
Epidemiology of symptomatic ossification of the posterior longitudinal ligament: a nationwide registry survey
Introduction
Ossification of the posterior longitudinal ligament (OPLL) is a type of heterotopic bone formation that can cause neurological damage (1). Previous radiographic studies have shown that approximately 3% of the Japanese population have OPLL that is detectable by plain radiography (2). Recent computed tomography (CT) studies have revealed that detectable OPLL is present in 1.3% of Americans of European ancestry and 6% of Japanese people (3,4).
These radiographic studies have revealed that many individuals have latent OPLL that does not induce myelopathy. It is currently unknown how many patients suffer from neurological symptoms due to OPLL.
OPLL has been designated as an intractable disease in Japan according to the Outline of Intractable Disease Measures since 1980 (5-7). According to this system, patients with symptomatic OPLL are registered in a national registry and are provided with a subsidy for treatment of the disease (7). Recently, these registry data have been made accessible to researchers. The purpose of this study was to investigate the prevalence of symptomatic and asymptomatic OPLL and the characteristics of patients with symptomatic OPLL. We present the following article in accordance with the STROBE reporting checklist (available at https://dx.doi.org/10.21037/jss-21-78).
Methods
We applied to the Intractable/Rare Disease Control Division of the Health Service Bureau at the Japanese Ministry of Health, Labor and Welfare for access to data from the clinical records of OPLL patients. Clinical records dating from January 1, 2011 to December 31, 2012 were provided on the condition that personal information would be protected. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional ethics board of the Japan Community Healthcare Organization, Osaka Hospital (IRB 2018-52), and the requirement for individual consent for this retrospective analysis was waived.
Japan’s system of medical registries and subsidies, as it relates to OPLL, is shown in Figure 1 (6). In keeping with national policy, the Japanese Ministry of Health, Labor and Welfare provides financial support for patients who suffer from intractable diseases with unknown cause and no established treatment (5-7). As of 2012, when the data used in this study were collected, 56 diseases were designated as intractable. Several other studies have been performed using registry data for intractable diseases such as idiopathic pulmonary fibrosis (8), moyamoya disease (9), and multiple systemic atrophy (10).
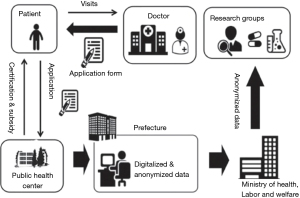
A patient with symptoms suggestive of OPLL, such as neck pain, numbness, clumsiness, radicular pain, or gait disturbance, first visits a physician, who examines the patient and diagnoses OPLL based on neurological signs and imaging tests (of which simple X-rays are standard). If ossification is difficult to see on X-rays, an MRI or CT can be performed. As a rule, the registry is intended to enroll OPLL patients with neurological symptoms such as myelopathy. Physicians will not enroll patients in the registry with no neurological symptoms or only a small ossification that cannot be seen on X-rays. The physician fills out an application form (known as the clinical record) and gives this form to the patient along with an application for the medical expense subsidy. The patient then applies to the public health center in his or her prefecture for a certificate of medical subsidy. After the public health center checks the clinical record, the governor’s office issues a certificate of medical subsidy. The clinical record and certificate of medical subsidy are renewed annually. New patients are classified as “new-onset” clinical records, while patients renewing their certificates are classified as “renewal” clinical records. The clinical record contains the patient’s sex, age, claim date, prefecture of residence, year of birth, disability grade, employment status, Japanese Orthopedic Association (JOA) score for cervical myelopathy, radiographic findings, and history of surgery or planned future surgery.
These clinical records, created in print form, are digitized as Microsoft Excel files by each prefecture and then integrated into the Japanese Ministry of Health, Labor and Welfare records. These data are then provided to researchers. In some prefectures, the digitization of clinical records has not been fully completed due to a shortage of workers. The mean rate of digitization of clinical records among the prefectures is approximately 70% (6,11). Regardless of the digitization backlog, however, a certificate of medical subsidy is issued to the patient as soon as the application is processed in print form. The present study’s data on medical subsidy certificates were complemented by other publicly available data on the Census and Statistics Department website (12).
Disability grades
Patients with OPLL are graded according to the severity of their disability. “First-grade disability” means that patients cannot maintain a sitting position due to disturbance in trunk function. “Second-grade disability” implies that patients are unable to walk. “Third-grade disability” means that patients have difficulty walking.
Statistical analysis
Student’s t-test was used to compare clinical outcomes between the new-onset group and the renewal group. The chi-square test was used to compare categorical data. A P value less than 0.05 (two-tailed) was considered statistically significant. The statistical analysis was performed with SPSS Statistics software (version 20; IBM, Armonk, NY, USA).
Results
Patients with certificates of medical subsidy
The number of patients with certificates of medical subsidy for symptomatic OPLL was 35,070 in 2011 and 33,346 in 2012 (Table 1). The mean number of patients with certificates of medical subsidy was therefore 34,208 per year (23,016 men and 11,192 women). The total population of Japan, according to the 2012 national census, was 125,957,000 (61,328,000 men and 64,630,000 women). The period prevalence of symptomatic OPLL, based on the number of certificates of medical subsidy, was therefore 0.027% (0.037% in men and 0.017% in women).
