
Seizures following cervical laminectomy and lateral mass fusion: case report and review of the literature
Introduction
Spine surgery can result in several complications, including vascular injury, nerve root injury, postoperative epidural hematoma formation, wound infections, spinal cord injury and dural tear (1-3). Incidental durotomy with cerebrospinal fluid (CSF) loss also has been reported after lumbar puncture, spinal anesthesia, myelography, and lumbar drain insertion (4-9). Different treatment options are available to treat durotomies that involve direct intraoperative primary closure, including the use of fibrin glue, fat or muscle grafts (10). Durotomy with a cerebrospinal fluid (CSF) leak can rarely lead to intracranial hemorrhage in the form of subdural hematoma, epidural hematoma, cerebellar hemorrhage, subarachnoid hemorrhage, and supratentorial intraparenchymal hemorrhage (11,12). The exact pathophysiology of this type of bleeding is unknown, but it is assumed that a CSF leak can cause a decrease in intracranial pressure and expansion of subdural spaces that may led to downward displacement of the brain, with stretching and a subsequent tearing of bridging veins hence, SDH formation (13,14). Cerebellar bleeding similarly occurs due to downward displacement of the cerebellum and tearing of cerebellar veins (15,16). We present a unique case of intracranial hemorrhage following an incidental dural tear during posterior cervical spinal surgery.
We present the following case in accordance with the CARE reporting checklist (available at https://dx.doi.org/10.21037/jss-20-642).
Case presentation
A 72-year-old, right-handed male presented with neck pain, numbness and weakness of both hands (greater on the right side) along with walking difficulties. His past medical history was only remarkable for gastroesophageal reflux disease. No history of hypertension or coagulation disorders were documented, and family history was not contributory. He was retired and smoked 1–2 packs of cigarettes per day, in addition to significant alcohol use every day. He was not on any anticoagulant medications.
His neurological exam revealed the mild weakness of intrinsic hand muscles with power +4/5 bilaterally and the right hip flexion weakness with the power of 4/5. Myelopathic signs included the presence of bilateral Hoffman signs and hyperreflexia in all four limbs.
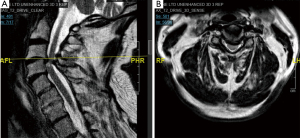
Pre-operative magnetic resonance imaging (MRI) cervical spine scan showed significant stenosis at the level of C3–C5 with spinal cord myelomalacia (Figure 1).Laboratory blood tests were all within normal limits, including platelet count, prothrombin time, and activated partial thromboplastin time.
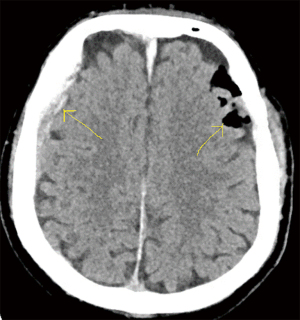
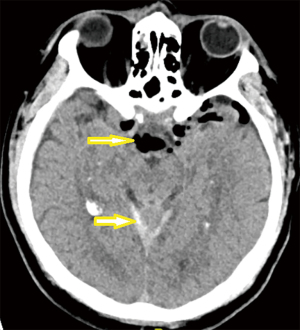
He underwent a posterior cervical decompression with instrumentation and fusion from C3–C5 (Figure 2). The patient was placed in a slight reverse Trendelenburg prone position with the head being above the horizontal plane approximately 10 degrees. During the surgery, a dural tear occurred when decompressing the lamina of C5, which resulted in a sudden gush of CSF on the right-side. The CSF leak was managed by immediately applying cottonoids followed by a 5-0 prolene primary closure. 0.5 mL of fibrin glue was applied over the repair area prior to closure. The dural tear repair was tested under direct visualization with an applied Valsalva maneuver at 40 mmHg, and no residual leak was observed at that time. The surgery was completed, and the patient was extubated and brought to the recovery unit. After a few minutes in the recovery room, the patient developed two generalized tonic-clonic seizures that lasted for 15 seconds. As a result, he was intubated and transferred to the Intensive Care Unit. An urgent computerized tomography (CT) scan of the head was ordered. It showed pneumocephalus intracranially in the subarachnoid space of the left Sylvian fissure and basal cisterns, along with an acute subdural hematoma of the midline falx, bilateral tentorial leaflets, right frontoparietal region, and subarachnoid hemorrhage (SAH) in the foli of the cerebellum. Local mass effect from the right frontoparietal area was present without midline shift (Figures 3,4). Different aetiologies of subarachnoid hemorrhage were considered like ruptured aneurysms or an arteriovenous malformation, however the bleeding pattern in multiple locations was not consistent with these causes of spontaneous hemorrhages; based on this, we did not obtain a CT angiogram (CTA).

