
Intrathecal morphine injection in anterior lumbar and lateral lumbar spine surgery: technical note
Introduction
Intrathecal morphine (ITM) is routinely used in many surgical specialties as an adjunct to postoperative analgesia (1,2). There have been multiple reports of the benefits of ITM in lumbar spine surgery where it has been shown to significantly reduce the need for intravenous opioid analgesia, improve time to mobilization, and shorten length of hospital stay (3).
Anterior lumbar spine surgery (ALSS) includes anterior lumbar interbody fusion (ALIF) and lumbar total disc replacement (TDR). Lateral lumbar spine surgery (LLSS) includes transpsoas lateral lumbar interbody fusion (LLIF), anteromedial to psoas (AMP), or anterior to the psoas oblique lumbar interbody fusion (OLIF). ALSS and LLSS have become mainstay surgical techniques, broadly indicated for the restoration of structural and biomechanical integrity in a variety of degenerative lumbar pathologies (4,5). In recent times ALSS and LLSS have increased in popularity with potential benefits of efficient access and direct visualization of the anterior column and disc space, shorter operative times and reduced iatrogenic trauma to paraspinal neurovasculature and musculature (5).
The widely known method of administering ITM intraoperatively during Lumbar Spine Surgery is via a posterior approach (6). Although Posterior lumbar spine surgery provides an opportunity for intrathecal injection, a theoretical concern of this is the risk of an iatrogenic cerebrospinal fluid (CSF) leak with dural puncture (7).
Large numbers of standalone anterior spinal surgeries are performed in our institution. The patient is positioned supine with no access during surgery to the posterior spine and therefore we developed a method of administering ITM through the anterior or lateral approach.
Herein we describe a technique for injection into the dural sac via the Anterior and Lateral approaches to the Lumbar Spine. This technique can be performed easily and quickly with standard surgical equipment. Through use of this technique, patients undergoing spine surgery may benefit from ITM with no risk of iatrogenic CSF leak.
Methods
Injection technique
The intrathecal injection is performed following completion of a full discectomy and immediately prior to impaction of the implant. It is at this point that the dural sac is maximally exposed.
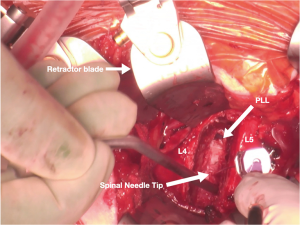
The disc space is thoroughly cleaned and posterior osteophytes removed using a drill and/or Kerrison punch. The posterior longitudinal ligament (PLL) is removed or preserved according to surgeon preference. An Insert and rotate dilator placed on the side of the disc space can assist to further open and place a slight stretch on the dura. A headlight can be used for better illumination. A 26-gauge spinal needle is directed toward the middle of the disc space, pushed through the PLL and the dura. The tip of the needle is held with long non-toothed forceps and the head of the needle with long thin tipped needle holder (Figure 1).
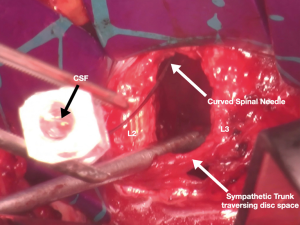
During injection, the syringe is held perpendicular to the surface of the dural sac. The needle is passed into the intrathecal space until CSF can be seen back flowing through the spinal needle (Video 1). In some patients the CSF pressure may be too low to cause backflow through the spinal needle therefore a Valsalva manoeuvre may be used to confirm CSF drainage. Once it is confirmed that the tip of the needle is in the intrathecal space a 2-mL syringe containing 0.2 mg of morphine diluted in saline is connected and administered.
The procedure can be accomplished with the use of equipment readily at hand in the operating theatre and without significantly prolonging operative time.
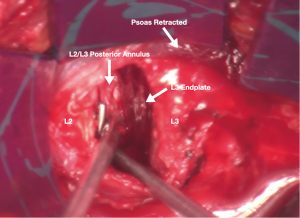
The injection technique during LLSS is more challenging as the dura and PLL are not as easily visualized or as accessible as during the anterior approach (Figure 2). Although technically more difficult than via the ALSS, we clean the posterior disc space all the way to the PLL. The spinal needle is held with forceps and the needle is gently curved and directed towards the middle of the disc space under magnification of loupes. Once visual confirmation is achieved that the tip is in the correct position the same steps of the anterior approach are followed (Figure 3).
Patients scheduled for ALSS or LLSS who received ITM via the anterior or lateral approach were eligible for inclusion.
