
Subacute hemorrhagic cyst of the ligamentum flavum occurred in the lumbosacral transitional vertebra presenting as progressive lumbar nerve root compression: a case report
IntroductionOther Section
There have been no reports mentioned about relationship between hemorrhagic intravertebral cystic lesion and the lumbosacral transitional vertebrae (LSVT). A causal relationship between the LSTV and lumbar disc herniation was already reported and generally accepted as the microtrauma theory in which hypermobility and mechanical stress are applied between the upper intervertebral discs of the LSTV (1). Pathogenesis of hemorrhagic cysts is less well understood. Microtrauma is suspected to be play a role in lumbar synovial cysts formation and a higher index of suspicion may be warranted in males with active occupations (2). In the LSTV, twisting movements act on the upper part adjacent to the transitional vertebra, might cause microtrauma around the facet joint that leads to the forming a hemorrhagic cyst following damage around the joint capsule. Here we report a rare case of a hemorrhagic intravertebral cystic lesion that occurred in the LSTV of a 42-year-old man and had a subacute course. We present this case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/jss-20-683).
Case presentationOther Section
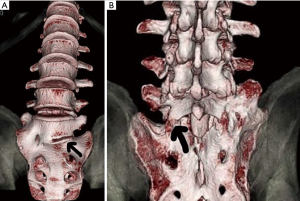
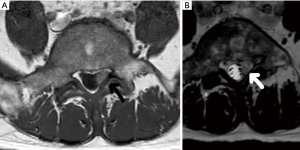
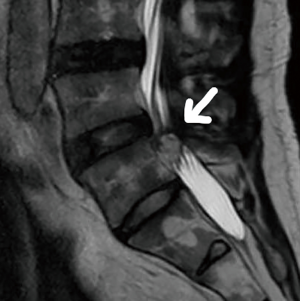
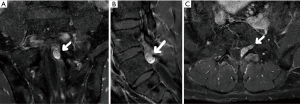
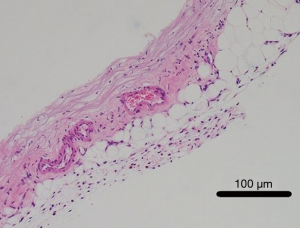
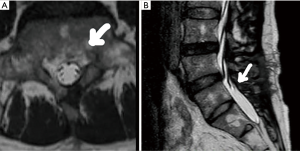
A 42 years old, male with no past medical history presented our outpatient department for the first time with chief complaint of radiating pain from the left buttock to the lateral aspect of the distal part of the left leg that began one week prior to presentation and had gradually increased in severity. He complained of pain at rest that made him unable to work as a farmer, and the gait was pain-avoidance-like gait. The lower limb extension elevation test was positive at 30° on the left lower limb and negative on the right limb. The manual strength test was 5/5 in the tibialis anterior muscle, 5/4 in the extensor hallucis longus muscle, and 5/5 in the gastrocnemius muscle. An X-ray and 3D CT image of the spine revealed ipsilateral lumbarization of the left sacrum (Figure 1A,B). A T1WI MRI showed iso signal intensity at the entrance of the left pedicle root of L6, and T2WI MRI showed a 10 mm nodular lesion with clear boundaries and uniform internal high signal intensity, and the L6 nerve root was compressed from the dorsal side (Figure 2A,B). No degeneration of the L4/5 disc or continuity between the nodule with the lumbar disc was observed (Figure 3). Contrast-enhanced MRI (Gd-T1WI) showed a heterogenous contrast-enhanced effect on the nodule (Figure 4). CT myelography also showed nerve root compression findings similar to those seen on MRI. LSTV was classified as Type IIIA using the Castellvi’s classification (3), and the nodule was found on the ipsilateral of the lumbarization. From the imaging findings, disc cysts, ganglion cysts, synovial cysts, disc sequestration and Schwannomas were differentials of the intravertebral canal cystic lesions; however, it was suspected to be a hemorrhagic cystic lesion because of acute progression of his symptoms and his relatively young age. Due to severity of pain and mild paralysis of the lower limbs, with the informed consent surgical treatment was performed 9 days after his presentation. Following medial facetectomy, resection of the nodule was performed under microscopic surgery. The ligamentum flavum was removed at the level of the pedicle and the subdural venous plexus immediately below was cauterized and removed, and a grayish blue, elastic soft spindle-shaped cyst was seen. The cyst was not continuous with the dural canal and the ventral nerve roots, however attached by fibrous tissue on its cranio-caudal side; therefore, it could not be easily removed by grasping and pulling, and had to be ablated for resection. The cyst was located on the dorsal side of the nerve root; therefore, it was unlikely to be in continuity with the intervertebral disc. During the procedure, slightly viscous dark-red blood flowed out of the cyst when it was compressed with a nerve spatula. Pathological findings showed that the cyst wall consisted of fibrous tissue, with mild lymphocyte infiltration and increased capillary growth, and some hemosiderin deposits by Hematoxylin and Eosin staining (magnification: 10×20). No lining cells, synovium, and nucleus pulposus tissue were found (Figure 5), and the nodule was diagnosed as intracystic hemorrhage of a ganglion in the ligamentum flavum. His symptoms improved shortly after the procedure and he was discharged 5 days after the surgery. The Japanese Orthopaedic Association Back Pain Evaluation Questionnaire (JOABPEQ) evaluated at his outpatient visit 6 months after the operation and pre-surgery were as 100, 75, 100, 100, 69 and 0, 0, 0, 0, 12 in terms of Low back pain, Lumbar function, Walking ability, Social life function and Mental health respectively. And there were no features suggestive of recurrence of the cystic lesion in the follow-up MRI (Figure 6). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
