
Staged two level non-contiguous vertebral column resection: technique and case report
Introduction
Spinal deformity is a complex issue that can lead to global spine imbalance with subsequent neurologic deficits, clinical deformity and chronic back pain (1). The recent advancement in deformity correction using improved surgical instrumentation and vertebral osteotomy techniques now allow for significant correction of sagittal and coronal malalignment that was previously unachievable in the past. In particular, the vertebral column resection (VCR) osteotomy technique is used in select cases of rigid severe spinal deformities to achieve significant curve correction.
The clinical outcomes from VCR were first reported in 1987 by Bradford et al., who initially described the technique as a circumferential apical VCR leading to significant curve correction (2). The anterior-posterior VCR evolved to the posterior-based VCR (PVCR), which was first described by Suk et al. in 2002 to allow similar curve correction while decreasing surgical time and blood loss (3). Among the different vertebral osteotomies, the PVCR allows the most impressive curve correction, but is also with higher morbidity rates (4-8). Therefore, the PVCR is typically reserved for severe rigid thoracic spinal deformity that is otherwise uncorrectable with lesser osteotomies (9,10). Given the magnitude of preoperative planning and technically challenging operative technique involved with the PVCR, there is currently limited literature for two level non-contiguous VCR. This case report will present a previously undiagnosed ankylosing spondylitis (AS) patient with a previously fused spine in marked coronal and sagittal malalignment that required a staged two level non-contiguous VCR for treatment of his fixed thoracic and cervicothoracic kyphoscoliosis.
We present the following case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/jss-20-656.
Results: case description
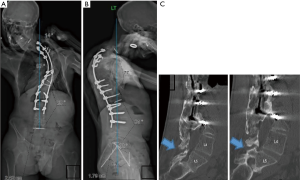
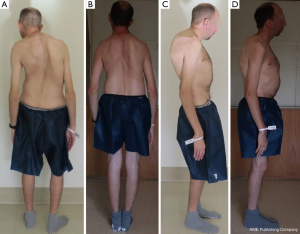
The patient is a 37-year-old male with a history of AS discovered only after his initial spinal reconstruction, who previously underwent posterior spinal instrumentation and fusion (PSIF) T3-L3 in 2008 now presenting with progressively worsening fixed thoracic and cervicothoracic kyphoscoliosis 10 years after initial surgery. He had a history of heart palpitation in the past, but was otherwise healthy. His physical exam was significant for radicular pain along the posterior aspect of his right arm, chronic back pain, truncal shift and worsening forward flexion deformity of his neck which was shifted and severely tilted forward and to the left (Figure 1). He had only minimal motion of his upper neck, and was otherwise fixed in his alignment and posture from his upper cervical spine to his pelvis. His forward gaze was downward and this led to difficulty using a computer monitor for his work. His standing anteroposterior (AP) and lateral spine films in his first office visit showed global sagittal and coronal malalignment with severe rigid thoracic kyphoscoliosis (head off to the left by 8 cm, proximal thoracic curve measuring at 87˚ in the coronal plane and 77˚ in the sagittal plane) (Figure 1A,B). The preoperative CT scan showed pseudoarthrosis between L4 and L5, but otherwise globally fused spine from the AS and PSIF.
We planned a staged reconstruction on him, initially addressing his alignment from the sacrum/pelvis to the upper thoracic spine, then a second stage to optimize his skull position on his cervical-thoracic spine. He was taken to the OR for stage 1: revision PSIF T1-pelvis with VCR T7-T8, transforaminal lumbar interbody fusion (TLIF) L4-5, and peri-apical posterior column osteotomies (PCOs). The patient was positioned prone using the OSI Jackson table with adequate padding to avoid excessive pressure points. We used Gardener-Wells tong traction (15 lbs) with his neck in neutral position. He was given prophylactic doses of Ancef and gentamycin and tranexamic acid (50 mg/kg loading dose and 5 mg/kg per hour maintenance dose) to decrease bleeding. Neuromonitoring was utilized for both procedures.