The study size was predetermined as a planned cohort between August 2018 and November 2019. The injection technique was performed in 21 cases via the anterior approach. Sixteen patients had a single-level fusion (L5/S1 n=15, L3/4 n=1) and five patients had two-level fusions (L4/5 + L5/S1).
In patients who had two-level fusions the morphine was administered at the level of L4/5. Surgical site drains were not used and the patients were followed for between three and twelve months.
More recently we began using the injection technique via the lateral approach and thus far three patients have received ITM this way. All three patients had single-level AMP fusions (L2/3 n=1, L3/4 n=2). The primary outcome is complication rate with the secondary outcome being total narcotic consumption. Outcomes were assessed by an independent assessor with no conflict with regards to the outcomes of this patient group.
Results
In the 24 cases in which the injection technique was performed, there we no instances of postoperative CSF leakage. None of the patients required patient-controlled analgesia (PCA) or any other infusions of morphine. There were no instances of patients developing ileus which we commonly encounter with PCA and no cases of respiratory decline. One patient experienced itching which persisted for 24 hours.
All patients could roll in the bed within 4 hours of surgery with no pain and were mobilised within 12 hours. Visual Analogue Scale (VAS) score was 0 in 10 patients, 1–2 in 10 patients (this group includes all patients who underwent lateral approach) and 3 in 4 patients. The minimum pre-operative VAS score was 7/10 in this group.
Five of the single-level patients were discharged within 48 hours with the other 11 one-level patients going home within 72 hours. All of the remaining two-level patients were discharged within 96 hours with no complications (this group includes patients who underwent lateral approach.
Discussion
In our observational study, ITM was safely and effectively administered via an anterior retroperitoneal or a lateral AMP approach to all patients. Whilst neural injury remains a theoretical risk of this technique, we encountered no instances of any neurological compromise. This was likely due to the excellent visualization and small gauge needle used when performing this technique.
Having also performed ITM through a posterior approach in the past, we are of the opinion that the advantage of an anterior and lateral ITM injection is the negligible possibility of CSF leak or fistula and the already available access during the surgical procedure.
Although we only encountered a single minor complication of transient postoperative itching, the current study is limited by the relatively small patient cohort, and the total number of procedures. The promising results warrant a larger study with multiple operators to confirm the benefits and safety of this technique versus administering ITM via the posterior approach to the spine.
Conclusions
Despite demonstrated safety and efficacy of ITM in lumbar spine surgery, the risk of precipitating a CSF leak remains as a barrier to widespread adoption of this analgesic technique. The technique used in this study facilitates safe injection via excellent direct visualization of the dural sac. This theoretically improves injection technique and therefore is not associated with postoperative CSF leakage.
Acknowledgments
I wish to acknowledge Mr. Aidan McEvoy for his assistance in preparing the manuscript.
Funding: None.
Footnote
Peer Review File: Available at http://dx.doi.org/10.21037/jss-20-610
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss-20-610). The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kong SK, Onsiong SM, Chiu WK, et al. Use of intrathecal morphine for postoperative pain relief after elective laparoscopic colorectal surgery. Anaesthesia 2002;57:1168-73. [Crossref] [PubMed]
- Hu B, Zhou H, Zou X, et al. Comparing the analgesic efficacy of infiltration analgesia vs. intrathecal morphine after total knee arthroplasty. Eur J Anaesthesiol 2020;37:55. [Crossref] [PubMed]
- Dhaliwal P, Yavin D, Whittaker T, et al. Intrathecal Morphine Following Lumbar Fusion: A Randomized, Placebo-Controlled Trial. Neurosurgery 2019;85:189-98. [Crossref] [PubMed]
- Mobbs RJ, Phan K, Assem Y, et al. Combination Ti/PEEK ALIF cage for anterior lumbar interbody fusion: Early clinical and radiological results. J Clin Neurosci 2016;34:94-9. [Crossref] [PubMed]
- Allain J, Dufour T. Anterior lumbar fusion techniques: ALIF, OLIF, DLIF, LLIF, IXLIF. Orthop Traumatol Surg Res 2020;106:S149-57. [Crossref] [PubMed]
- France JC, Jorgenson SS, Lowe TG, et al. The use of intrathecal morphine for analgesia after posterolateral lumbar fusion: a prospective, double-blind, randomized study. Spine (Phila Pa 1976) 1997;22:2272-7. [Crossref] [PubMed]
- Jewett GAE, Yavin D, Dhaliwal P, et al. Oblique Intrathecal Injection in Lumbar Spine Surgery: A Technical Note. Can J Neurol Sci 2017;44:514-7. [Crossref] [PubMed]