DiscussionOther Section
Cystic lesions that occur in the spinal canal and can lead to neurological symptoms include disc cysts (4), ganglion cysts (5), synovial cysts (6), disc sequestration (7) and Schwannomas (8-10). The clinical features of this patient were as a result of left 6th lumbar nerve root compression due to bleeding into the cystic lesion on the posterior peridural membrane. The reasons are, the pain increased over time, has a subacute course, the cyst contained dark red viscous fluid intraoperatively, contrast-enhanced MRI findings revealed contrast effect even inside the cyst, and there were a few pathological depositions of hemosiderin. In this case, lumbar disc cysts were unlikely diagnosis because the cyst was seen just below the ligamentum flavum and the epidural plexus, and there were no features suggestive of a disc herniation on imaging or pathological evaluations. Facet joint cysts are rare with prevalence between 0.6% and 7.3% (11). They usually present in the sixth decade (12). Non-hemorrhagic synovial cysts are reported to be related to degenerative spinal changes and segmental instability (13,14). Other study about relationship between facet joint cysts and MRI have also reported that cysts to have significant associations with facet arthropathy, facet joint osteoarthritis and spondylolisthesis (15). On MRI, non-hemorrhagic synovial cysts are typically T1-hypointense and T2-hyperintense, but the signal varies depending on factors including protein content, blood products, and timing of hemorrhage within the cyst (12). T2 imaging of cysts is known to have varying signal intensity, and previous reports have similarly surmised previous old hemorrhages, elevated protein content, and calcification can all be causes of this varying signal (16). Pathologically, facet joint cysts are composed of cuboid or pseudocolumnar epithelium and clear or straw-colored fluid. They can be classified as either synovial of ganglionic histologically (17). Cysts can be found to have hemorrhaged and this can lead to acute neural compression with an incidence of 9.3% (12). Our case has no evidence of continuity between the cyst and the facet joints on imaging and macroscopic finding; furthermore, pathological findings did not show a synovial cell layer on the inner surface of the wall of the cyst. It is reported that some sequestered disc fragments still can be misdiagnosed as other more common epidural neoplasms because they appear hypointense on T1WI, hyperintense on T2WI and they present with ring-like peripheral Gd enhancement images (7). Although the ring-like peripheral enhancement is helpful for differentiating between disc fragments that mimic a tumor and metastatic tumors, hematomas, and meningioma, it can also be observed in Schwannomas (7). Schwannomas are uniformly distributed throughout the spine and topographically, they may be intradural-extramedullary (72%), intra and extradural (13%), completely extradural (13%), or, exceptionally, intramedullary (1%) (8-10). Internal heterogeneous signal on T2WI MRI was confusing because it had a target sign usually seen in schwannomas, however, this finding is suspected to indicate that the cyst was composed of a mixture of old and new hematomas.
The most plausible explanation for our diagnosis for this case was that the cyst was formed by intracystic hemorrhage of a ganglion in the ligamentum flavum which lead to a change in viscosity within the cyst (18). However, it is difficult to distinguish between synovial cyst and ganglion cyst, and they are collectively called juxta-facet cysts (JFC) (19). The microtrauma theory is generally accepted as the cause of this, and it is based on the fact that JFC occurs frequently in the elderly and often occurs with osteoarthritis changes in the facet joints (19). Similarly, microtrauma is also suspected to be play a role in lumbar synovial cysts formation and a higher index of suspicion may be warranted in males with active occupations (2).
LSTV are found in 3.3–12.3% (3,20) of the general population and are not uncommon. We consider that LSTV relates to the formation of a hemorrhagic cyst in this case. There are no reports on LSTV and intravertebral cystic lesions, but a study by Castellvi et al., discussed the association between LSTV and lumbar disc herniation in 30% of 200 lumbar disc herniations and 2.5% of cases were classified as type III (3). In addition, in a report on the site of facet joint degeneration that compared LSTV and non-LSTV, the rate of degeneration in the upper transitional vertebra at the same level were 60.4% and 42.8%, respectively, and this difference was statistically significant (21). It has been argued that hypermobility and instrumental stress are applied between the upper intervertebral discs of the LSTV (1). The literature review of 44 cases found that cyst hemorrhage more often occurs in men and at an earlier age, lending support to a micro-trauma hypothesis if occupation and lifestyle is considered (12).
