
Hanging radiograph in idiopathic scoliosis patients: significance as a preoperative stress X-ray
Introduction
Before corrective surgery for idiopathic scoliosis, stress X-rays are indispensable to collect information regarding the reducibility of deformity, deciding fusion levels, and categorizing curve types and so on. Various types of stress X-rays to evaluate the spinal flexibility in patients with scoliosis have been reported in the past (1-16).
In previous report, the hanging radiograph was utilized in evaluating the spinal flexibility in patients with idiopathic scoliosis scheduled Osaka Medical College (OMC) brace treatment (17). The side-bending and the traction radiographs are usually performed and seem to be useful to estimate the amount of curve correction before surgery, however, the hanging radiograph has not been conducted preoperatively so far as known.
The objective of this study was to investigate retrospectively the significance of the hanging radiograph for prediction of the curve correction with surgical procedure by comparing with the side-bending and the traction radiographs.
We present the following article in accordance with the STROBE reporting checklist (available at https://dx.doi.org/10.21037/jss-21-74).
Methods
The subjects enrolled in this study were 22 cases of idiopathic scoliosis who performed posterior instrumentation and fusion by ISOLA method between 2008 and 2014. They included 2 males and 20 females, ranging in age from 11 years 5 months to 28 years 7 months, with a mean age of 16 years and 8 months. The curve types by Lenke classification were type 1 in 20 cases, type 2 in 1 case, and type 3 in 1 case. All these patients were preoperatively evaluated the flexibility of curves by the side-bending, the traction, and the hanging radiographs under the supervision of the first author on the same day.
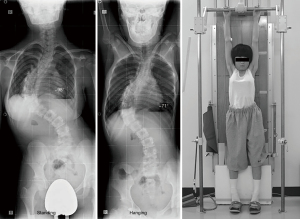
The side-bending radiograph was completed with the patient voluntarily bending maximally while in a supine position. The traction radiograph was obtained through applying maximally tolerable manual distraction force by the first author to stretch the spine using a standard cervical traction halter with a second individual holding the patient’s ankles in a supine position. The hanging radiograph was taken in position that the patient was hanging onto the bar, stretching the back, and touching the toes lightly to the floor not to sway the body after instructed exerting greatly to stretch the back as much as possible (Figure 1) (17).
We investigated the correction rates of main thoracic curves in side-bending, traction, and hanging positions and compared them with the correction rates after surgery that were collected within 3 months postoperatively. In addition, correction indices were also calculated and compared among these stress X-rays.
Cobb angles were manually measured on main thoracic curves using the standard technique. Correction rates and correction indices were calculated using the following formulas.
Statistical analysis was performed using two-tailed paired t-test and Pearson’s correlation coefficient. A P value of <0.05 was considered to be statistically significant.
We obtained written informed consent from the patients and their guardians for publication of this report and any accompanying images. Further, all procedures performed in this study were in accordance with the Helsinki declaration (as revised in 2013).
This research has been approved by the IRB of the authors’ affiliated institution (IRB No. 30-07).
Results
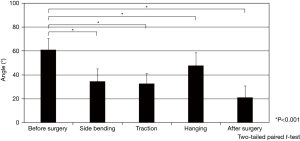
The average preoperative Cobb angle of main thoracic curves was 61.1°±9.3°. It was corrected with surgery to 21.3°±9.5°, and the stress X-rays by way of side-bending, traction, and hanging positions to 34.6°±10.4°, 32.7°±8.5°, and 47.7°±10.6°, respectively (Figure 2).
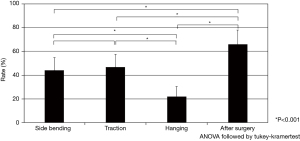
The mean correction rate after surgery was 65.9% that was statistically higher than those in side-bending (44.2%), traction (46.6%), and hanging (22.1%) positions (Figure 3). There were statistical correlations between the correction rates after surgery and in side-bending position (R=0.73) and those after surgery and in traction position (R=0.57). However, there was no statistical correlation between the correction rates after surgery and in hanging position (R=−0.01) (Figure 4).

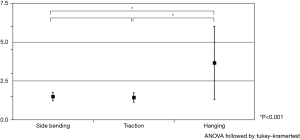
The correction indices of side-bending, traction, and hanging positions were 1.51, 1.45, and 3.67, respectively. The correction index in hanging position was statistically higher than those in side-bending and traction positions (Figure 5).
