, 30-day mortality rates, timing to theatre, length of stay, and rate of COVID-19 infections in our patient population.
Methods
We performed a prospective cohort study of all of the patients in our spinal unit undergoing operative intervention after the moratorium on elective operating was announced (5), for the proceeding three months, up until 10th June 2020, a period of 82 days. These were retrospectively compared with a control population from the same time period in 2019.
All operative cases were identified using the electronic theatre database Theatreman (Trisoft, UK). Patient demographics were extracted from this, and their care records on the Electronic Patient Records Sunrise (Allscripts, UK) was interrogated for admission data, operative details, COVID-19 diagnosis, and any complications including 30-day mortality rates. A Patient Administration System (PAS) enquiry was then performed to confirm the mortality rate, and to identify any subsequent deaths post-discharge. For the patients that died during their hospital stay at our Trust, cause of death was available on their electronic patient record. When the patient had died after discharge from our Trust, the cause of death was not available on our electronic records (one case), and was confirmed through the patient’s General Practice who were able to provide this information.
Laboratory testing for COVID-19 was routinely performed for all patients admitted for operative procedures, and also post-operatively if there was any clinical suspicion of COVID-19 transmission. In some cases, due to the time critical nature of the pathology, and before rapid COVID testing was available, the operating surgeon was unable to wait for the results of the testing. In these cases, they were treated as potentially positive, and all precautions were taken as if they were positive. The testing involved testing for SARS-CoV-2 viral RNA using polymerase chain reaction (PCR) techniques. In the initial stages of the pandemic, computed tomography (CT) scans of the chest were also performed to look for signs of COVID pneumonia.
Patients were managed in cohorts within the hospital according to COVID status. Those with a proven negative SARS-CoV-2 were treated in “Green” wards with standard precautions and tests repeated every three days, and as indicated by symptoms. Patients were tested for SARS-CoV-2 on admission to the hospital. Those awaiting the results of this were managed as “Amber” patients, and were treated in side-rooms with full precautions until their COVID status had been confirmed. Patients with a positive SARS-CoV-2 were managed in “Blue” areas separate to the general hospital population, and with full precautions; including FFP3 face masks, eye protection and impervious gowns, with designated donning and doffing areas4.
Statistical analysis
Statistical analysis was performed using unpaired t test to assess for significant differences in continuous data, and chi-square for categorical data, using 95% confidence intervals between the COVID-19 cohort and control cohort from 2019. The cases identified were sub-stratified as those needing spinal instrumentation or not, and a sub-group analysis was performed.
Ethical statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethics Committee approval was not required as this was a retrospective observational study using routinely collected data, did not affect patient care, and contains no patient identifiable data. Informed consent was not obtained from patients as this was a retrospective observational study using routinely collected data. The study did not affect patient care, and contains no patient identifiable data.
Results
In the 82-day study period covering the COVID-19 pandemic, 78 operative cases were performed, of which 38 (49%) were instrumented cases. The median age for all cases was 51.8 years (IQR 36.25–64.75), the instrumented population were significantly older than the non-instrumented population. There were 41 males and 37 females who underwent operative intervention (Table 1).

Full table
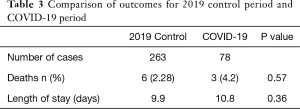
There were significantly fewer operative cases performed during the COVID-19 period (n=78) compared to three times the number of cases performed in the corresponding period in 2019 (n=263).
The most common indication for surgical intervention in the COVID-19 period was for acute decompression (39 cases, 50% of all), followed by trauma (Table 2). The cases were split into one of four categories; trauma, infection, malignancy and degenerative. Degenerative is quite a broad term, and included degenerative cervical disc disease, cervical stenosis including myelopathy, thoracic stenosis, lumbar stenosis and lumbar disc disease (Figure 1). The individual levels operated on can be seen in Figures 2 and 3, with the L4/5 level being the most common. The median number of spinal levels involved in the instrumented category was three.