We report a rare case of a hemorrhagic intravertebral cystic lesion that occurred in the LSTV of a 42-year-old man and had a subacute course. In this LSTV with a type IIIA degeneration the patient also had cyst formation on the non-osseous fusion side; therefore, it can be presumed that the burden on the facet joint area also increased. It was speculated that in the LSTV, twisting movements act on the upper part adjacent to the transitional vertebra, causing microtrauma around the soft tissues of facet joint that leads to the forming a hemorrhagic cyst. It is difficult to make a diagnosis of hemorrhagic cyst from imaging alone. It must be suspected from the aspect of age (relatively young), gender (male), clinical course (acute to subacute) and MR imaging (various signal intensity patterns on T2WI and contrast effect on Gd enhancement).
AcknowledgmentsOther Section
Funding: None.
FootnoteOther Section
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/jss-20-683
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss-20-683). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
ReferencesOther Section
- Elster AD. Bertolotti's syndrome revisited. Transitional vertebrae of the lumbar spine. Spine (Phila Pa 1976) 1989;14:1373-7. [Crossref] [PubMed]
- Cannarsa G, Clark SW, Chalouhi N, et al. Hemorrhagic lumbar synovial cyst: case report and literature review. Nagoya J Med Sci 2015;77:481-92. [PubMed]
- Castellvi AE, Goldstein LA, Chan DP. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine (Phila Pa 1976) 1984;9:493-5. [Crossref] [PubMed]
- Chiba K, Toyama Y, Matsumoto M, et al. Intraspinal cyst communicating with the intervertebral disc in the lumbar spine: discal cyst. Spine (Phila Pa 1976) 2001;26:2112-8. [Crossref] [PubMed]
- Arantes M, Silva RS, Romão H, et al. Spontaneous hemorrhage in a lumbar ganglion cyst. Spine (Phila Pa 1976) 2008;33:E521-4. [Crossref] [PubMed]
- Brish A, Payan HM. Lumbar intraspinal extradural ganglion cyst. J Neurol Neurosurg Psychiatry 1972;35:771-5. [Crossref] [PubMed]
- Emamian SA, Skriver EB, Henriksen L, et al. Lumbar herniated disk mimicking neurinoma. Case report. Acta Radiol 1993;34:127-9. [Crossref] [PubMed]
- Jinnai T, Koyama T. Clinical characteristics of spinal nerve sheath tumors: analysis of 149 cases. Neurosurgery 2005;56:510-5. [Crossref] [PubMed]
- Greenberg MS. Spinal schwannomas. In: Handbook of Neurosurgery. Thieme, 2010:734-6.
- Celli P, Trillò G, Ferrante L. Spinal extradural schwannoma. J Neurosurg Spine 2005;2:447-56. [Crossref] [PubMed]
- Eyster EF, Scott WR. Lumbar synovial cysts: report of eleven cases. Neurosurgery 1989;24:112-5. [Crossref] [PubMed]
- Lyons MK, Atkinson JL, Wharen RE, et al. Surgical evaluation and management of lumbar synovial cysts: the Mayo Clinic experience. J Neurosurg 2000;93:53-7. [PubMed]
- Boviatsis EJ, Stavrinou LC, Kouyialis AT, et al. Spinal synovial cysts: pathogenesis, diagnosis and surgical treatment in a series of seven cases and literature review. Eur Spine J 2008;17:831-7. [Crossref] [PubMed]
- Kjerulf TD, Terry DW Jr, Boubelik RJ. Lumbar synovial or ganglion cysts. Neurosurgery 1986;19:415-20. [Crossref] [PubMed]
- Doyle AJ, Merrilees M. Synovial cysts of the lumbar facet joints in a symptomatic population: prevalence on magnetic resonance imaging. Spine (Phila Pa 1976) 2004;29:874-8. [Crossref] [PubMed]
- Apostolaki E, Davies AM, Evans N, et al. MR imaging of lumbar facet joint synovial cysts. Eur Radiol 2000;10:615-23. [Crossref] [PubMed]
- Sabo RA, Tracy PT, Weinger JM. A series of 60 juxtafacet cysts: clinical presentation, the role of spinal instability, and treatment. J Neurosurg 1996;85:560-5. [Crossref] [PubMed]
- Finkelstein SD, Sayegh R, Watson P, et al. Juxta-facet cysts. Report of two cases and review of clinicopathologic features. Spine (Phila Pa 1976) 1993;18:779-82. [Crossref] [PubMed]
- Kao CC, Winkler SS, Turner JH. Synovial cyst of spinal facet. Case report. J Neurosurg. 1974;41:372-6. [Crossref] [PubMed]
- Bron JL, van Royen BJ, Wuisman PI. The clinical significance of lumbosacral transitional anomalies. Acta Orthop Belg 2007;73:687-95. [PubMed]
- Vergauwen S, Parizel PM, van Breusegem L, et al. Distribution and incidence of degenerative spine changes in patients with a lumbo-sacral transitional vertebra. Eur Spine J 1997;6:168-72. [Crossref] [PubMed]