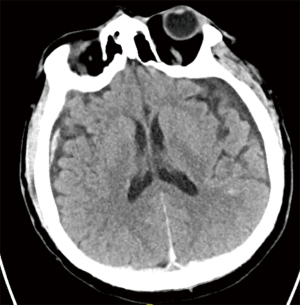
The patient seizures initially were managed with sedation (Midazolam) and antiepileptics (Phenytoin) in the recovery room. The patient switched over to Levetiracetam in the intensive care unit. After a few days, he was extubated and transferred to the ward. His wound healed very well, without signs of infections, swelling, or CSF leaking from the skin. A Follow-up CT brain scan on a postoperative day five demonstrated resolution of the pneumocephalus and decreased size of the subdural hematomas (Figure 5).
He had a full recovery, and he was discharged without further incidents on postoperative day 19. He underwent physiotherapy at an outpatient rehabilitation center following hospital discharge. Three months after discharge, the patient was assessed in the clinic. He reported no further seizures, and his neurological examination showed improvement of his bilateral hand weakness and gait compared to his pre-operative status. No new neurological deficits were noted. All procedures performed in studies involving human participant were in accordance with the ethical standards of the institutional and national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient, to allow presentation of his case.
Discussion
Dural injuries are a relatively infrequent complication of spine surgery, with an incidence of 4% to 9% (17,18). Multiple etiologies of a CSF leak due to dural tear during surgeries were reported, including direct trauma, excessive nerve root traction, and misplaced instrumentation (19,20). The risk factors that can precipitate this complication include older age, female sex, a previous surgery with scar formation, corrective vertebral osteotomy (CVO), degenerative spondylolisthesis, and radiotherapy that can impair tissue healing (13,21-26). Dural openings are also a part of spinal operations—for example, intradural tumour or lesion.
Acute intraoperative CSF leak after dural tear can rarely lead to the formation of intracranial hematomas. We searched the literature and found 55 cases of intracranial hematomas, including epidural, subdural, SAH, cerebral and cerebellar hematomas following incidental CSF leak during spine surgery (Table 1). In most cases, patients present with a persistent headache due to caudal movement of the brain that creates tension on the pain-sensitive dural sinuses (30). In addition to mental status changes, nausea, and vomiting (31).In our case, the patient did not present with any of the milder preceding symptoms. Instead, he presented with a new-onset sudden generalized tonic-clonic seizure that occurred immediately after the surgery.
Table 1
| Author | Age/sex | Procedure | Intracranial complications | Outcomes |
|---|---|---|---|---|
| Chadduck WM (1981) ( |
59M | C3-7 Cervical laminectomy | CBH | Leg’s spasticity |
| Mikawa Y |
75M | Redo C1-C2 fusion | CBH + SAH | Died (pneumonia) |
| Andrews RT |
36M | Lumbar scoliosis instrumentation | CBH + HCP | Quadriparesis (decline) |
| Burkhard PR |
71M | Right L5/S1 Laminectomy & discectomy | SDH | Baseline |
| Lu CH |
59F | Redo L5/S1 decompression, instrumentation & fusion | SDH | Baseline |
| Friedman JA |
43M | T9/10 transpedicular discectomy | CBH | Slight residual dysarthria & gait ataxia |
| Friedman JA |
56F | L3/S1 decompression, instrumentation & fusion | CBH | Residual mild dysarthria & ataxia |
| Hentschel SJ |
58F | T5 extradural breast cancer resection & reconstruction | SDH & Pn | Baseline |
| Kuhn J |
46M | Redo L5/S1discectomy | SDH | Residual H/A & concentration problem |
| Sciubba DM |
55F | Redo L3 corpectomy, Instrumentation & fusion | SDH | Baseline |
| Karaeminogullari O |
73F | L3-5 laminectomy + L2-L5 Instrumentation & fusion | CBH + HCP | Mild ataxia |
| Farag E |
43F | L4-S1fusion & reexploration of dural defect | CBH | Diplopia far lateral gaze |
| Konya D |
48F | L3-5 laminectomy & fixation L4/5 discectomy | CBH | Baseline |
| Ozturk E |
23F | thoracolumbar scoliosis Instrumentation & fusion | CBH + TH + Putamen hemorrhage + Pn | Baseline |
