
Return to golf after adult degenerative and deformity spine surgery: a preliminary case series of how surgery impacts golf play and performance
Introduction
Degenerative spine disease is a common ailment among older adults, negatively affecting quality of life and the ability to enjoy hobbies. Cervical and lumbar degeneration with concomitant neck and back pain affect approximately 60% of adults in their sixth decade of life (1,2). Quality of life associated with degenerative spine conditions is analogous to living with brain tumors and/or cancer (3), and those suffering spinal deformity have a quality of life similar to patients with blindness, emphysema, renal failure, and stroke (4). From 1988 to 2012, rates of spine surgery have increased 4-fold, with higher rates in patients ≥70 years (5). A similar uptick in spinal deformity surgery has been seen, with a 3.4-fold increase in patients ≥60 years from 2004 to 2011 (6). Understanding how degenerative and deformity spine conditions, along with associated surgical intervention, impacts quality of life in an elderly population can be of benefit to surgeons and patients.
Golf is a recreational sport enjoyed by many older individuals, with 34.2 million Americans playing golf in 2019, of which 5.3 million were ≥65 years (7). Older individuals ≥65 years also play golf 3-times more often than younger individuals aged 18–34 years, likely a byproduct of retirement (7). Golf is an excellent source of physical activity for older people and has been linked to improved cardiovascular health that likely comes from walking the course (8). Prior studies have shown that degenerative spine conditions can significantly hinder golf frequency and performance (9,10). Authors have also suggested that golf may predispose athletes to spinal injury, as lumbar spine ailments are the most common injury incurred in golfers, making up to 22–34% of all golfing injuries (11). Moreover, low handicap golfers have been shown to generate more torque throughout their swing than medium or high-handicap golfers (12). Due to the unnatural strains placed on the low back during a violent golf swing, authors have analogized golf to a “contact sport” given the high risk of spine injury (13-15). Though much research focuses on low back injury prevention in golfers (16,17), which includes swing modification, muscle conditioning, and flexibility training, few discuss the need for surgery. The ability to return to golf after spine surgery is an important factor that many patients consider when deciding to pursue surgical treatment, and little evidence exists to guide these important quality of life decisions (9,10).
Given the overlap of patients with degenerative spine disease who also enjoy recreational golf, an in-depth study of golf after spine surgery was undertaken. While return to golf after upper and lower extremity surgery has been studied (8,18), golf participation and performance after spine surgery is understudied. Several cross-sectional survey studies provide hypothetical surgeon responses on how to manage return to golf after spine surgery (14,19); however, without primary patient data, treatment-altering conclusions cannot be made.
The objective of the current study was to provide in-depth information on how golfers fared after spine surgery. In a cohort of self-identified, avid golfers undergoing degenerative or deformity spine surgery, we sought to describe the: (I) presentation, (II) operative treatment, and (III) return-to-play (RTP) process in this population.
We present the following article in accordance with the STROBE reporting checklist (available at https://dx.doi.org/10.21037/jss-21-43).
Methods
Study design
A retrospective, single-institution case series of adults >18 years undergoing degenerative or deformity spine surgery from 2015–2019 who self-identified as avid, recreational golfers was conducted. Degenerative surgery was a-priori defined as ≤4 level decompression and/or fusion of the cervical or lumbar spine due to degenerative pathology. Spinal deformity surgery was a-priori defined as ≥6 level instrumented fusion with at least one of the following radiographic criteria [Cobb angle>30°, sagittal vertical axis (SVA) >5 cm, coronal vertical axis (CVA) >3 cm, pelvic tilt (PT) of >25°, or thoracic kyphosis (TK) >60°]. All patients underwent regional X-rays or standing full-spine low dose Stereoradiograph X-rays (EOS Imaging, Paris, France). This study obtained the institution’s IRB approval (IRB# AAAT3012) prior to conducting study activities, and was exempted from needing an informed consent. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Data collection
Demographic, presentation, and operative information were collected from the electronic medical record (EMR). Preoperative and postoperative clinic notes, operative reports, relevant imaging, and anesthetic care records were reviewed, along with inpatient documentation. In addition to a thorough EMR review, patients were contacted directly by telephone to gather the following sport-specific information: years of golf played prior to surgery, numerical rating scale (NRS) pain scores before and after surgery, time of RTP after surgery, 18-hole rounds of golf per month before and after surgery, handicap before and after surgery, and self-perceived golf effort/performance level before and after surgery. For the “effort/performance level,” athletes were asked to rate the amount of effort they could put forth given their symptoms and/or how well they were able to perform on a scale of 1–10: 1= poorest effort/performance and 10= best effort/performance. Golf handicaps were used as a metric as well, with a positive number representing number of strokes above par.