Once adequate bony spine anatomy was exposed after careful subperiosteal dissection to avoid unnecessary bleeding, we confirmed solid fusion from T1-L4, motion pseudoarthrosis at L4-5 and solid fusion again from L5-sacrum. All pedicle screws (inserted using the freehand technique) and distal implantation, including TLIF at L4-5 and bilateral S2 iliac screws (inserted using the freehand technique), were placed and confirmed with intraoperative CT scan prior to approaching the planned VCR site at T7-8 (11,12). To avoid spinal subluxation during the VCR, a temporary rod was placed using a 5.5 mm cobalt chrome rod on the right side 4 levels above and 3 levels below T7 and, similarly, a temporary rod was placed at the left side 3 levels above and 3 levels below T7. Once temporary fixation was completed, we performed wide laminectomy starting from the inferior T6 lamina to superior T9 lamina. Peri-apical PCO at T9-10 further mobilized the spine allowing for harmonious curve correction.
The T7 and T8 vertebral bodies were accessed after removing the right (convex) T7 and T8 pedicles and gaining further exposure by resecting 5 cm of the right medial 6th, 7th, and 8th ribs. The right T7 nerve root was also ligated after clamping it for 5 minutes to confirm absence of iatrogenic spinal cord blood supply injury (13). For kyphoscoliotic deformity, the majority of the vertebral body is removed from the convex side (right side for this case), because the vertebral body is rotated lateral and dorsal at the apex of the convexity. With adequate visualization, we began decancellation the T7 and T8 vertebral bodies from the right side and removed the T7 and T8 vertebral bodies via lateral extracavitary corpectomy. We removed the majority of the vertebral bodies except for the thin rim of the anterior walls for stability and fusion purposes.
After confirming stable spinal cord data, subperiosteal dissection at the concave side was carried out after removing the left temporary rod. The left T7 and T8 pedicles were removed using a small high-speed power burr since the apical concave pedicles are typically very cortical. This freed up the spinal cord which was resting on the medial apical pedicles as previously described in literature for scoliotic deformities (13). The lateral vertebral body at the left side was removed and the posterior wall impactor was used to carefully remove the posterior wall from the ventral spinal cord.
At this point, the resection was complete and correction across the resected T7-8 vertebral bodies was sequentially performed first with convex compression to shorten the apex and provide the spinal cord less tension, followed by concave distraction. The apical spinal column was thus shortened during this procedure and the main correcting technique is the convex compression. After adequate curve correction, the right side temporary rod was exchanged with a permanent rod going from T1 to L1. We then used the domino to connect the rod from L2 to the S2AI screw. Afterwards, an 18×18 mm large custom VCR cage was placed in the defect between T6 and T9 for anterior fusion and compressed to lock it in place. Bone morphogenic protein (BMP) was also added into the VCR site. The left side permanent rod (6.0 to 5.5 mm cobalt chrome plus hybrid rod) was placed after the cage insertion. Both rods were further supplemented with hook rod constructs (5.5 mm cobalt chrome from T2 to T11), which allowed 4 rods to cross the VCR site for extra stability at the 2 level VCR site. All implant position and realignment were confirmed with intraoperative total spine radiographs and the spinal cord data was stable throughout.
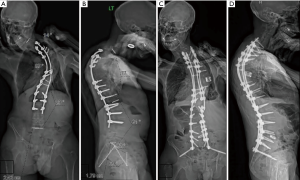
The patient’s postoperative course was significant for right pleural effusion and complete atelectasis requiring supplemental oxygen and eventually re-intubation on postoperative day (POD) 3. His net fluid balance on POD 1 was +750 cc and POD 2 was −227 cc, which most likely contributed to his fluid overload. He was uneventfully extubated on POD 4 and discharged on POD 7 with standing films demonstrating markedly improved global spinal alignment (Figure 2A,B,C,D). He recovered well from this initial reconstructive VCR surgery, and returned to office 5 months postoperatively with persistent discomfort in his right neck down his right shoulder and coronal imbalance due to cervicothoracic curvature as we had expected. He had difficulty managing his neck pain which kept him awake at night and prevented activity of daily living. The standing films from his initial office visit to his 6-month follow-up visit showed improved coronal and sagittal balance, but persistent neck tilt and shift with worsening proximal junctional kyphosis (PJK). With his persistent postoperative pain and discomfort coming from the residual cervicothoracic kyphoscoliosis and worsening PJK in his autofused spine, we moved forward to the second stage of his planned reconstruction for an extension PSIF C2-T6 and T2 VCR to further improve and optimize his overall skull and global spinal alignment. The plan for the T2 VCR coincides with the work done by Koller et al. who showed that adequate thoracic spine correction in patients with AS is only possible when there is residual mobility at the sternocostal junctions at T4-9 or when the three column osteotomy is at T1-T3 and T10-T12 with rib osteotomies (10).