| Chalela JA |
62F | L3-5 Laminectomy &fusion | CBH & HCP | Baseline |
| Zimmerman RM |
77M | T11 to S1 instrumentation &fusion | CBH + IVH | Major cognitive deficit. Died 9 months later (pneumonia) |
| Zimmerman RM |
55F | Revision L2 to L4 decompression, instrumentation &fusion | SDH | Baseline |
| Zimmerman RM |
63M | L2 to L5 decompression, instrumentation &fusion | CB SAH | Baseline |
| Zimmerman RM |
64F | L1-sacrum decompression, instrumentation | CBH + HCP | Died (CBH + HCP) |
| Calisaneller T |
67F | L4/S1 decompression & instrumentation | CBH | Baseline |
| Hashidate H |
85F | T5-7 extradural tumor resection | CBH | Near baseline |
| Beier AD |
39F | Right L5/S1 microdiscectomy | Right FP SDH | Baseline |
| Cevik B |
79F | L4-5 decompression | CBH + Pn | Baseline |
| Cevik B |
68F | L4-S1 decompression & instrumentation | CBH | Baseline |
| Ulivieri S |
53F | L4-5 microdiscectomy | CBH | Baseline |
| Nam TK |
61M | L3-5 decompression & discectomy | CBH + IVH + Pn | Mild cerebellar signs |
| Jung YY |
58M | L1-2 discectomy, decompression, instrumentation & fusion | Bilateral FP SDH | Baseline |
| Gul S |
64F | Redo L3-5 decompression, discectomies, & instrumentation | CBH + HCP | Gait ataxia, left foot drop, Bilateral diplopia on far lateral gaze |
| Nowak R |
12F | Thoracic instrumentation | Bifrontal SDH + Pn | Baseline |
| Fernandez-Jara J |
58F | L5/S1 decompression & instrumentation | CBH + CB SAH | Baseline |
| Hempelmann RG |
61F | T1-4 decompression for tumor | CBH | uneventful |
| Hempelmann RG |
69F | L3-4 decompression, instrumentation & fusion | CBH + TOH | Baseline |
| Hempelmann RG |
62F | L2-4 decompression, instrumentation & fusion | CBH + POH | Baseline |
| You SH |
63M | L5-S1 discectomy Redo L3-5 laminectomies &instrumentation | CBH + TH | Baseline |
| Lee HY |
63F | Redo L3-4 fusion | CBH | Baseline |
| Khalatbari MR |
53M | L4-5 discectomy | CBH + HCP | Baseline |
| Khalatbari MR |
75M | L1-5 laminectomy | CBH + HCP | Died (pulmonary complications) |
| Khalatbari MR |
34F | L4-5 discectomy | FP SDH | Baseline |
| Khalatbari MR |
29M | L4-5 discectomy | P EDH | Baseline |
| Utku U |
57M | T12-L5 laminectomy & instrumentation | FT SDH | Baseline |
| CavanillesWalker JM |
65F | L2-5 laminectomy, instrumentation & fusion | CBI + HCP | Dysmetria hands/fingers & transient vertigo |
| Choi BW |
57F | L4-5 laminectomy, instrumentation & fusion | CBH | Baseline |
| Kaloostian PE |
45M | Anterior & posterior cervical decompression, instrumentation & fusion | CBH | Baseline |
| Kaloostian PE |
55M | Redo lumbar posterior decompression, instrumentation | TP SDH | Baseline |
| Kaloostian PE |
61F | T6–7 transpedicular corpectomy T6–8 laminectomies T3–10 instrumentation & fusion | TP ICH | Baseline |
| Kaloostian PE |
64F | L1-S1 decompression, instrumentation & fusion | CBH + HCP | Died (CBH + HCP) |
| Kaloostian PE |
63M | Lumbar Laminectomy, instrumentation & fusion | CB SAH | Baseline |
| Kaloostian PE |
76M | L4 tumor resection & instrumentation & fusion | SDH | Baseline |
| Kaloostian PE |
77M | T11–S1 posterior instrumentation & fusion | CB SAH + IVH + HCP | Residual cognitive deficient, decrease mobility, died 9 months later (pneumonia) |
| L-2 pedicle subtraction osteotomy | ||||
| Kaloostian PE |
81F | L4-5 decompression, instrumentation & fusion | CBH + HCP | Died (CBH + HCP) |
| Morimoto T |
47M | Occipitocervical fusion and C1 posterior arch resection | SDH | Baseline |
| Haller JM |
58F | L3-4 decompression, instrumentation & fusion | CBH | Baseline |
| Floman Y |
75F | L2-5 decompression, instrumentation & fusion | CBH | Baseline |
| Floman Y |
67F | L4-5 decompression, instrumentation & fusion | CBH | Baseline |
| Floman Y |
56M | T10-S1 decompression, instrumentation & fusion | CBH | Baseline |
CBH, cerebellar hemorrhage; SDH, subdural hematoma; HCP, hydrocephalus; IVH, intraventricular hemorrhage; SAH, subarachnoid hemorrhage; CBI, cerebellar infarction; EDH, epidural hematoma.