Return to play
RTP was dichotomized into two endpoints. First RTP was defined as the time point when patients returned to any golf-specific physical activity, such as the driving range or practice rounds. Full RTP was defined as the time point when patients were no longer limited by their pathology and/or surgery and could play a full round of golf uninhibited. In addition, four total time points were assessed: (I) pre-pathology: time before any symptoms developed; (II) mid-pathology: time when symptoms were at worst prior to surgery; (III) First RTP: (defined above), and (IV) Full RTP: (defined above).
In terms of postoperative recovery practices, specific instructions were given to both cervical degenerative, lumbar degenerative and deformity patients. Cervical fusions were cleared to pitch/putt with a hard collar after 6 weeks, with full return to golf after 3 months. Lumbar fusion patients were cleared to pitch/putt at 3 months, with full return to golf after 6 months. Deformity patients were similarly cleared to pitch/putt at 3 months, with a more conservative full return to golf in the 6–12 months range depending on the extent of surgery, the patient’s comfort level, and their overall recovery. Throughout the recovery process and with all return to physical activity, patients were counseled to listen to their body, and if they had significant pain with any movement, to limit that amount of activity. Specific to golf, patients were counseled to be mindful during their full swing for excessive twisting of the lower trunk and when bending down to pick-up the ball or place it on a tee, to bend with their hips/knees rather than their lower back.
Statistical analysis
Descriptive statistics were used to summarize each patient’s course. Categorical data were presented using frequencies and percentages, while continuous data were presented as means and standard deviations (SD). Due to the small sample size of 6 patients, minimal statistical analysis was performed. Student’s t-tests were used to assess changes in NRS pain scores before and after surgery. All statistical analyses were performed in STATA version 14 (StataCorp LP, College Station, Texas, USA).
Results
Presentation and operative treatment
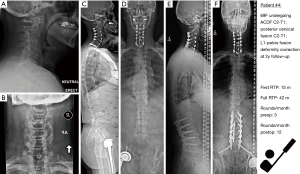
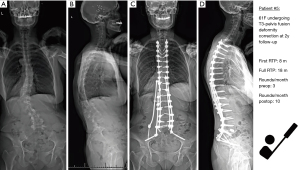
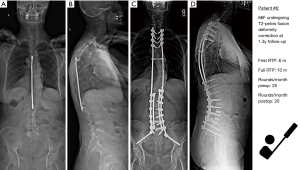
Among 6 golfers undergoing degenerative or deformity spine surgery, mean age was 60 years, and 5 of 6 (83%) patients were female (Table 1). All patients were self-identified, avid golfers with a mean experience of 31 years, except for Patient 3 who started later in life and had 9 years of experience. Three patients underwent degenerative surgery (Patients 1–3), while three patients underwent deformity surgery (Patients 4–6). Patients underwent a mean of 9.7 years of non-operative treatment prior to pursuing surgery. Operations ranged from single-level open transforaminal lumbar interbody fusion (TLIF) fusion (Patients 1 & 3), cervical laminoplasty (Patient 2), to larger deformity operations, including cervical and lumbar decompression and kyphosis correction (Patient 3), and thoracolumbar deformity correction (Patients 5 & 6). Patient 4 underwent 3 total planned operations: anterior cervical discectomy and fusion (ACDF), posterior cervical decompression and fusion, and posterior lumbar fusion, done over a 2.5-month period (11/16/2015–1/26/2016). All other patients underwent a single-stage operation. Of note Patient 4 underwent 1 unplanned reoperation due to new left iliopsoas weakness after the lumbar decompression/fusion due to increased lordosis at L2/3 causing retrolisthesis and narrowing of the left L2/3 and L3/4 foramen, which required revision bilateral laminotomies at L2/3 and L3/4 on postoperative day 3. Additionally, Patient 5 had a cerebrospinal fluid (CSF) leak that required reoperation at 5 weeks postoperative.
