
Minimally invasive sacroiliac joint fusion using a novel hydroxyapatite-coated screw: final 2-year clinical and radiographic results
Introduction
Sacroiliac joint (SIJ) pain has been increasingly diagnosed and is commonly identified as a source of low back pain documented in 14–22% of patients in a spine clinic (1,2). The hyaline cartilage, fibrocartilage, and synovium, which comprise the complex syndesmotic SIJ, are prone to degeneration leading to dysfunction. Forces from the lumbar spine to the pelvis are transmitted through the SIJ and can cause this degeneration over time (3-5). A dysfunctional SIJ can lead to symptoms including low back pain that radiates to the ipsilateral thighs, buttock, groin, and legs, as well as pain in the lumbar spine to the lower extremities (6).
Initial conservative treatment has typically consisted of physical therapy, manual therapy, or the use of steroid injections, bracing, and opioid pain relievers (5). A study found that these treatments may be effective in only 12.5% of patients and for some in the short term, but many patients will require a more permanent solution (7).
Utilization of minimally invasive SIJ fusion has been increasing to about 87% in 2012 compared to that of open procedures (8). SIJ fusion has been developed to stabilize the joint by using hydroxyapatite (HA)-coated transiliac screws. HA-coated screws are designed to be implanted across a dysfunctional SIJ to create stability, and promote bone growth through the screw slot, and along the surface of the screw for lasting fixation. The current study describes the use of this HA-coated screw design in patients over 2-year follow-up. Mid-term clinical outcome studies are needed to determine the effectiveness of this procedure in relieving the pain caused by SIJ dysfunction.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jss-20-627).
Methods
This study is a 24-month follow-up on a previously published 12-month follow-up report by Rappoport et al. (9). Institutional Review Board approval was secured prior to enrollment. Patients diagnosed with SIJ dysfunction who had failed conservative treatment were consented. Diagnosis of SIJ dysfunction was determined through provocative physical examination, supported by medical history, by excluding other potential causes of pain through lumbar magnetic resonance imaging, and finally diagnostic injection to the SIJ to confirm SIJ dysfunction. Exclusionary criteria included a history of osteopenia or osteomalacia, metabolic bone disease, any condition that totally precludes the possibility of bone fusion, or use of medications that may interfere with bone/soft tissue healing.
Surgical technique
The surgical technique utilized in this study was previously described in the initial report by Rappoport et al. (9). Fluoroscopically guided intra-articular injections were used to diagnose the patients. The SIJ fusion implant utilized in this study (SI-LOK, Globus Medical, Inc., Audubon, Pennsylvania, USA) was a novel HA-coated slotted screw designed specifically for a lateral approach MIS fusion of the SIJ. The slot allows for bone through-growth resulting in biological fixation of the screw. The HA coating of the screw is designed to promote osseous apposition to the implant. The washer design of the screw assists the surgeon in optimizing proper screw insertion depth.
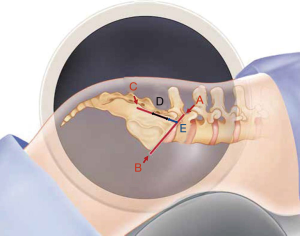
Following prone positioning on a Jackson table, scout inlet, outlet and lateral C-arm images are obtained. The skin is marked (Figure 1) at the confluence (A) of the alar lines (B) and the posterior cortex of the sacrum (C) on the lateral image. An approximate 2–3 cm incision (D) is made 1 cm distal (E) to the intersection of these 2 lines. Blunt finger dissection is performed down to the fascia. The first guide pin is initially inserted using the lateral projection, beginning in the region of the posterior sacrum, staying caudal to the alar line and angled approximately 10–15 degrees downward. Pin projection is checked in the inlet and outlet views as well, with the outlet view used to determine screw length. Drilling is performed across the joint over the guide pin and the screw slot is filled with bone from the drill reaming.
