
Evolution of vertebral posttraumatic necrosis to bone healing after self-stabilizing osteophytosis development—case report
Introduction
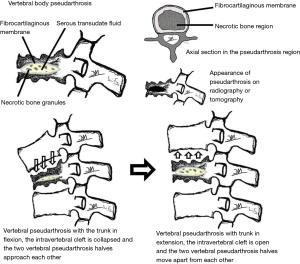
Post-traumatic vertebral necrosis and pseudarthrosis at the thoracolumbar transition level usually progresses to bone resorption, leading to vertebral collapse, sometimes with retropulsion of the posterior wall, and to invasion of the vertebral canal by bone fragments that can cause neurological injury (Figure 1). Due to this frequent unfavorable evolution of vertebral pseudarthrosis, early percutaneous surgical stabilization of symptomatic vertebral pseudarthrosis is usually indicated, allowing for practically immediate pain relief and functional improvement, which is beneficial in terms of health and quality of life (1-7). However, because of the current surgical indication for vertebral pseudarthrosis, there is a lack of recent studies about its natural evolution and conservative treatment outcomes.
We present the following article in accordance with the CARE reporting checklist (available at https://dx.doi.org/10.21037/jss-21-58).
Case presentation
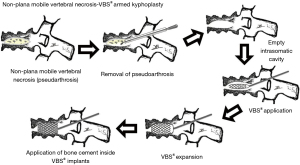
We present the case of a 77-year-old male patient with a history of overweight and arterial hypertension, who appeared in a wheelchair at the clinic office, with complaints of axial pain at the thoracolumbar transition level. The patient was previously autonomous and active. This pain was more intense when he changed from a sitting to an upright position and led to him only being able to deambulate with a walker. The pain substantially decreased in the decubitus position. He had no signs of radiculopathy or any associated neurological deficit. The pain started progressively in the previous month and was more intense at the present moment, rated as 8/10 on the visual analogue pain scale (8). He reported having suffered a fall from his own height 2 months before, with direct trauma to the thoracolumbar transition region. However, he did not go to health care because he only reported mild axial pain [rated as 2/10 on the visual analogue pain scale (8)], which improved with oral acetaminophen. Radiographs and computed tomography were then performed, identifying flattening of the L1 vertebral body with the presence of a vacuum sign or intravertebral cleft, compatible with pseudarthrosis, with non-plana vertebra morphology and reaching the posterior wall, without relevant retropulsion (Figure 2). This finding raised the suspicion of a probable initial type cephalic A3 fracture, based on AOSpine classification (9). Given the presence of vertebral pseudarthrosis located in the thoracolumbar transition and reaching the posterior wall (with a high probability of progressive vertebral flattening and eventual collapse), as well as pain classified as 8/10 of the visual analogue pain scale, significant gait limitation, and a calculated Oswestry disability index of 84 points, surgical treatment of armed kyphoplasty and adjacent percutaneous pedicle instrumentation was proposed to the patient (Figure 3) (8,10).

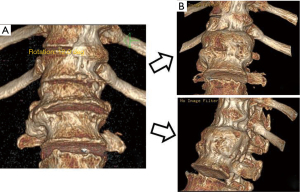
Nevertheless, the patient refused any type of surgical intervention, in spite of having been informed and having understood the risks of the frequent unfavorable evolution of vertebral pseudarthrosis, including severe neurological damage. Therefore, the use of a Jewett-type brace was indicated whenever he moved to an upright position, symptomatic control with analgesics and surveillance for signs of radiculopathy or neurological deficits, maintaining a monthly follow-up in clinic office, with clinical and radiographic control. Due to the COVID-19 pandemic and consequent delays in appointments and physical isolation, the patient only returned to the clinic office 6 months after. He was walking with one crutch and reporting a decrease in pain at the thoracolumbar transition to 2/10 of the visual analogue pain scale (8). He no longer felt pain at digital pressure of the L1 spinous process. Furthermore, the axial impact test of the body on the heels did not arise back pain. He reported that after the last appointment before the pandemic, he maintained overlapping pain and functional limitation for another 4 months and was even bedridden for periods of 1 and 2 weeks when the pain was more severe. However, after this period, he reported a progressive improvement and over the previous 2 months he felt less axial pain, which allowed him to progressively resume daily activities. The evaluation of the Oswestry score in this appointment was 50 points (10). Radiographs and computed tomography were performed, which showed bone healing of the vertebra, with flattening of two-thirds of the original vertebral height, no longer showing signs of intrasomatic cleft, and with the presence of an anterior bone mass about 1 cm thick, joining the vertebral bodies of the D12-L1-L2 segment anteriorly (Figures 3,4). The patient was reassessed after 2 months, and was already able to walk autonomously, without external support. He reported pain classified as grade 1/10 of the visual analogue pain scale and he now changes from a sitting to an upright position without any aggravating pain. We calculated an Oswestry score of 18 points (8,10).