Table 1
| Pathology | Degenerative | Deformity | |||||
|---|---|---|---|---|---|---|---|
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | ||
| Follow-up time | 5 years | 5 years | 4 years | 5 years | 2 years | 1.3 years | |
| Age/sex | 48/F | 55/M | 67/F | 69/F | 61/F | 66/F | |
| Golf experience (years) | 28 | 40 | 9 | 62 | 20 | 25 | |
| Diagnosis | Lumbar stenosis; focal kyphosis | Cervical myeloradiculopathy | Lumbar stenosis | Cervical myeloradiculopathy; flat back syndrome, lumbar stenosis | Coronal and sagittal malalignment | Rigid thoracic hyperkyphosis, lumbar scoliosis | |
| Length of non-surgical treatment (years) | 20 | 5 | 12 | 2 | 8 | 11 | |
| Preop NRS Pain Score | Back 8 | Neck 10 | Back 6 | Back 10; neck 8 | Back 8 | Back 6 | |
| Leg 9 | Arm 10 | Leg 10 | Leg 8; arm 7 | Leg 0 | Leg 0 | ||
| Postop NRS Pain Score | Back 1 | Neck 0 | Back 0 | Back 0; neck 0 | Back 0 | Back 4 | |
| Leg 2 | Arm 0 | Leg 1 | Leg 0; arm 0 | Leg 0 | Leg 0 | ||
| Operation | L4/5 open TLIF | C3-7 laminoplasty | L4/5 open TLIF | ACDF C2-T1; posterior cervical fusion C2-T1; L1-pelvis decompression/fusion | T3-pelvis deformity correction, PCOs T10-S1, L5/S1 TLIF w/kickstand rod | T2-pelvis deformity correction, L4/5 and L5/S1 TLIF, L3-S1 PCOs | |
| First RTP (months) | 5 | 2 | 6 | 15 | 8 | 6 | |
| Full RTP (months) | 6 | 2 | 18 | 42 | 18 | 10 | |
NRS, numerical rating scale; ACDF, anterior cervical discectomy and fusion; RTP, return-to-play; TLIF, transforaminal lumbar interbody
Postoperative course
Preoperative and postoperative NRS pain scores are provided, at a mean follow-up of 3.7 years (Table 1). Mean preoperative NRS back/neck pain was 9.7, which decreased to 0.8 postoperatively (P<0.001). Mean preoperative NRS leg/arm pain was 6.2, which decreased to 0.5 postoperatively (P<0.001). Compared to the degenerative lumbar patients, the two thoracolumbar deformity patients had no leg pain preoperatively or postoperatively, but endorsed significant preoperative back pain secondary to their deformity.
Return to play
Not surprisingly, players undergoing smaller operations (lumbar fusion/laminoplasty) returned to golf sooner than patients undergoing larger deformity corrections, with a mean first RTP of 4.3 months for degenerative patients vs. 9.7 months among deformity patients (Table 1; Figure 1). With respect to full RTP, averages are not presented due to 2 patients that were outliers. Among the 3 degenerative patients, Patients 1 and 2 returned to golf fully by 6 and 2 months, respectively; however, Patient 3 had a prolonged return at 18 months. Among deformity patients, Patients 5 and 6 returned by 18 and 10 months, yet Patient 4 had a prolonged return at 42 months, though this patient underwent 4 total operations over a 2.5-month period.