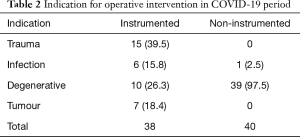
Full table
There were three patients who were found to have died within the COVID-19 pandemic period, giving a 30-day mortality rate of 4.2%, with one in the instrumented cohort (2.6%), and two in the non-instrumented cohort (5.0%). This difference was not statistically significantly. Five patients (6.4%) overall tested positive for SARS-Cov-2 RNA, with 3 (7.9%) in the instrumented group, and 2 (5.0%) in the non-instrumented group, with no significant difference. No patients who tested positive for SARS-CoV-2 pre-operatively underwent surgical intervention, and one patient underwent stabilization for infection who had initially tested positive for SARS-CoV-2, and after initial treatment with antibiotics, went on to test negative and then received surgical intervention.
There was a higher 30-day mortality rate amongst the patients operated in the COVID-19 period compared to the 2019 control population (4.2% vs. 2.28%). This did not achieve statistical significance (Table 3).
Full table
The mean time from admission to theatre was 3.7 days, with the non-instrumented cases waiting less on average (2.1 days) compared to the instrumented (5.4 days). The average length of stay for operative cases in the period studied was 10.8 days, with non-instrumented cases having a shorter length of stay (2.1 days) compared to the instrumented cases (14.9 days) (P<0.0001).
The average length of stay was slightly higher during the COVID-19 period compared to that in 2019 (10.8 vs. 9.9 days), but again, this was not statistically significant (Table 3).
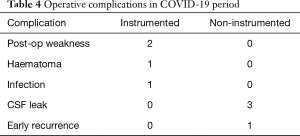
Not including death, there were 8 operative complications observed (10.3%) in the COVID-19 cohort, which were evenly distributed as 4 in each group (Table 4).
Full table
Discussion
Due to the moratorium on elective operative imposed as a result of the COVID-19 pandemic, the operative cases performed in our tertiary referral unit fell by almost one-third. This is to be expected, due to the guidance given by NHS England.
For those patients who did undergo operative intervention during the COVID-19 period, there was a slightly higher 30-day mortality rate compared to 2019, but this was not significant. This may be explained by the fact that none of the patients operated on had tested positive for SARS-CoV-2. One patient did test positive, but the decision was made to delay surgical intervention until they had recovered from their SARS-CoV-2 infection, and tested negative. This decision was informed by using the available evidence at the time, suggesting a 23.8% 30-day mortality rate for those patients undergoing surgical intervention who tested positive for SARS-CoV-2 (9). The patient was deemed able to wait until recovery from COVID-19, as they had stable neurology, was being treated for spondylodiscitis with intra-venous antibiotics, and had stable inflammatory markers without systemic features of sepsis.
The length of stay was longer for patients operated in the COVID-19 period (10.8 vs. 9.9 days), but this was not statistically significant. The reason for this slight increase in length of stay could be that during the COVID-19 pandemic period, almost all of the cases operated on were emergency admissions, including cauda equina syndrome, fractures, metastatic cord compression and infections. These cases would still have been seen during the 2019 control period, but the average length of stay will have been reduced by the elective cases performed in this period, such as the planned elective discectomies and micro-decompressions. Due to complex cases making up a higher proportion of the cases operated on, these would tend to have a longer length of stay in hospital post-operatively.
Of the patients who died during the COVID-19 period, two of them had their cause of death attributed to SARS-CoV-2 infection, which was contracted post-operatively in both cases. This gave a 30-day mortality due to SARS-CoV-2 infection of 2.56% in our population. The remaining patient had a cardiac related cause of death. As noted previously, no patient who underwent surgical intervention was known to be positive for SARS-CoV-2 RNA at the time of operative intervention. This finding supports the evidence from Giorgio et al. in Italy, who operated on 19 patients during this time, none of whom tested positive for SARS-CoV-2 (10).
There was no statistically significant difference in the distribution of the patients who tested positive for SARS-CoV-2 RNA between the instrumented and non-instrumented cohorts, or in the time from admission to operation in the two groups. The mean time to theatre was shorter for the non-instrumented cases, but a few cases, such as the patient testing positive for SARS-CoV-2 who was managed conservatively until they tested negative, could be a confounding factor affecting these results.
With regards to the instrumented and non-instrumented cases performed during the COVID-19 pandemic period, the instrumented cases were found to have a significantly longer length of stay (14.9 vs. 2.1 days). This did achieve statistical significance, and would be expected as the instrumented cases, including stabilization for trauma, infection and tumour, have a much larger physiological impact compared to, for example, the decompressions for cauda equina syndrome. The instrumented cases are also associated with a prolonged course of rehabilitation, and the need for post-operative antibiotics in the cases of infection. This is backed up by existing literature, suggesting spinal instrumentation is a predictor for longer length of stay (11).