Different etiologies can induce these intracranial haemorrhages involving previous head trauma, arteriovenous malformations, cerebral atrophy, cranial vault abnormalities, hemorrhagic diatheses, or the presence of cerebral aneurysms (4,7). However, none of these factors were present in our patient, nor were they the source of any of the cases in our literature review (Table 1). Instead, our patient was healthy and had no history of hypertension, head trauma or coagulopathy. In addition, dehydration has been described as a known risk factor for intracranial hemorrhage since it reduces brain volume and reduces low intracranial pressure that can increase blood vessel tension hence, making them more vulnerable to rupture (59,60). In our patient, no dehydration was reported throughout the surgery or preoperatively. Also, by positioning the head above the body’s horizontal plane can be considered another risk factor for intracranial bleeding. Chadduck reported a cerebellar hemorrhage case in a 59-year-old patient operated on in a sitting position after uncomplicated cervical laminectomy. The elevated position of the head is believed to cause a significant drop in CSF pressure and the development of cerebellar bleeding (27). Our patient was put in a reverse Trendelenburg position with the head being above the horizontal plane by approximately 10 degrees. A slightly head-down positioning during durotomy is recommended in order to lessen brain displacement (9).
Although the exact mechanism of intracranial hemorrhage is unknown, it is postulated that intracranial hematomas development is related to a persistent decrease in intracranial pressure due to loss of CSF volume leading to stretching and then tearing of bridging veins (13,14,61,62). Some authors also suggest that cerebellar hemorrhage can occur due to a drop in CSF pressure that induces downward displacement hence, injuring bridging cerebellar veins (cerebellar sag formation) (15,16). Göbel et al. (15) supported this phenomenon, who reported this as a cause of remote cerebellar hemorrhage after spinal surgery. Also, Friedman et al. (32) in 2002 reported two cases of cerebellar hemorrhage due to cerebellar sagging caused by dural spinal tear. We believe that the cause of intracranial bleeding in our patient was the sudden loss of a significant volume of CSF through the dural tear that induced the hemorrhage.
A CT-scan will confirm the diagnosis and must be performed as early as possible following the development of any concerning symptoms (63). It may show downward displacement of the brain and cerebellar tonsillar herniation, decrease in the size of the ventricles, meningeal enhancement, dilated epidural veins, or intracranial hemorrhage (13,19,63). In our patient, the CT scan demonstrated pneumocephalus and a moderate-sized subdural hematoma along with subarachnoid hemorrhage. The presence of pneumocephalus might be explained by the ‘inverted bottle mechanism’ which was reported in previous studies due to the negative pressure created by the CSF leak (39,64). We believe the acute right frontal-parietal subdural hematoma irritated the brain, which propagated the seizures. A significant concern in our case was the potential for further enlargement and increased mass effect of the subdural hematoma, which fortunately did not occur. In our review, we found that the most reported intracranial complications were: cerebellar hemorrhage (63.6%), subdural hematoma (25.4%), and hydrocephalus (20%) followed by intraventricular hemorrhage (5.45%), lobar hemorrhage, subarachnoid hemorrhage, pneumocephalus (9%), and finally cerebellar infarction and epidural hematoma (1.8%) of patients (Table 2).