Golf performance
Prior to surgery, several patients found many aspects of golf difficult, which included bunker play, long irons, and driving (Table 2). In addition, 3 patients endorsed that “everything” was difficult right before they needed surgery. Regarding frequency of 18-hole rounds per month, all patients played either the same or more rounds of golf after surgery once they reached full RTP (Table 2; Figure 2). Of note, the only patients that did not play more rounds per month after surgery were Patients 2 and 6, who were high-level golfers already playing 15 and 20 rounds per month, respectively, before surgery. They each returned to their preoperative frequency of rounds per month.
Table 2
| Pathology | Degenerative | Deformity | |||||
|---|---|---|---|---|---|---|---|
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | ||
| Most difficult part of golf prior to surgery | Bunker play; long irons | All aspects of game; “couldn’t golf at all” | All aspects of game; “could no longer walk the course” | “Everything except putting” | Driving off the tee | All aspects of game | |
| Rounds of 18-hole rounds of golf per month, |
2/4/6/10 | 15/0/15/15 | 0/2/2/6 | 3/0/3/12 | 3/0/2/10 | 20/15/8/20 | |
| More golf after surgery? | Yes | Same | Yes | Yes | Yes | Same | |
| Handicap, |
22/8/8/6 | 5/NA/5/5 | NA/NA/NA/25 | 15/NA/NA/15 | 30/NA/30/25 | 9/13/15/15 | |
| Self-perceived effort/performance level, |
10/4/6/8 | 10/1/10/10 | 10/3/8/10 | 10/1/5/10 | 10/1/6/10 | 10/7/5/9 | |
| Better performance after surgery? | Yes | Same | NA | Same | Yes | No | |
| Approximate 18-hole round score | 102/90/85/80 | 77/NA/79/79 | NA/NA/NA/93 | 90/NA/98/90 | 123/NA/120/100 | 78/85/95/92 | |
RTP, Return to Play; NA, not applicable; Pre-pathology: time before any symptoms developed; Mid-pathology: time when symptoms were at worst prior to surgery; First RTP: time point when patients returned to any golf-specific physical activity; Full RTP: time point when patients were no longer limited by their pathology and/or surgery and could play a full round of golf uninhibited. fusion; PCO, posterior column osteotomy.
In terms of performance, the handicap of all players improved after surgery to better than before surgery, except for one high-level golfer (Table 2; Figure 3). Patient 6 was scoring in the high 70s with a 9 handicap before her spinal deformity correction, yet was not able to return to this high-level of performance, and postoperatively had a handicap of 15, although she also had the shortest follow-up of all 6 patients and could potentially improve with time. Of note, Patient 3 took up golf more seriously postoperatively and was unable to compute a handicap until after full RTP.
With respect to self-perceived effort/performance level, prior to surgery patients were performing at a mean of 2.8 of their prior maximal effort/performance levels. After surgery, patients rated their own performance at a mean of 9.5 after full RTP (P<0.001) (Table 2). Representative deformity patients are summarized in Figures 4-6.
Discussion
The current pilot study sought to conduct an in-depth investigation of how patients return to golf after undergoing degenerative and deformity spine surgery. In 6 patients with a mean golfing experience of over 3 decades, all patients were able to return to playing golf at or more frequently than their preoperative status. Pain scores improved significantly in all patients at a mean follow-up of 3.7 years. As expected, degenerative patients returned sooner than deformity patients. All patients performed at a higher level after surgery, except for one high-level golfer whose handicap dropped slightly. Though this represents a preliminary study that requires replication in larger samples, it is our hope these early data can help surgeons and patients improve their understanding about return to golf after spine surgery and lead to larger, multi-institutional studies.