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Currently it is considered that the natural history of the vertebral nonunion and pseudarthrosis ends in vertebral body collapse, kyphosis and spinal cord compression, so it is prudent to stop this course of events and prevent such consequences. Because of this unfavorable disease progression and knowing that pseudarthrosis and the necrotic bone do not heal for themselves, conservative treatment is often ineffective and currently considered the last treatment option for this pathology in a previously active patient. As such, the treatment of vertebral symptomatic pseudarthrosis is surgical, including percutaneous cement stabilization by vertebroplasty or kyphoplasty, with or without expandable implants, and cemented screw stabilization at an early stage when there is still a vertebral body. The literature shows similar outcomes to all these minimally invasive stabilization techniques (11-24). Decompression and posterior or anterior fusion are indicated when neurological injury or a severe vertebral body collapse are present. The goal is to avoid the late stage, which usually requires a more invasive surgery, in old and fragile patients (25,26).
In this case, excessive mobility of a vertebral fracture at the initially undiagnosed thoracolumbar transition probably led to evolution to symptomatic pseudarthrosis, as demonstrated by the presence of an intravertebral cleft and the typical mechanical pain, which means a type of posttraumatic vertebral necrosis with intrasomatic mobility (Figure 1). Despite presenting risk factors for unfavorable evolution, such as being located at the thoracolumbar transition, reaching the posterior wall and with the presence of an important sized intravertebral cleft, this patient’s pseudarthrosis evolved favorably, with clinical improvement, probably due to the development of a stabilizing anterior bone mass of the vertebral body, joining the vertebra to the adjacent bodies along their anterolateral sides (1-7). Vertebrae stabilization would have minimized the pathological hypermobility that perpetuated pseudarthrosis, allowing for the clinically and imagiologically proven bone healing of the vertebrae (Figure 5). As far as we are concerned, the evolution of a vertebral pseudarthrosis that self-stabilized with the development of an anterior osteophyte mass, joining the adjacent vertebrae, has not been described in the scientific literature to date. Even so, we must pay attention to the fact it took a period of 4 to 6 months for the patient to present symptomatic improvement. It is currently considered an excessive period of disabling complaints, which, according to the literature, can be avoided with a percutaneous vertebral stabilization with bone cement, usually obtaining immediate symptomatic relief and functional improvement. Also, the prolonged time of bedridden and immobilization time with a brace can be harmful for elderly patients, frequently due to other diseases that can aggravate with immobilization and loss of back muscle strength (1-7,11-24).