During the second stage of his reconstruction, he was placed in halo traction using 10 lbs to further stabilize his skull and neck. His old incision was extended proximally and subperiosteal dissection was carried out in usual fashion to expose from C2 to T12. We first addressed the decompression at C6-7 to free up the C7 nerve roots at the site of pseudarthrosis confirmed on a preoperative CT scan. After adequate exposure, bilateral C2 pars screws, C3-6 lateral mass screws, and C7-T4 pedicle screws were placed. The T1-T4 screws were replaced with larger diameter screws. All screw positions were confirmed with intraoperative CT scan prior to the T2 VCR.
The preparation for the T2 VCR began with bilateral temporary rod placement from C7-T4. The T2 VCR was completed in similar fashion as his previous VCR, first starting with bilateral laminectomies from inferior T1 lamina to superior T3 lamina. Since the convex side was on the left on the cervicothoracic curve, the T2 vertebral body was first resected through the left T2 pedicle and then through the right T2 pedicle. The right (concave) T2 pedicle was removed using a small high-speed power burr, which freed up the spinal cord. After complete resection of the T2 vertebral body, we did multiple rounds of sequential convex compression and concave distraction after placing the final rods with appropriate sagittal bend to shorten and adequately align the spine. Once the implants and curve correction were deemed satisfactory after reviewing the intraoperative fluoroscopic imaging, an 8×25 mm titanium crescent cage was press-fit into the defect anteriorly between T1-3. The VCR site was further stabilized with four 5.5 mm cobalt chrome rods and one 3.5 mm cobalt chrome rod. We used the off-set connectors on the main rods at the level of the VCR to add these additional rods in an efficient manner. The cervicothoracic deformity correction was achieved with proper patient head positioning using the halo traction and adequate rod contouring and positioning based on the senior author’s previous experience and expertise. All implant position was confirmed with intraoperative radiographs stitched to view the entire spine from the skull to the sacrum/pelvis for adequate coronal and sagittal global balance and the spinal cord data was stable throughout.
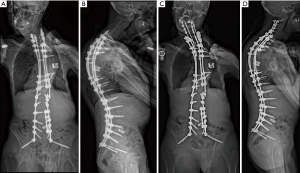
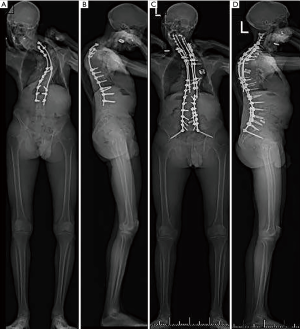
The patient did well postoperatively and was discharged on POD 3 after obtaining standing films, which showed improved coronal and sagittal imbalance with PJK correction (Figure 3A,B,C,D). After both his surgeries, the patient was given Enoxaprin 40 mg once a day as an inpatient for deep vein thrombosis prophylaxis. He most recently followed up for his 1 year follow-up with no major complications and improvements in clinical and radiographic global balance and SRS and ODI scores (Figures 4-6; Tables 1,2).
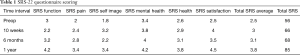
Full table
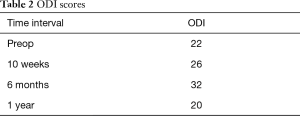
Full table
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient. CUMC IRB approved protocol # AAAR1866 for informed consent.