Though much has been written about golf after spine surgery, most studies lack primary data and instead report survey results or summarize existing data. Abla and colleagues (19) surveyed 523 spine surgeons about return to golf practices after common spine operations, such as lumbar decompression/fusion and ACDF. The majority of surgeons recommended a RTP time of 4–8 weeks after lumbar decompression, 2–3 months after ACDF, and 6 months after lumbar fusion. The authors also queried surgeons based on hypothetical, representative patients—retired male avid golfer, retired female weekend golfer, working male occasional golfer, collegiate golfer, and female professional golfer—and a shorter RTP was recommended for more competitive golfers. Though a useful survey study, no primary patient information was included, and only degenerative operations were discussed. In another review by Haddas et al. (14), the authors adequately summarized how to protect lumbar spine musculature while golfing, useful stretching techniques, and ways to maintain lumbar flexibility. The authors also asserted a void in the literature regarding RTP protocols and postoperative rehabilitation protocols for golfers undergoing lumbar spine surgery, particularly in those with high impact swings (14). The remaining literature presented discussed RTP in all sports, without mention of golf-specific studies. Again, no primary patient data was presented.
The 3 patients undergoing degenerative surgery in our study all first returned to golf in under 6 months, and 2 of 3 patients returned fully at 6 months. To our knowledge, only two studies have provided primary data on RTP in golfers after spine surgery. In a study of 34 patients undergoing elective cervical spine surgery only, Richards et al. (9) reported that 71% endorsed a decrease in golf ability due to their spine condition, and 68% successfully returned to golf postoperatively. Interestingly, 57% played the same amount or more after surgery, while 43% played less after surgery, which is in contrast to our results, where 100% of patients played the same or more postoperatively. In terms of performance, they reported 65% of patients played at the same or higher level after surgery, (9) contrary to our results, where all but one high-level golfer performed the same or better postoperatively. RTP time was >12 months in 40% of patients, also longer than our cohort of 3 patients. The second study by Shifflett and colleagues (10) surveyed 34 golfers undergoing 1 or 2-level degenerative lumbar spine fusion, including open posterior fusion (50%), anterior lumbar fusion (35%), and minimally invasive TLIF (15%). In 79% of golfers, back/leg pain negatively affected their ability to play golf, and by 1-year, 65% of patients returned to practice and 52% returned to course play (10). With respect to postoperative performance, 77% played the same amount or more postoperatively, and 80% reported the same or improved handicap (10). Unfortunately, postoperative follow-up did not extend past 1-year, thus we do not know the true rates of RTP. Interestingly, 9% of patients engaged in some sort of golf-specific rehabilitation, and the biggest decrease on their golf performance was driving distance in 50% of patients, while accuracy suffered only in 9%. Overall, the second study of degenerative lumbar fusion patients fits with the current data.
Patients undergoing cervical and thoracolumbar deformity correction each returned to golf successfully, albeit at a later time than degenerative patients. Among the existing literature of return to golf after spine surgery, only degenerative operations are discussed, without mention of larger spinal deformity reconstructions. Contrary to what most patients and surgeons may think, our results show that return to golf is possible after spinal deformity correction. The only data on RTP in deformity patients is limited to adolescent idiopathic scoliosis (AIS) patients, where approximately 50% of AIS patients returned to sports by 6-month. However, golf specifically was not mentioned, and adolescents bear little resemblance to adult deformity populations (20,21). One adult study assessed patient’s preoperative goals after deformity surgery and found that 37 of 59 patients (63%) stated that exercise or sport was a desired postoperative activity, but specific sports were not mentioned. To our knowledge, the return to golf data in the three deformity patients presented here may be some of the few, if any, currently presented in the literature.
It is our hope this data can be used to counsel patients undergoing spine surgery on their postoperative return to golf. Based on the initial results of our limited case series, we recommend golf practices be studied across multiple institutions in a more systematic and prospective manner. Instead of retrospectively asking patients to report golf practices, obtaining a larger sample of all types of golfers, those who play frequently and infrequently, will help us better understand the impact of surgery on the novice golfer. Moreover, engaging with sport-specific physical therapists may also assist with the RTP process.