The complication rate in our unit during the COVID-19 period was found to be 10.3%. A systematic review performed in 2010 suggests that based on 79,471 patients undergoing spinal surgery, an overall complication rate of 16.4% was identified (12). This suggests that our complication rate is lower than that found in the literature, despite the restrictions found with operating in full PPE during the COVID-19 pandemic (7).
One limitation of this data set is that the COVID-19 sample size is small, at 78 cases. This may mean that the study is under-powered to detect any significant difference in 30-day mortality rates between the two populations. The only way to improve this and reduce the risk of type II error, would be to collaborate and pool data with other similar spinal units, in order to improve the sample size.
Conclusions
The global pandemic caused by severe acute respiratory syndrome coronavirus 2 has had a huge impact on health-care provision as a whole, and also on spinal services. The number of operative cases performed in our tertiary unit fell by one-third during the pandemic period. Despite the fear that mortality would increase in our patient population, our data shows no significant difference in mortality rates for those operated on during the COVID-19 pandemic, and the same time in 2019. Similarly, there was no significant difference in length of stay between the two time periods, or in complication rates when compared with the existing literature. Patient selection may have played a factor in our favourable 30-day mortality rates, and longer-term studies are needed to demonstrate the full impact of the COVID-19 pandemic on spinal services.
Acknowledgments
Funding: None.
Footnote
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jss-20-643
Peer Review File: Available at http://dx.doi.org/10.21037/jss-20-643
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss-20-643). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethics Committee approval was not required as this was a retrospective observational study using routinely collected data, did not affect patient care, and contains no patient identifiable data. Informed consent was not obtained from patients as this was a retrospective observational study using routinely collected data. The study did not affect patient care, and contains no patient identifiable data.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zhu N, Zhang D, Wang W, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med 2020;382:727-33. [Crossref] [PubMed]
- World Health Organisation. WHO announces COVID-19 outbreak a pandemic. March 12, 2020. Available online: covid-19-outbreak-a-pandemic (accessed July 10th, 2020).http://www.euro.who.int/en/health-topics/healthemergencies/coronavirus-covid-19/news/news/2020/3/whoannounces-
- HM Government. Coronavirus (COVID-19) in the UK. July 9, 2020. Available online: (accessed November 5th, 2020)https://coronavirus.data.gov.uk
- COVIDSurg Collaborative. Global guidance for surgical care during the COVID-19 pandemic. Br J Surg 2020;107:1097-103. [Crossref] [PubMed]
- National Health Service. Clinical guide for the management of patients requiring spinal surgery during the Coronavirus pandemic, March 20, 2020. Available online: (accessed July 10th 2020)https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/specialty-guide-management-of-patients-requiring-spinal-surgery-v1-20-march-2020.pdf
- Federation of Surgical Specialty Associations. Clinical Guide to Surgical Prioritisation During the Coronavirus Pandemic, June 26, 2020. Available online: (accessed July 10th 2020)https://www.rcseng.ac.uk/coronavirus/surgical-prioritisation-guidance/
- Jain NS, Alluri RK, Schopler SS, et al. COVID-19 and Spine Surgery: A Review and Evolving Recommendations. Global Spine J 2020;10:528-33. [Crossref] [PubMed]
- Greater Manchester Neuro-Sciences Centre, Salford, UK. Available online: (accessed July 10, 2020)https://www.srft.nhs.uk/about-us/depts/neuro-surgery/pts/neurosurgical-spinal-services/
- COVIDSurg Collaborative. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet 2020;396:27-38. [Crossref] [PubMed]
- Giorgi PD, Villa F, Gallazzi E, et al. The management of emergency spinal surgery during the COVID-19 pandemic in Italy. Bone Joint J 2020;102-B:671-6. [Crossref] [PubMed]
- Kobayashi K, Ando K, Kato F, et al. Trends of postoperative length of stay in spine surgery over 10 years in Japan based on a prospective multicenter database. Clin Neurol Neurosurg 2019;177:97-100. [Crossref] [PubMed]
- Nasser R, Yadla S, Maltenfort MG, et al. Complications in spine surgery. J Neurosurg Spine 2010;13:144-57. [Crossref] [PubMed]