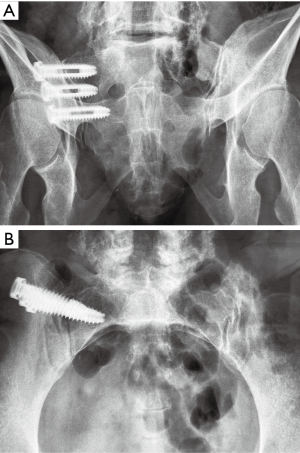
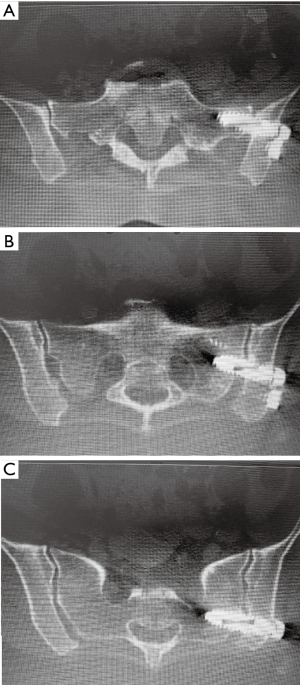
The screw is then inserted across the joint into proper position on the outlet view. The washer can be seen to tilt when the lateral cortex is engaged. The inlet view is then used to check the screw position, and the second pin is placed using the dual parallel pin guide. Switching to the lateral view, the first screw position is confirmed, as well as the position of the second pin. On the working outlet view, the guide pin is advanced staying lateral to the S1 foramen. Screw length is determined, and the screw is packed and inserted in the same fashion. The third screw is placed using the same technique. Once all 3 screws have been placed, final position is determined with outlet (Figure 2A), inlet (Figure 2B) and lateral views. If intra-operative CT scan is available, further precise confirmation of screw position can be determined (Figure 3). All patients had 3 screws placed in this study.
Outcome measures
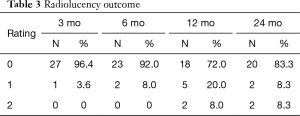
Patient demographic data were captured. Intraoperative data were recorded including operative time, estimated blood loss, fluoroscopic exposure time, and duration of hospital stay. Patient reported outcomes visual analog scale (VAS) back and leg pain, Oswestry Disability Index (ODI) and a satisfaction and work status survey were collected preoperatively and at each follow-up. Surgeon reported outcomes Odom’s criteria, and radiographic determinations were recorded at each follow-up. Mechanical stability of the SIJ was defined as absence of screw loosening and radiolucent gaps at the bone-screw interface, screw migration, and improvement in patient symptoms by 12 months postoperatively. Radiolucency was assessed using the criteria in Table 1, and these scores were used to inform decisions on mechanical stability.

Full table
Statistical analysis
Statistical analysis was carried out using SPSS version 20.0.0 software for Windows (IBM Corp., Armonk, NY, USA). Descriptive statistics, frequency tables, and measures of central tendencies were calculated. Mean changes were assessed using Wilcoxon signed ranks tests for related samples, with a P value <0.05 considered significant.
Ethical statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Western Institutional Review Board (IRB00000533) and informed consent was taken from all the patients.
Results
Data on 32 patients were prospectively collected between June 2013 and July 2018. Mean patient age was 55.2 (±10.7) years, and 62.5% were female. Of the initial 32 patients included in the previous 12-month follow-up report (9), four patients were could not be contacted to return for 24-month follow-up. Mean operative time was 42.6±20.4 minutes. Mean fluoroscopic time was 2.9±1.3 minutes. Estimated blood loss did not exceed 50 mL (mean, 12.5±10.5 mL) in all cases. Overnight hospital stay was required for 84% of patients, and the remaining patients required a 2-day stay (16%).
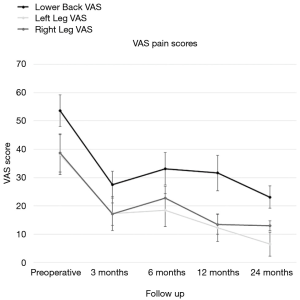
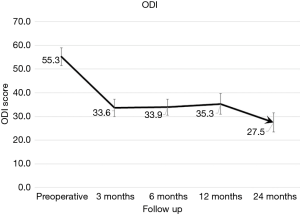
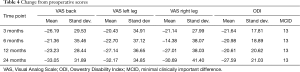
Low back pain VAS (Figure 4) scores were significantly reduced from preoperative scores to 24-month follow-up at a mean of 54.8 (±26.2) compared to 20.0 (±18.4), respectively (Table 2). Similarly, left leg VAS scores were reduced from preoperative (37.7±31.7) to 24-month follow-up (5.8±8.1), as right leg VAS scores were reduced from 39.8 (±33.2) to 11.5 (±20.1) at 24-month follow-up. All reductions were found to be statistically significant (P<0.05). VAS pain scores for back, left and right legs did not significantly (P=0.658, P=0.904, P=0.702 respectively) change between 12-month and 24-month follow-up. There was no significant difference (P=0.159) between left and right leg VAS pain scores at 24-month follow up. All average decreases are located in Table 3. ODI scores were significantly reduced through 24-month follow-up. Mean preoperative ODI scores (Figure 5) were 55.6 (±17.5), and were reduced to a mean of 27.5 (±18.8). The 6.4-point difference between 12 and 24-month average ODI was significant (P=0.030).