Table 2
| % (n) | |
|---|---|
| CBH | 63.6% (35/55) |
| SDH | 25.4% (14/55) |
| HCP | 20% (11/55) |
| IVH | 5.45% (3/55) |
| Lobar ICH | 9% (5/55) |
| SAH | 9% (5/55) |
| Pn | 9% (5/55) |
| CBI | 1.8% (1/55) |
| EDH | 1.8% (1/55) |
CBH, cerebellar hemorrhage; SDH, subdural hematoma; HCP, hydrocephalus; IVH, intraventricular hemorrhage; SAH, subarachnoid hemorrhage; CBI, cerebellar infarction; EDH, epidural hematoma.
The management of acute SDH after CSF leak varies. Conservative treatment with bed rest, hydration and analgesia are recommended for a small hemorrhage without significant mass effect (32,34). Surgical intervention is often required for patients with extensive hemorrhages who have clinically significant neurological deficits (35). Most of the reported SDH cases usually have a benign course with good neurological recovery (33,38). Our literature review found that most patients improved clinically and returned to their baseline (69%), but 18.2% developed neurological symptoms and/or deficits, and 12.7% died (28,29,36,37,40-58,65,66). The cause of death in most patients was related to pneumonia (57.1%), followed by cerebellar hemorrhage with hydrocephalus in 42.8% of patients (Tables 3,4). In the present case, our patient was managed conservatively in the ICU, and his clinical symptoms improved without surgical intervention.
Table 3
| % (n) | |
|---|---|
| Baseline | 69% (38/55) |
| Residual neurological symptoms and/or deficits | 18.2% (10/55) |
| Death | 12.7% (7/55) |
Table 4
| % (n) | |
|---|---|
| Pneumonia | 57.1% (4/7) |
| CBH + HCP | 42.8% (3/7) |
CBH, cerebellar hemorrhage; HCP, hydrocephalus.
Conclusions
A subdural hematoma is a rare but potentially serious complication after CSF leak due to iatrogenic durotomy during spinal surgery. Rapid repair of incidental durotomy should be performed immediately to decrease the volume of CSF leakage, and a Valsalva maneuver should be done to ensure adequate closure to prevent this type of complication. The presence of seizures after spine surgery should alert the physician for postoperative intracranial hemorrhage. A CT scan should be done immediately after the surgery to verify the diagnosis and exclude any other possible structural causes of intracranial bleeding. Management is based on the intracranial radiographic findings and neurological status of the patient.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://dx.doi.org/10.21037/jss-20-642
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/jss-20-642). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participant were in accordance with the ethical standards of the institutional and national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient, to allow presentation of his case.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license).
References
- Kraemer R, Wild A, Haak H, et al. Classification and management of early complications in open lumbar microdiscectomy. Eur Spine J 2003;12:239-46. [Crossref] [PubMed]
- Lindley EM, McCullough MA, Burger EL, et al. Complications of axial lumbar interbody fusion. J Neurosurg Spine 2011;15:273-9. [Crossref] [PubMed]
- Wang JC, Bohlman HH, Riew KD. Dural tears secondary to operations on the lumbar spine. Management and results after a two-year-minimum follow-up of eighty-eight patients. J Bone Joint Surg Am 1998;80:1728-32. [Crossref] [PubMed]
- Gaucher DJ Jr, Perez JA Jr. Subdural hematoma following lumbar puncture. Arch Intern Med 2002;162:1904-5. [Crossref] [PubMed]
- Wells JB, Sampson IH. Subarachnoid hemorrhage presenting as post-dural puncture headache: a case report. Mt Sinai J Med 2002;69:109-10. [PubMed]