Discussion
The assessment of the spine flexibility has been conventionally implemented by use of the side-bending radiograph obtained with the patient in the supine or standing position (1). In addition, the push-prone radiograph in which the examiner applies manual pressure on the apices of the curve (2,3), the fulcrum-bending radiograph which is made with patient lying on his or her side over a large radiolucent plastic cylinder (4-6), the supine traction radiograph which is obtained by applying traction force using a standard cervical traction halter with a second individual applying countertraction on both lower extremities (7,8), the cervical suspension radiograph after application of a traction force corresponding to 30% of the patient’s body weight through a standard cervical traction head halter (9), and the axillary suspension radiograph which was taken in lifting position by a axillary harness to create a spinal traction force resulting from the patient’s own weight (10) have been reported as the stress X-rays to estimate the spinal flexibility in patients with idiopathic scoliosis. Further, general anesthesia is employed by some surgeons to take the supine traction radiograph for evaluation of maximum curve flexibility just before surgery (11-13). After advent of the EOS system, Hirsch et al. (14,15) utilized it to record the cervical suspension and the side-bending images in upright position and demonstrated that they showed similar results in classic supine position with seven and five times less radiation exposure, respectively. Recently, Ceyhan et al. (16) introduced a new piece of equipment; an electric traction table (ETT) that can apply simultaneously longitudinal traction and lateral pushing forces to the patient and predict the balance of the corrected body for choosing selective fusion levels. In a systematic review, Khodaei et al. (18) reported that the supine side-bending technique was the most practically used to assess the spinal flexibility but the fulcrum-bending technique was the most accurate in predicting post-operative correction among different radiographic methods.
It has been previously reported that the hanging radiograph is taking for the idiopathic scoliosis patients to assess if an appropriate correction by OMC brace is attained before prescription (17). The Cobb angle in hanging position were approximately correlated with the Cobb angle on OMC brace wearing independent of curve patterns, except some curves in multiple curve patterns, and were useful confirming adequate correction by OMC brace (17).
Advantages of the hanging radiograph are as follows: it is easily taken in outpatient clinic without any expensive equipment, extra-time, and extra-workforce, the target angle corrected by OMC bracing can be estimated, and the condition of traction force remains relatively steady because it depends just on the patient’s own weight. By contrast, disadvantages of it are as follows: it is insusceptible to take for the patients who cannot hang onto the bar, the force direction applied by this technique is just longitudinal which is not same as corrective force of OMC brace and corrective surgery by ISOLA method, and this technique is not applicable to some curves in multiple curve patterns (17).
In the current study, we investigated the significance of the hanging radiograph for preoperative evaluation of posterior instrumentation and fusion by ISOLA method. As a result, the correction rates of the side-bending and the traction radiographs seem to be useful anew to predict the amount of curve correction before surgery. Whereas, the hanging radiograph did not have any significance as preoperative evaluation at all.
The spinal flexibility is influenced by various factors, such as age, gender, apex level, number of involved vertebrae besides curve magnitude. Further, the optimal stress X-ray is suspected to be different in each case. Watanabe et al. (19) generally provided that the traction radiographs have a superior corrective ability than the side-bending radiographs in main and proximal thoracic curves, whereas the side-bending radiographs have a superior corrective ability than the traction radiographs in thoracolumbar and lumbar curves from their prospective clinical and radiologic study of adolescent idiopathic scoliosis. He et al. (20) reported that curve magnitude and location are two important parameters in selecting appropriate technique for the spinal flexibility assessment and the treatment effect prediction. They advocated that the traction technique should be considered for the patient with severe curves, while the side-bending technique is suggested for the patients with moderate curves, and then the fulcrum-bending technique is recommended to assess thoracic curve flexibility, whereas the side-bending technique is for the assessment of thoracolumbar/lumbar curve flexibility. Accordingly, the adoption of the favorable stress X-rays for each patient must be desirable for the scrupulous preoperative planning to obtain ideal and well-balanced correction of scoliosis.
This study included a couple of limitations. First, this is a retrospective observational study. Second, multiple types of curve pattern were evaluated together. Third, the number of patients was relatively small. Forth, the stress conditions applied by all three different positions were not always standardized. This was an unavoidable issue in current study. Despite these drawbacks, we would emphasize that our study will make a contribution to some advancement for the future management of AIS because accumulation of such minor data based on clinical experiences from a large number of institutions must be imperative to the future solution of issues regarding the outcome of surgery for AIS.