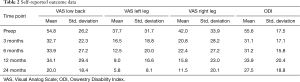
Full table
Full table
Patient satisfaction was rated on a 0 to 10 scale and was completed at each follow-up. At 24-month follow-up, mean satisfaction was 9.0 (±1.6), supporting a high level of satisfaction. One-hundred percent of patients answered that they would recommend the surgery and would have the surgery again.
Surgeon assessment determined that no patient was considered to have poor outcomes by Odom’s criteria. Further, 80.8% of patients were assessed to have either good or excellent outcomes, with 5 of 26 patients considered to have fair outcomes. Radiolucency scores are located in Table 3. There were no severe cases of radiolucency at any time point. Of the 24 patients assessed at 24 months, 22 (91.7%) had mild or no evidence of radiolucency. At 12-month follow-up, 2 patients showed moderate signs of radiolucency, and the same number had moderate signs at 24-months. At 24-month follow-up, mechanical stability was maintained for all patients assessed as stable at 12 months. The two patients who were considered not mechanically stable at 12-month follow-up underwent revision surgery post 12-month follow-up. One patient achieved stability after revision and the other was lost to follow-up.
Discussion
The high prevalence of low back pain in an aging population demands an effective response by physicians (10). Conservative treatment, most specifically long-term opioid use, can result in a number of complications without effectively addressing the root cause of the problem (11). When conservative treatment fails to relieve low back pain caused by SIJ dysfunction, a surgical solution could potentially provide long-term pain relief and improvement in quality of life (12).
The current study provides clinical evidence that the use of HA-coated screws to stabilize the SIJ significantly reduces VAS pain scores from preoperative scores. Furthermore, VAS pain scores continued to decrease on average at each time point. This improvement in VAS pain and ODI scores (Table 4) is substantially greater than the minimally clinical important difference (13-15). ODI scores significantly decreased between 12- and 24-month follow-up. This may be related to further body conditioning and exercise improvement over time; however, this can only be taken as speculative as there is no way to confirm through the data.
Full table
Similar results were reported in a randomized control study of SIJ fusion using triangular dowels with a 26.7 mean pain score at 24-month follow-up (16). Furthermore, in a 24-month follow-up analysis of patients treated with a different screw system for SIJ dysfunction, the reported mean VAS pain score was 44.8 (converted to a 100-point scale) at a final follow-up of 36 months on average (17). Comparable results were also reported in a 2016 study (18) of a dowel implant that reduced pain scores to 26.0 at 24-month follow-up. In the same study, ODI was decreased to 30.9 at 24 months. The current study of an HA-coated slotted screw system for SIJ fusion showed comparative VAS pain scores of 20.0, and an ODI score of 27.5 at 24 months.
Limitations of this study include the single cohort design, the small number of patients, and the loss of a number of patients to follow-up between 1 and 2 years. However, the data were prospectively collected, and patients were consecutively enrolled. Although there were no comparators, there are historical controls in the literature and outcomes similar to the cited studies that provide clinical evidence of the utility of SIJ screws in reducing low back pain and improving functional outcomes.
Conclusions
Clinical outcomes studies are essential in providing evidence of the effectiveness of sacroiliac screws to stabilize the joint in cases of SIJ dysfunction. This study shows positive clinical and functional outcomes for patients who have undergone fusion using HA-coated screws for SIJ dysfunction that are comparable to the literature.
Acknowledgments
Funding: Funding for this study was provided by Globus Medical, Inc., for which LHR is a paid consultant and receives research support, KH receives research support, and TS is a salaried employee.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jss-20-627
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jss-20-627
Peer Review File: Available at http://dx.doi.org/10.21037/jss-20-627
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss-20-627). Dr. LHR reports personal fees from Globus Medical, Inc., during the conduct of the study; personal fees from 4Web, personal fees from Orthofix, Inc., personal fees from Globus Medical, Inc., personal fees from Titan Spine, personal fees from Medtronic, outside the submitted work; Ms. KH reports personal fees from Globus Medical, Inc., during the conduct of the study; Mr. TS reports personal fees from Globus Medical, Inc., during the conduct of the study.