- Sköldefors EK, Olofsson CI. Intracranial subdural haematoma complicates accidental dural tap during labour. Eur J Obstet Gynecol Reprod Biol 1998;81:119-21. [Crossref] [PubMed]
- Acharya R, Chhabra SS, Ratra M, et al. Cranial subdural haematoma after spinal anaesthesia. Br J Anaesth 2001;86:893-5. [Crossref] [PubMed]
- Dardik A, Perler BA, Roseborough GS, et al. Subdural hematoma after thoracoabdominal aortic aneurysm repair: an underreported complication of spinal fluid drainage? J Vasc Surg 2002;36:47-50. [Crossref] [PubMed]
- Cammisa FP Jr, Girardi FP, Sangani PK, et al. Incidental durotomy in spine surgery. Spine (Phila Pa 1976) 2000;25:2663-7. [Crossref] [PubMed]
- Narotam PK, José S, Nathoo N, et al. Collagen matrix (DuraGen) in dural repair: analysis of a new modified technique. Spine (Phila Pa 1976) 2004;29:2861-7; discussion 2868-9. [Crossref] [PubMed]
- Khalatbari MR, Khalatbari I, Moharamzad Y. Intracranial hemorrhage following lumbar spine surgery. Eur Spine J 2012;21:2091-6. [Crossref] [PubMed]
- Kaloostian PE, Kim JE, Bydon A, et al. Intracranial hemorrhage after spine surgery. J Neurosurg Spine 2013;19:370-80. [Crossref] [PubMed]
- Sciubba DM, Kretzer RM, Wang PP. Acute intracranial subdural hematoma following a lumbar CSF leak caused by spine surgery. Spine (Phila Pa 1976) 2005;30:E730-2. [Crossref] [PubMed]
- Yamashima T, Friede RL. Why do bridging veins rupture into the virtual subdural space? J Neurol Neurosurg Psychiatry 1984;47:121-7. [Crossref] [PubMed]
- Göbel F, Heidecke V, Hube R, et al. Cerebellar hemorrhage as an early complication of spinal operations. 2. Case reports and review of the literature. Z Orthop Ihre Grenzgeb 1999;137:371-5. [PubMed]
- Brockmann MA, Nowak G, Reusche E, et al. Zebra sign: cerebellar bleeding pattern characteristic of cerebrospinal fluid loss. Case report. J Neurosurg 2005;102:1159-62. [Crossref] [PubMed]
- Jones AA, Stambough JL, Balderston RA, et al. Long-term results of lumbar spine surgery complicated by unintended incidental durotomy. Spine (Phila Pa 1976) 1989;14:443-6. [Crossref] [PubMed]
- Hagen R, Engesaeter LB. Unilateral and bilateral partial laminectomy in lumbar disc prolapse. A follow-up study of 156 patients. Acta Orthop Scand 1977;48:41-6. [Crossref] [PubMed]
- Beier AD, Soo TM, Claybrooks R. Subdural hematoma after microdiscectomy: a case report and review of the literature. Spine J 2009;9:e9-e12. [Crossref] [PubMed]
- Bosacco SJ, Gardner MJ, Guille JT. Evaluation and treatment of dural tears in lumbar spine surgery: a review. Clin Orthop Relat Res 2001;238-47. [Crossref] [PubMed]
- Du JY, Aichmair A, Kueper J, et al. Incidental durotomy during spinal surgery: a multivariate analysis for risk factors. Spine (Phila Pa 1976) 2014;39:E1339-E1345. [Crossref] [PubMed]
- Yoshihara H, Yoneoka D. Incidental dural tear in spine surgery: analysis of a nationwide database. Eur Spine J 2014;23:389-94. [Crossref] [PubMed]
- Takahashi Y, Sato T, Hyodo H, et al. Incidental durotomy during lumbar spine surgery: risk factors and anatomic locations: clinical article. J Neurosurg Spine 2013;18:165-9. [Crossref] [PubMed]
- Assietti R, Kibble MB, Bakay RA. Iatrogenic cerebrospinal fluid fistula to the pleural cavity: case report and literature review. Neurosurgery 1993;33:1104-8. [Crossref] [PubMed]
- Ishikura H, Ogihara S, Oka H, et al. Risk factors for incidental durotomy during posterior open spine surgery for degenerative diseases in adults: A multicenter observational study. PLoS One 2017;12:e0188038 [Crossref] [PubMed]