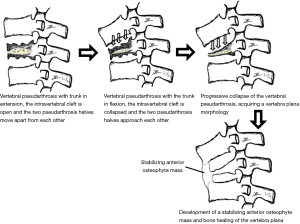
As such, despite the favorable evolution of this rare clinical case, we consider that the treatment of symptomatic vertebral pseudarthrosis of the thoracolumbar transition in a previously active patient is surgical and should be carried out as early as possible in order to avoid the most frequent evolution of this entity, that is, vertebral collapse, posterior wall retropulsion and neurological deficits. We therefore consider that in spite of the unusually favorable evolution of this clinical case, in order to avoid highly disabling symptoms for several months, early percutaneous cement stabilization of symptomatic vertebral pseudarthrosis is indicated, allowing for practically immediate pain relief and functional improvement, which is beneficial in terms of health and quality of life (7,11-24). In mobile vertebral necrosis cases, regardless of the plana or non-plana morphology, given the pseudarthrosis capacity for reduction by positioning the spine in hyperextension, we usually perform armed kyphoplasty with expansive intravertebral implants. Initially, we carry out the pseudarthrosis region removal and adequate resection of the body’s interior through a percutaneous transpedicular approach. In these cases we usually apply expansive intravertebral stent implants and fill them with polymethylmethacrylate cement, allowing for great resistance of the metal associated with bone cement (it simulates the concept of construction industry’s reinforced concrete). Adjacent pedicle instrumentation would aim to reduce the loads on the affected posterior wall of the vertebra, minimizing the risk of its retropulsion (Figure 2).
In conclusion, this is a clinical case of unusual favorable evolution of vertebral pseudarthrosis, which, however, is very useful for confirming the prolonged duration and intensity of symptoms in the face of conservative treatment for this disease. This case report does not intend to withdraw early surgical indication for this pathology. On the contrary, it confirms its relevance. Nevertheless, it also proves that it is possible to achieve success in this pathology through conservative treatment. It is a recent proof of the efficacy of conservative treatment concerning vertebral pseudarthrosis, even in thoracolumbar transition region and with a large intravertebral cleft. This fills a gap in the literature, which, to date, has only focused on surgical treatment for this condition. In our opinion, conservative treatment can be a successful option for high surgical-risk patients or for those who refuse surgery. It is possible, with long-term use of a Jewett-type brace, to obtain self-stabilization and bone healing of a necrotic and clefted vertebra pseudarthrosis, with almost complete symptomatic relief.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://dx.doi.org/10.21037/jss-21-58
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/jss-21-58). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Maldague BE, Noel HM, Malghem JJ. The intravertebral vacuum cleft: a sign of ischemic vertebral collapse. Radiology 1978;129:23-9. [Crossref] [PubMed]
- McKiernan F, Faciszewski T. Intravertebral clefts in osteoporotic vertebral compression fractures. Arthritis Rheum 2003;48:1414-9. [Crossref] [PubMed]
- Hasegawa K, Homma T, Uchiyama S, et al. Vertebral pseudarthrosis in the osteoporotic spine. Spine (Phila Pa 1976) 1998;23:2201-6. [Crossref] [PubMed]
- McKiernan F, Jensen R, Faciszewski T. The dynamic mobility of vertebral compression fractures. J Bone Miner Res 2003;18:24-9. [Crossref] [PubMed]
- Young WF, Brown D, Kendler A, et al. Delayed post-traumatic osteonecrosis of a vertebral body (Kummell's disease). Acta Orthop Belg 2002;68:13-9. [PubMed]
- Benedek TG, Nicholas JJ. Delayed traumatic vertebral body compression fracture; part II: pathologic features. Semin Arthritis Rheum 1981;10:271-7. [Crossref] [PubMed]