Conclusions
In this patient with ankylosing spondylitis, a postoperative rigid thoracic kyphoscoliosis, and marked truncal imbalance and skull to pelvis imbalance a 2-level non-contiguous VCR performed in a staged fashion at the apex of the thoracic curve and subsequently at the apex of the cervicothoracic curve were utilized to restore sagittal and coronal imbalance and improved skull position and optimal visual gaze. The need for performing two non-contiguous VCR is quite rare and necessary only in a small subset of deformity patients with rigid curves causing malignment in different areas of the spine. Prior to undertaking such an endeavor, the spine surgeon must be aware of his or her expertise with the surgical techniques involving the VCR. The non-contiguous VCR surgery is challenging but also capable of correcting even the most rigid and severe spine deformity with appropriate planning and optimal surgical technique.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/jss-20-656
Peer Review File: Available at http://dx.doi.org/10.21037/jss-20-656
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss-20-656). LGL serves as an unpaid editorial board member of Journal of Spine Surgery from Oct 2019 to Oct 2021. Dr. LGL reports personal fees from Medtronic, grants and personal fees from DePuy-Synthes Spine, personal fees from K2M, non-financial support from Broadwater, non-financial support from Seattle Science Foundation, grants and non-financial support from Scoliosis Research Society, non-financial support from Stryker Spine, non-financial support from The Spinal Research Foundation, grants from EOS, grants from Setting Scoliosis Straight Foundation, personal fees from Fox Rothschild, LLC, personal fees from Quality Medical Publishing, other from Evans Family Donation, other from Fox Family Foundation, grants and non-financial support from AOSpine, outside the submitted work; Dr. LGL reports personal fees from Medtronic, grants and personal fees from DePuy-Synthes Spine, personal fees from K2M, non-financial support from Broadwater, non-financial support from Seattle Science Foundation, grants and non-financial support from Scoliosis Research Society, non-financial support from Stryker Spine, non-financial support from The Spinal Research Foundation, grants from EOS, grants from Setting Scoliosis Straight Foundation, personal fees from Fox Rothschild, LLC, personal fees from Quality Medical Publishing, other from Evans Family Donation, other from Fox Family Foundation, grants and non-financial support from AOSpine, outside the submitted work. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient. CUMC IRB approved protocol # AAAR1866 for informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Good CR, Auerbach JD, O’Leary PT, Schuler TC. Adult spine deformity. Curr Rev Musculoskelet Med 2011;4:159-67. [Crossref] [PubMed]
- Bradford D. Vertebral Column Resection. Orthop Trans 1987;11.
- Suk SI, Kim JH, Kim WJ, et al. Posterior vertebral column resection for severe spinal deformities. Spine (Phila Pa 1976) 2002;27:2374-82. [Crossref] [PubMed]
- Enercan M, Ozturk C, Kahraman S, et al. Osteotomies/spinal column resections in adult deformity. Eur Spine J 2013;22 Suppl 2:S254-64. [Crossref] [PubMed]
- Lenke LG, Newton PO, Sucato DJ, et al. Complications after 147 consecutive vertebral column resections for severe pediatric spinal deformity: A multicenter analysis. Spine (Phila Pa 1976) 2013;38:119-32. [Crossref] [PubMed]
- Lenke LG, Sides BA, Koester LA, et al. Vertebral column resection for the treatment of severe spinal deformity. Clin Orthop Relat Res 2010;468:687-99. [Crossref] [PubMed]
- Papadopoulos EC, Boachie-Adjei O, He`ss WF, et al. Early outcomes and complications of posterior vertebral column resection. Spine J 2015;15:983-91. [Crossref] [PubMed]
- Suk SI, Chung ER, Lee SM, et al. Posterior vertebral column resection in fixed lumbosacral deformity. Spine (Phila Pa 1976) 2005;30:E703-10. [Crossref] [PubMed]
- Dorward IG, Lenke LG. Osteotomies in the posterior-only treatment of complex adult spinal deformity: a comparative review. Neurosurg Focus 2010;28:E4. [Crossref] [PubMed]
- Koller H, Koller J, Mayer M, et al. Osteotomies in ankylosing spondylitis: where, how many, and how much? Eur Spine J 2018;27:70-100. [Crossref] [PubMed]
- Kim YJ, Lenke LG, Bridwell KH, et al. Free Hand Pedicle Screw Placement in the Thoracic Spine: Is it Safe. Spine (Phila Pa 1976) 2004;29:333-42; discussion 342. [Crossref] [PubMed]
- Shillingford JN, Laratta JL, Tan LA, et al. The Free-Hand Technique for S2-Alar-Iliac Screw Placement: A Safe and Effective Method for Sacropelvic Fixation in Adult Spinal Deformity. J Bone Joint Surg Am 2018;100:334-42. [Crossref] [PubMed]
- Saifi C, Laratta JL, Petridis P, Shillingford JN, Lehman RA, Lenke LG. Vertebral column resection for rigid spinal deformity. Global Spine J 2017;7:280-90. [Crossref] [PubMed]