- Herren C, Sobottke R, Mannion AF, et al. Incidental durotomy in decompression for lumbar spinal stenosis: incidence, risk factors and effect on outcomes in the Spine Tango registry. Eur Spine J 2017;26:2483-95. [Crossref] [PubMed]
- Chadduck WM. Cerebellar hemorrhage complicating cervical laminectomy. Neurosurgery 1981;9:185-9. [Crossref] [PubMed]
- Mikawa Y, Watanabe R, Hino Y, et al. Cerebellar hemorrhage complicating cervical durotomy and revision C1-C2 fusion. Spine (Phila Pa 1976) 1994;19:1169-71. [Crossref] [PubMed]
- Andrews RT, Koci TM. Cerebellar herniation and infarction as a complication of an occult postoperative lumbar dural defect. AJNR Am J Neuroradiol 1995;16:1312-5. [PubMed]
- Burkhard PR, Duff JM. Bilateral subdural hematomas following routine lumbar diskectomy. Headache 2000;40:480-2. [Crossref] [PubMed]
- Lu CH, Ho ST, Kong SS, et al. Intracranial subdural hematoma after unintended durotomy during spine surgery. Can J Anaesth 2002;49:100-2. [Crossref] [PubMed]
- Friedman JA, Ecker RD, Piepgras DG, et al. Cerebellar hemorrhage after spinal surgery: report of two cases and literature review. Neurosurgery 2002;50:1361-3; discussion 1363-4. [PubMed]
- Hentschel SJ, Rhines LD, Wong FC, et al. Subarachnoid-pleural fistula after resection of thoracic tumors. J Neurosurg 2004;100:332-6. [PubMed]
- Kuhn J, Hofmann B, Knitelius HO, et al. Bilateral subdural haematomata and lumbar pseudomeningocele due to a chronic leakage of liquor cerebrospinalis after a lumbar discectomy with the application of ADCON-L gel. J Neurol Neurosurg Psychiatry 2005;76:1031-3. [Crossref] [PubMed]
- Karaeminogullari O, Atalay B, Sahin O, et al. Remote cerebellar hemorrhage after a spinal surgery complicated by dural tear: case report and literature review. Neurosurgery 2005;57:E215-discussion E215. [PubMed]
- Farag E, Abdou A, Riad I, et al. Cerebellar hemorrhage caused by cerebrospinal fluid leak after spine surgery. Anesth Analg 2005;100:545-6. [Crossref] [PubMed]
- Konya D, Ozgen S, Pamir MN. Cerebellar hemorrhage after spinal surgery: case report and review of the literature. Eur Spine J 2006;15:95-9. [Crossref] [PubMed]
- Ozturk E, Kantarci M, Karaman K, et al. Diffuse pneumocephalus associated with infratentorial and supratentorial hemorrhages as a complication of spinal surgery. Acta Radiol 2006;47:497-500. [Crossref] [PubMed]
- Chalela JA, Monroe T, Kelley M, et al. Cerebellar hemorrhage caused by remote neurological surgery. Neurocrit Care 2006;5:30-4. [Crossref] [PubMed]
- Zimmerman RM, Kebaish KM. Intracranial hemorrhage following incidental durotomy during spinal surgery. A report of four patients. J Bone Joint Surg Am 2007;89:2275-9. [Crossref] [PubMed]
- Calisaneller T, Yilmaz C, Ozger O, et al. Remote cerebellar haemorrhage after spinal surgery. Can J Neurol Sci 2007;34:483-4. [Crossref] [PubMed]
- Hashidate H, Kamimura M, Nakagawa H, et al. Cerebellar hemorrhage after spine surgery. J Orthop Sci 2008;13:150-4. [Crossref] [PubMed]
- Cevik B, Kirbas I, Cakir B, et al. Remote cerebellar hemorrhage after lumbar spinal surgery. Eur J Radiol 2009;70:7-9. [Crossref] [PubMed]
- Ulivieri S, Neri L, Oliveri G. Remote cerebellar haematoma after lumbar disc surgery. Case report. Ann Ital Chir 2009;80:219-20. [PubMed]
- Nam TK, Park SW, Min BK, et al. Remote cerebellar hemorrhage after lumbar spinal surgery. J Korean Neurosurg Soc 2009;46:501-4. [Crossref] [PubMed]
- Jung YY, Ju CI, Kim SW. Bilateral Subdural Hematoma due to an Unnoticed Dural Tear during Spine Surgery. J Korean Neurosurg Soc 2010;47:316-8. [Crossref] [PubMed]
- Gul S, Kalayci M, Acikgoz B. A rare complication of spinal surgery: cerebellar hemorrhage. Turk Neurosurg 2010;20:413-7. [PubMed]