Table 1
| Patients with certificates of medical benefit for OPLL | Patients whose digitized clinical records were available | Availability rate | |||
|---|---|---|---|---|---|
| New-onset | Renewal | Total | |||
| Numbers of patients in 2011 | 35,070 (23,584) | 4,645 (3,389) | 20,054 (13,300) | 24,699 (16,689) | 70 |
| Numbers of patients in 2012 | 33,346 (22,447) | 4,806 (3,497) | 20,550 (13,699) | 25,356 (17,196) | 76 |
| Means of the 2011 and 2012 values | 34,208 (23,016) | 4,726 (3,443) | 20,302 (13,500) | 25,028 (16,943) | 73 |
Numbers in parentheses indicate male sex. OPLL, ossification of the posterior longitudinal ligament.
Clinical records
Among the 34,208 patients per year with certificates of medical subsidy, 25,028 patients per year (73%) had digitized clinical records available. There were 4,726 new-onset patients per year (9,451 patients over the two years) and 20,302 renewal patients per year (40,604 patients over the two years).
New-onset group
Table 2 shows the demographic details of the new-onset patients whose clinical records were available. Among the 9,451 new-onset patients, there were 6,886 males (73%) and 2,565 females (27%). Figure 2 shows their age distribution; the mean age of new-onset patients was 65±12 years. Patients in their 60s constituted the largest age group (32%), followed by those in their 70s (28%). The mean time from onset to diagnosis was 2.6±5.5 years.
Table 2
| New-onset | Renewal | P value | |
|---|---|---|---|
| Total number of patients in 2011–2012 | 9,451 | 40,604 | N/A |
| Male | 6,886 | 26,999 | N/A |
| Female | 2,565 | 13,605 | N/A |
| Male/female ratio | 2.7 | 2.0 | <0.001 |
| Age (yrs) | 65±12 | 70±11 | <0.001 |
| Time course from disease onset (yrs) | 2.6±5.5 | 9.7±8.7 | <0.001 |
| JOA subscores/possible points | |||
| Upper extremity motor function/4 | 2.3±1.1 | 2.4±1.1 | <0.001 |
| Lower extremity motor function/4 | 2.0±1.2 | 1.8±1.1 | <0.001 |
| Upper extremity sensory function/2 | 0.8±0.7 | 0.9±0.7 | <0.001 |
| Lower extremity sensory function/2 | 1.0±0.7 | 0.9±0.7 | <0.001 |
| Trunk sensory function/2 | 1.4±0.7 | 1.3±0.7 | <0.001 |
| Bladder function/3 | 2.3±0.9 | 2.2±0.9 | <0.001 |
| Total/17 | 9.8±3.6 | 9.4±3.6 | <0.001 |
| Employment status, n [%] | |||
| Paid work | 2,850 [30] | 6,620 [16] | <0.001 |
| Housework | 1,678 [18] | 7,172 [18] | 0.8 |
| In-home care | 2,285 [24] | 18,955 [47] | <0.001 |
| Inpatient | 1,605 [17] | 1,888 [5] | <0.001 |
| Nursing home | 72 [1] | 1,163 [3] | <0.001 |
| Grade of disability, n [%] | |||
| First grade | 147 [1.6] | 3861 [9.5] | <0.001 |
| Second grade | 158 [1.7] | 4619 [11] | <0.001 |
| Third grade | 129 [1.4] | 3060 [7.5] | <0.001 |
| Fourth grade | 137 [1.4] | 1433 [3.5] | <0.001 |
| Fifth grade | 58 [0.6] | 919 [2.2] | <0.001 |
N/A, not applicable; JOA, Japanese Orthopedic Association; OPLL, ossification of the posterior longitudinal ligament.
Figure 3 shows the distribution of JOA scores. The mean JOA score among new-onset patients was 9.8 out of 17 possible points (Table 2). Patients with 11 points constituted the largest group (11%), followed by those with 10 (11%) and 12 (10%) points. When focusing only on cervical spine surgery patients, the mean JOA score was 9.7. The distribution of scores for this subgroup remained unchanged, with 11 being the most common score.
As for employment status, 30% of the patients had paid work, 18% were homemakers, 24% were being cared for at home, and 17% were inpatients (Table 2). As for disability grade, there were 129 new-onset patients (1.4%) in the third grade, 158 (1.7%) in the second grade, and 147 (1.6%) in the first grade. The remaining large majority of new-onset patients were not considered disabled.
Table 3 shows the location of ossification as revealed through radiography. Cervical OPLL was found in 8,067 new-onset patients (85%), thoracic OPLL in 799 (8%), and lumbar OPLL in 514 (5%) (Table 3).