Ethical Statement: The authors are accountable for all aspects of the work (including full data access, integrity of the data and the accuracy of the data analysis) in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Western Institutional Review Board (IRB00000533) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ackerman SJ, Polly DW Jr, Knight T, et al. Nonoperative care to manage sacroiliac joint disruption and degenerative sacroiliitis: high costs and medical resource utilization in the United States Medicare population. J Neurosurg Spine 2014;20:354-63. [Crossref] [PubMed]
- Ackerman SJ, Polly DW Jr, Knight T, et al. Management of sacroiliac joint disruption and degenerative sacroiliitis with nonoperative care is medical resource-intensive and costly in a United States commercial payer population. Clinicoecon Outcomes Res 2014;6:63-74. [Crossref] [PubMed]
- Buchowski JM, Kebaish KM, Sinkov V, et al. Functional and radiographic outcome of sacroiliac arthrodesis for the disorders of the sacroiliac joint. Spine J 2005;5:520-8; discussion 529. [Crossref] [PubMed]
- Katz V, Schofferman J, Reynolds J. The sacroiliac joint: a potential cause of pain after lumbar fusion to the sacrum. J Spinal Disord Tech 2003;16:96-9. [Crossref] [PubMed]
- Slipman CW, Shin CH, Patel RK, et al. Etiologies of failed back surgery syndrome. Pain Med 2002;3:200-14; discussion 214-7. [Crossref] [PubMed]
- Cohen SP. Sacroiliac joint pain: a comprehensive review of anatomy, diagnosis, and treatment. Anesth Analg 2005;101:1440-53. [Crossref] [PubMed]
- Polly DW, Cher DJ, Wine KD, et al. Randomized Controlled Trial of Minimally Invasive Sacroiliac Joint Fusion Using Triangular Titanium Implants vs Nonsurgical Management for Sacroiliac Joint Dysfunction: 12-Month Outcomes. Neurosurgery 2015;77:674-90; discussion 690-1. [Crossref] [PubMed]
- Lorio MP, Polly DW Jr, Ninkovic I, et al. Utilization of Minimally Invasive Surgical Approach for Sacroiliac Joint Fusion in Surgeon Population of ISASS and SMISS Membership. Open Orthop J 2014;8:1-6. [Crossref] [PubMed]
- Rappoport LH, Luna IY, Joshua G. Minimally Invasive Sacroiliac Joint Fusion Using a Novel Hydroxyapatite-Coated Screw: Preliminary 1-Year Clinical and Radiographic Results of a 2-Year Prospective Study. World Neurosurg 2017;101:493-7. [Crossref] [PubMed]
- Hoy D, Bain C, Williams G, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum 2012;64:2028-37. [Crossref] [PubMed]
- Polly DW, Cher D. Ignoring the sacroiliac joint in chronic low back pain is costly. Clinicoecon Outcomes Res 2016;8:23-31. Erratum in: Clinicoecon Outcomes Res 2016 Jul 8;8:349. doi: 10.2147/CEOR.S107802. eCollection 2016. [PubMed]
- Araghi A, Woodruff R, Colle K, et al. Pain and Opioid use Outcomes Following Minimally Invasive Sacroiliac Joint Fusion with Decortication and Bone Grafting: The Evolusion Clinical Trial. Open Orthop J 2017;11:1440-8. [Crossref] [PubMed]
- Carreon LY, Bratcher KR, Canan CE, et al. Differentiating minimum clinically important difference for primary and revision lumbar fusion surgeries. J Neurosurg Spine 2013;18:102-6. [Crossref] [PubMed]
- Copay AG, Cher DJ. Is the Oswestry Disability Index a valid measure of response to sacroiliac joint treatment? Qual Life Res 2016;25:283-92. [Crossref] [PubMed]
- Myles PS, Myles DB, Galagher W, et al. Measuring acute postoperative pain using the visual analog scale: the minimal clinically important difference and patient acceptable symptom state. Br J Anaesth 2017;118:424-9. [Crossref] [PubMed]
- Polly DW, Swofford J, Whang PG, et al. Two-Year Outcomes from a Randomized Controlled Trial of Minimally Invasive Sacroiliac Joint Fusion vs. Non-Surgical Management for Sacroiliac Joint Dysfunction. Int J Spine Surg 2016;10:28. [Crossref] [PubMed]
- Mason LW, Chopra I, Mohanty K. The percutaneous stabilisation of the sacroiliac joint with hollow modular anchorage screws: a prospective outcome study. Eur Spine J 2013;22:2325-31. [Crossref] [PubMed]
- Duhon BS, Bitan F, Lockstadt H, et al. Triangular Titanium Implants for Minimally Invasive Sacroiliac Joint Fusion: 2-Year Follow-Up from a Prospective Multicenter Trial. Int J Spine Surg 2016;10:13. [Crossref] [PubMed]