Conclusions
The correction rates in side-bending and traction positions seem to be useful to estimate the amount of curve correction before surgery. In the meanwhile, that in hanging position did not have any significance as preoperative evaluation.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://dx.doi.org/10.21037/jss-21-74
Data Sharing Statement: Available at https://dx.doi.org/10.21037/jss-21-74
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/jss-21-74). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This research has been approved by the IRB of the authors’ affiliated institution (IRB No. 30-07). We obtained written informed consent from the patients and their guardians for publication of this report and any accompanying images. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Vaughan JJ, Winter RB, Lonstein JE. Comparison of the use of supine bending and traction radiographs in the selection of the fusion area in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 1996;21:2469-73. [Crossref] [PubMed]
- Kleinman RG, Csongradi JJ, Rinksy LA, et al. The radiographic assessment of spinal flexibility in scoliosis: a study of the efficacy of the prone push film. Clin Orthop Relat Res 1982;47-53. [Crossref] [PubMed]
- Vedantam R, Lenke LG, Bridwell KH, et al. Comparison of push-prone and lateral-bending radiographs for predicting postoperative coronal alignment in thoracolumbar and lumbar scoliotic curves. Spine (Phila Pa 1976) 2000;25:76-81. [Crossref] [PubMed]
- Cheung KM, Luk KD. Prediction of correction of scoliosis with use of the fulcrum bending radiograph. J Bone Joint Surg Am 1997;79:1144-50. [Crossref] [PubMed]
- Luk KD, Cheung KM, Lu DS, et al. Assessment of scoliosis correction in relation to flexibility using the fulcrum bending correction index. Spine (Phila Pa 1976) 1998;23:2303-7. [Crossref] [PubMed]
- Luk KD, Don AS, Chong CS, et al. Selection of fusion levels in adolescent idiopathic scoliosis using fulcrum bending prediction: a prospective study. Spine (Phila Pa 1976) 2008;33:2192-8. [Crossref] [PubMed]
- Kirk KL, Kuklo TR, Polly DW Jr. Traction versus side-bending radiographs: is the proximal thoracic curve the stiffer curve in double thoracic curves? Am J Orthop (Belle Mead NJ) 2003;32:284-8. [PubMed]
- Polly DW Jr, Sturm PF. Traction versus supine side bending. Which technique best determines curve flexibility? Spine (Phila Pa 1976) 1998;23:804-8. [Crossref] [PubMed]
- Büchler P, de Oliveria ME, Studer D, et al. Axial suspension test to assess pre-operative spinal flexibility in patients with adolescent idiopathic scoliosis. Eur Spine J 2014;23:2619-25. [Crossref] [PubMed]
- Lamarre ME, Parent S, Labelle H, et al. Assessment of spinal flexibility in adolescent idiopathic scoliosis: suspension versus side-bending radiography. Spine (Phila Pa 1976) 2009;34:591-7. [Crossref] [PubMed]
- Davis BJ, Gadgil A, Trivedi J, et al. Traction radiography performed under general anesthetic: a new technique for assessing idiopathic scoliosis curves. Spine (Phila Pa 1976) 2004;29:2466-70. [Crossref] [PubMed]
- Hamzaoglu A, Talu U, Tezer M, et al. Assessment of curve flexibility in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2005;30:1637-42. [Crossref] [PubMed]
- Ibrahim T, Gabbar OA, El-Abed K, et al. The value of radiographs obtained during forced traction under general anaesthesia in predicting flexibility in idiopathic scoliosis with Cobb angles exceeding 60 degree. J Bone Joint Surg Br 2008;90:1473-6. [Crossref] [PubMed]
- Hirsch C, Ilharreborde B, Mazda K. EOS suspension test for the assessment of spinal flexibility in adolescent idiopathic scoliosis. Eur Spine J 2015;24:1408-14. [Crossref] [PubMed]
- Hirsch C, Ilharreborde B, Mazda K. Flexibility analysis in adolescent idiopathic scoliosis on side-bending images using the EOS imaging system. Orthop Traumatol Surg Res 2016;102:495-500. [Crossref] [PubMed]
- Ceyhan E, Delialioglu OM, Bayrakci K, et al. The Usefulness of Employing an Electronic Traction Table to Determine Flexibility in Adolescent Idiopathic Scoliosis. Turk Neurosurg 2017;27:245-51. [PubMed]
- Kuroki H, Inomata N, Hamanaka H, et al. Significance of hanging total spine X-ray to estimate the indicative correction angle by brace wearing in idiopathic scoliosis patients. Scoliosis 2012;7:8. [Crossref] [PubMed]
- Khodaei M, Pachêco-Pereira C, Trac S, et al. Radiographic methods to estimate surgical outcomes based on spinal flexibility assessment in patients who have adolescent idiopathic scoliosis: A systematic review. Spine J 2018;18:2128-39. [Crossref] [PubMed]
- Watanabe K, Kawakami N, Nishiwaki Y, et al. Traction versus supine side-bending radiographs in determining flexibility: what factors influence these techniques? Spine (Phila Pa 1976) 2007;32:2604-9. [Crossref] [PubMed]
- He C, Wong MS. Spinal Flexibility Assessment on the Patients With Adolescent Idiopathic Scoliosis: A Literature Review. Spine (Phila Pa 1976) 2018;43:E250-8. [Crossref] [PubMed]