- Lane JI, Maus TP, Wald JT, et al. Intravertebral clefts opacified during vertebroplasty: pathogenesis, technical implications, and prognostic significance. AJNR Am J Neuroradiol 2002;23:1642-6. [PubMed]
- Freyd M. The graphic rating scale. J Educ Psychol 1923;43:83-102. [Crossref]
- Vaccaro AR, Oner C, Kepler CK, et al. AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976) 2013;38:2028-37. [Crossref] [PubMed]
- Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976) 2000;25:2940-52; discussion 2952. [Crossref] [PubMed]
- Kim DY, Lee SH, Jang JS, et al. Intravertebral vacuum phenomenon in osteoporotic compression fracture: report of 67 cases with quantitative evaluation of intravertebral instability. J Neurosurg 2004;100:24-31. [PubMed]
- Jang JS, Kim DY, Lee SH. Efficacy of percutaneous vertebroplasty in the treatment of intravertebral pseudarthrosis associated with noninfected avascular necrosis of the vertebral body. Spine (Phila Pa 1976) 2003;28:1588-92. [Crossref] [PubMed]
- Peh WC, Gelbart MS, Gilula LA, et al. Percutaneous vertebroplasty: treatment of painful vertebral compression fractures with intraosseous vacuum phenomena. AJR Am J Roentgenol 2003;180:1411-7. [Crossref] [PubMed]
- Ha KY, Lee JS, Kim KW, et al. Percutaneous vertebroplasty for vertebral compression fractures with and without intravertebral clefts. J Bone Joint Surg Br 2006;88:629-33. [Crossref] [PubMed]
- Nakamae T, Fujimoto Y, Yamada K, et al. Efficacy of Percutaneous Vertebroplasty in the Treatment of Osteoporotic Vertebral Compression Fractures with Intravertebral Cleft. Open Orthop J 2015;9:107-13. [Crossref] [PubMed]
- Nieuwenhuijse MJ, van Rijswijk CS, van Erkel AR, et al. The intravertebral cleft in painful long-standing osteoporotic vertebral compression fractures treated with percutaneous vertebroplasty: diagnostic assessment and clinical significance. Spine (Phila Pa 1976) 2012;37:974-81. [Crossref] [PubMed]
- Nakamae T, Fujimoto Y, Yamada K, et al. Percutaneous vertebroplasty for osteoporotic vertebral compression fracture with intravertebral cleft associated with delayed neurologic deficit. Eur Spine J 2013;22:1624-32. [Crossref] [PubMed]
- Wu AM, Lin ZK, Ni WF, et al. The existence of intravertebral cleft impact on outcomes of nonacute osteoporotic vertebral compression fractures patients treated by percutaneous kyphoplasty: a comparative study. J Spinal Disord Tech 2014;27:E88-93. [Crossref] [PubMed]
- Wang G, Yang H, Chen K. Osteoporotic vertebral compression fractures with an intravertebral cleft treated by percutaneous balloon kyphoplasty. J Bone Joint Surg Br 2010;92:1553-7. [Crossref] [PubMed]
- Chen B, Fan S, Zhao F. Percutaneous balloon kyphoplasty of osteoporotic vertebral compression fractures with intravertebral cleft. Indian J Orthop 2014;48:53-9. [Crossref] [PubMed]
- Xia YH, Chen F, Zhang L, et al. Percutaneous kyphoplasty treatment evaluation for patients with Kümmell disease based on a two-year follow-up. Exp Ther Med 2018;16:3617-22. [PubMed]
- Park SJ, Kim HS, Lee SK, et al. Bone Cement-Augmented Percutaneous Short Segment Fixation: An Effective Treatment for Kummell's Disease? J Korean Neurosurg Soc 2015;58:54-9. [Crossref] [PubMed]
- Premat K, Vande Perre S, Cormier É, et al. Vertebral augmentation with the SpineJack® in chronic vertebral compression fractures with major kyphosis. Eur Radiol 2018;28:4985-91. [Crossref] [PubMed]
- Distefano D, Scarone P, Isalberti M, et al. The 'armed concrete' approach: stent-screw-assisted internal fixation (SAIF) reconstructs and internally fixates the most severe osteoporotic vertebral fractures. J Neurointerv Surg 2021;13:63-8. [Crossref] [PubMed]
- Cho Y. Corpectomy and circumferential fusion for advanced thoracolumbar Kümmell's disease. Musculoskelet Surg 2017;101:269-74. [Crossref] [PubMed]
- Uchida K, Kobayashi S, Matsuzaki M, et al. Anterior versus posterior surgery for osteoporotic vertebral collapse with neurological deficit in the thoracolumbar spine. Eur Spine J 2006;15:1759-67. [Crossref] [PubMed]