- Nowak R, Maliszewski M, Krawczyk L. Intracranial subdural hematoma and pneumocephalus after spinal instrumentation of myelodysplastic scoliosis. J Pediatr Orthop B 2011;20:41-5. [Crossref] [PubMed]
- Fernandez-Jara J, Jorge-Blanco A, Carro-Martinez AI, et al. Remote cerebellar hemorrhage after lumbar spinal surgery. Emerg Radiol 2011;18:177-80. [Crossref] [PubMed]
- Hempelmann RG, Mater E. Remote intracranial parenchymal haematomas as complications of spinal surgery: presentation of three cases with minor or untypical symptoms. Eur Spine J 2012;21:S564-8. [Crossref] [PubMed]
- You SH, Son KR, Lee NJ, et al. Remote cerebral and cerebellar hemorrhage after massive cerebrospinal fluid leakage. J Korean Neurosurg Soc 2012;51:240-3. [Crossref] [PubMed]
- Lee HY, Kim SH, So KY. Seizure and delayed emergence from anesthesia resulting from remote cerebellar hemorrhage after lumbar spine surgery -A case report-. Korean J Anesthesiol 2012;63:270-3. [Crossref] [PubMed]
- Utku U, Güler S, Yalnız E, et al. Subdural and cerebellar hematomas which developed after spinal surgery: a case report and review of the literature. Case Rep Neurol Med 2013;2013:431261 [Crossref] [PubMed]
- Cavanilles-Walker JM, Tomasi SO, Sgier F, et al. Remote cerebellar haemorrhage after lumbar spine surgery: case report. Arch Orthop Trauma Surg 2013;133:1645-8. [Crossref] [PubMed]
- Choi BW, Lee SM, Yoon MG, et al. Cerebellar Hemorrhage after Posterior Lumbar Decompression and Interbody Fusion Complicated by Dural Tear: A Case Report. J Korean Soc Spine Surg 2014;21:183-8. [Crossref]
- Morimoto T, Shiraki M, Otani K, et al. Supratentorial subdural hemorrhage of a previous head injury and cerebellar hemorrhage after cervical spinal surgery: a case report and review of the literature. Spine (Phila Pa 1976) 2014;39:E743-7. [Crossref] [PubMed]
- Haller JM, Calvert G, Spiker WR, et al. Remote Cerebellar Hemorrhage after Revision Lumbar Spine Surgery. Global Spine J 2015;5:535-7. [Crossref] [PubMed]
- Floman Y, Millgram MA, Ashkenazi E, et al. Remote Cerebellar Hemorrhage Complicating Unintended Durotomy in Lumbar Spine Surgery. Int J Spine Surg 2015;9:29. [Crossref] [PubMed]
- Chodobski A, Szmydynger-Chodobska J, McKinley MJ. Cerebrospinal fluid formation and absorption in dehydrated sheep. Am J Physiol 1998;275:F235-8. [PubMed]
- Lu YH, Liaw WJ, Chang WT, et al. Stroke-like complication after abdominal surgery: a case report of chronic subdural hematoma. Zhonghua Yi Xue Za Zhi (Taipei) 1994;54:141-4. [PubMed]
- Mayfrank L, Laborde G, Lippitz B, et al. Bilateral chronic subdural haematomas following traumatic cerebrospinal fluid leakage into the thoracic epidural space. Acta Neurochir (Wien) 1993;120:92-4. [Crossref] [PubMed]
- Morandi X, Haegelen C, Henaux PL, et al. Brain shift is central to the pathogenesis of intracerebral haemorrhage remote from the site of the initial neurosurgical procedure. Med Hypotheses 2006;67:856-9. [Crossref] [PubMed]
- García-Morales I, Porta-Etessam J, Galán L, et al. Recurrent subdural haematomas in a patient with spontaneous intracranial hypotension. Cephalalgia 2001;21:703-5. [Crossref] [PubMed]
- Yoon SJ, Oh GS, Lee SJ, et al. Pneumocephalus in patients with orthostatic headache. J Clin Neurol 2008;4:89-93. [Crossref] [PubMed]
- Guerin P, El Fegoun AB, Obeid I, et al. Incidental durotomy during spine surgery: incidence, management and complications. A retrospective review. Injury 2012;43:397-401. [Crossref] [PubMed]
- Castle M, Barrena C, Samprón N, et al. Remote cerebellar haemorrhage after lumbar arthrodesis: case report and literature review. Neurocirugia (Astur) 2011;22:574-8. [PubMed]