The current study is not without limitation. The most important weakness is the small sample size of six patients. We strongly caution against applying these data to large populations, as this is a small, retrospective sample of patients undergoing spine surgery. We attempted to counteract this limitation by obtaining in-depth information on preoperative and postoperative golf practices. It would be inappropriate to apply the results of these six patients to all patients undergoing degenerative and deformity spinal surgery; rather, these results can be viewed as preliminary findings from a small sample that can help patients better understand their postoperative recovery. Second, all data are self-reported, without confirmation of actual playing practices. It is possible that rounds per month or handicaps may have been higher or lower than provided. Third, we included patients who self-identified as avid golfers, and it is entirely possible we did not capture patients who played recreationally and did not mention this to their spine surgeon. Moreover, it is possible these recreational golfers were not able to RTP successfully, and this information may have been missed. Thus, we caution against overinterpretation of this small sample. We very much view this study as a pilot analysis to be replicated prospectively across multiple institutions, with additional questions included such as rang of mobility, area of game impacted most (driving, irons, putting), disadvantageous golfing behaviors during the early and late recovery periods, and walking the course versus driving in a golf cart.
Conclusions
In 6 self-identified, avid golfers undergoing degenerative or deformity spine surgery with a mean follow-up of 3.7 years, all were able to return to playing golf at or more frequently than their preoperative status. Pain scores improved significantly in all patients. Degenerative patients returned to golf sooner than deformity patients, and all patients performed at a higher level after surgery, except for one high-level golfer whose handicap worsened slightly. These data provide baseline information for future, prospective studies enrolling all patients of golf skill level and playing frequency to learn more about golf after spine surgery.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://dx.doi.org/10.21037/jss-21-43
Data Sharing Statement: Available at https://dx.doi.org/10.21037/jss-21-43
Peer Review File: Available at https://dx.doi.org/10.21037/jss-21-43
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/jss-21-43). LGL reports personal fees from Medtronic, grants and personal fees from DePuy-Synthes Spine, personal fees from K2M, non-financial support from Broadwater, non-financial support from Seattle Science Foundation, grants and non-financial support from Scoliosis Research Society, non-financial support from Stryker Spine, non-financial support from The Spinal Research Foundation, grants from EOS, grants from Setting Scoliosis Straight Foundation, personal fees from Fox Rothschild, LLC, personal fees from Quality Medical Publishing, other from Evans Family Donation, other from Fox Family Foundation, grants and non-financial support from AOSpine, outside the submitted work. LGL serves as an unpaid editorial board member of Journal of Spine Surgery from Oct 2019 to Oct 2021. RAL reports consultant/royalty fees from Medtronic, research grants from Department of Defense, outside the submitted work. Dr. KDR reports royalties from Biomet, consulting fees from Nuvasive, and Happe Spine, stock or stock options from Axiomed, Expanding Orthopedics, Spineology, Spinal Kinetics, Amedica, Vertiflex, Benevenue, and Paradigm Spine, outside the submitted work. SZ serves as an unpaid editorial board member of Journal of Spine Surgery. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study has obtained the institution’s IRB approval prior to conducting study activities, and was exempted from needing an informed consent. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Moon MS, Yoon MG, Park BK, et al. Age-Related Incidence of Cervical Spondylosis in Residents of Jeju Island. Asian Spine J 2016;10:857-68. [Crossref] [PubMed]
- Horváth G, Koroknai G, Acs B, et al. Prevalence of low back pain and lumbar spine degenerative disorders. Questionnaire survey and clinical-radiological analysis of a representative Hungarian population. Int Orthop 2010;34:1245-9. [Crossref] [PubMed]
- Whittle IR, Scotland J, Dengu F, et al. Preoperative quality of life in patients with degenerative spinal disorders: many are worse than patients with brain tumours and cancer. Br J Neurosurg 2012;26:460-5. [Crossref] [PubMed]
- Smith JS, Line B, Bess S, et al. The Health Impact of Adult Cervical Deformity in Patients Presenting for Surgical Treatment: Comparison to United States Population Norms and Chronic Disease States Based on the EuroQuol-5 Dimensions Questionnaire. Neurosurgery 2017;80:716-25. [Crossref] [PubMed]
- Aizawa T, Kokubun S, Ozawa H, et al. Increasing Incidence of Degenerative Spinal Diseases in Japan during 25 Years: The Registration System of Spinal Surgery in Tohoku University Spine Society. Tohoku J Exp Med 2016;238:153-63. [Crossref] [PubMed]
- Sing DC, Berven SH, Burch S, et al. Increase in spinal deformity surgery in patients age 60 and older is not associated with increased complications. Spine J 2017;17:627-35. [Crossref] [PubMed]
- Foundation NG. Golf industry facts 2021 [cited 2021 February 14th, 2021]. Available online: https://www.ngf.org/golf-industry-research/
- Jackson JD, Smith J, Shah JP, et al. Golf after total knee arthroplasty: do patients return to walking the course? Am J Sports Med 2009;37:2201-4. [Crossref] [PubMed]
- Richards A, Pines A, Rubel NC, et al. Return to Golf, Tennis, and Swimming After Elective Cervical Spine Surgery. Cureus 2020;12:e9993 [Crossref] [PubMed]
- Shifflett GD, Hellman MD, Louie PK, et al. Return to Golf After Lumbar Fusion. Sports Health 2017;9:280-4. [Crossref] [PubMed]
- Robinson PG, Murray IR, Duckworth AD, et al. Systematic review of musculoskeletal injuries in professional golfers. Br J Sports Med 2019;53:13-8. [Crossref] [PubMed]
- Worsfold P, Smith NA, Dyson RJ. Low handicap golfers generate more torque at the shoe-natural grass interface when using a driver. J Sports Sci Med 2008;7:408-14. [PubMed]
- Deora H, Yagnick NS, Tripathi M, Mohindra S. Letter to the Editor: Is Golf the New Football or Have We Made It So? Sports Med Int Open 2019;3:E72-3.
- Haddas R, Pipkin W, Hellman D, et al. Is Golf a Contact Sport? Protection of the Spine and Return to Play After Lumbar Surgery. Global Spine J 2021; Epub ahead of print. [Crossref] [PubMed]
- Walker CT, Uribe JS, Porter RW. Golf: a contact sport. Repetitive traumatic discopathy may be the driver of early lumbar degeneration in modern-era golfers. J Neurosurg Spine 2019; Epub ahead of print. [Crossref] [PubMed]
- Gluck GS, Bendo JA, Spivak JM. The lumbar spine and low back pain in golf: a literature review of swing biomechanics and injury prevention. Spine J 2008;8:778-88. [Crossref] [PubMed]
- Goebel D, Drollinger F, Drollinger A. Lumbar Spine Injuries: Primary Prevention in Amateur and Professional Golf Players. Sports Med Int Open 2018;2:E179-84. [Crossref] [PubMed]
- Vives MJ, Miller LS, Rubenstein DL, et al. Repair of rotator cuff tears in golfers. Arthroscopy 2001;17:165-72. [Crossref] [PubMed]
- Abla AA, Maroon JC, Lochhead R, et al. Return to golf after spine surgery. J Neurosurg Spine 2011;14:23-30. [Crossref] [PubMed]
- Sellyn GE, Hale AT, Tang AR, et al. Pediatric thoracolumbar spine surgery and return to athletics: a systematic review. J Neurosurg Pediatr 2019; Epub ahead of print. [Crossref] [PubMed]
- Sarwahi V, Wendolowski S, Gecelter R, et al. When Do Patients Return to Physical Activities and Athletics After Scoliosis Surgery?: A Validated Patient Questionnaire Based Study. Spine (Phila Pa 1976) 2018;43:167-71. [Crossref] [PubMed]