Table 3
| New-onset | Renewal | P value | |
|---|---|---|---|
| Cervical OPLL [%] | 8,067 [85]* | 30,600 [75]† | <0.001 |
| Thoracic OPLL [%] | 799 [8]* | 5,203 [13]† | <0.001 |
| Lumbar OPLL [%] | 514 [5]* | 3,092 [8]† | <0.001 |
| Cervical OLF [%] | 137 [1]* | 670 [1]† | 0.2 |
| Thoracic OLF [%] | 806 [6]* | 5,313 [9]† | <0.001 |
| Lumbar OLF [%] | 225 [2.3]* | 1,693 [4]† | <0.001 |
* and †, the total number of radiographic findings is higher than the total number of patients because some patients had multiple lesions. OPLL, ossification of the posterior longitudinal ligament; OLF, ossification of the ligamentum flavum.
Table 4 shows the surgical data. A total of 7,928 new-onset patients (84%) had undergone surgery. Among these, 6,135 patients (64%) had undergone posterior cervical surgery, 858 (9%) had undergone anterior cervical surgery, 598 (6%) had undergone posterior thoracic surgery, 49 (0.5%) had undergone anterior thoracic surgery, 278 (3%) had undergone posterior lumbar surgery, and 10 (0.1%) had undergone anterior lumbar surgery.
Table 4
| New-onset | Renewal | P value | |
|---|---|---|---|
| Total number of surgeries [%] | 7,928 [84]* | 36,266 [89]† | <0.001 |
| Posterior cervical surgery [%] | 6,135 [64]* | 25,819 [64]† | 0.02 |
| Anterior cervical surgery [%] | 858 [9]* | 4,280 [11]† | <0.001 |
| Posterior thoracic surgery [%] | 598 [6]* | 4,097 [10]† | <0.001 |
| Anterior thoracic surgery [%] | 49 [0.5]* | 651 [1.6]† | <0.001 |
| Posterior lumbar surgery [%] | 278 [3]* | 1,353 [3]† | 0.05 |
| Anterior lumbar surgery [%] | 10 [0.1]* | 66 [0.2]† | 0.04 |
| Thoracic surgery + Cervical surgery [%] | 332 [4]* | 2,953 [7.3]† | <0.001 |
* and †, The total number of surgeries is higher than the total number of patients because some patients had multiple surgeries.
Renewal group
Among the 40,604 renewal patients there were 26,999 men (66%) and 13,605 women (34%). Figure 4 shows their age distribution; the mean age of renewal patients was 70±11 years. Patients in their 70s constituted the largest age group (37%), followed by those in their 60s (29%). The mean time from disease onset to the most recent follow-up was 9.7±8.7 years.
Figure 5 shows the distribution of JOA scores. The mean JOA score among renewal patients was 9.4 out of 17 possible points (Table 2). Patients with 11 points constituted the largest group (11%), followed by those with 10 points (11%).
As for employment status, 16% of renewal patients had paid work, 18% were homemakers, 47% were being cared for at home, 5% were inpatients, and 3% were in a nursing home. As for disability grade, there were 3,060 renewal patients (7.5%) in the third grade, 4,619 (11%) in the second grade, and 3,861 (9.5%) in the first grade.
Table 3 shows the location of ossification as revealed through radiography. Cervical OPLL was found in 30,600 renewal patients (75%), thoracic OPLL in 5,203 (13%), and lumbar OPLL in 3,092 (8%).
Table 4 shows the surgical data. A total of 36,266 renewal patients (89%) had undergone surgery. Among these, 25,819 (64%) had undergone posterior cervical surgery, 4,280 (11%) had undergone anterior cervical surgery, 4,097 (10%) had undergone posterior thoracic surgery, 651 (1.6%) had undergone anterior thoracic surgery, 1,353 (3%) had undergone posterior lumbar surgery, and 66 (0.2%) had undergone anterior lumbar surgery.
Comparison of clinical data between new-onset patients and renewal patients
Mean age was significantly higher among the renewal patients than the new-onset patients (P<0.001). The time from disease onset was significantly longer among the renewal patients than the new-onset patients (P<0.001) (Table 2). Renewal patients had significantly higher proportions of thoracic OPLL and posterior thoracic surgery compared to new-onset patients (P<0.001).
Discussion
To the best of our knowledge, this is the largest epidemiologic study of OPLL to date. In 2011 and 2012, there were 34,208 patients with symptomatic OPLL per year in Japan, indicating a period prevalence of 0.027% overall. Notably, the period prevalence was twice as high in men as in women. The onset of symptoms was highest when patients were in their 60s. Patients with symptomatic OPLL suffered severe neurological damage on average, with a mean JOA score of 9 points. Twenty percent of renewal patients had a first- or second-grade disability associated with OPLL. A JOA score of 11 points was the most common indication for the first surgery, and 86% of surgeries were performed posteriorly. As for incidence, based on the available clinical records, there were 4,726 new-onset patients per year. Considering that the digitization rate of clinical records was 73%, however, we estimate that approximately 6,474 patients develop new symptomatic OPLL each year. The incidence of symptomatic OPLL was 0.005% (5 per 100,000 population). The prevalence of symptomatic OPLL is therefore much lower than the previously reported rates of radiographically detectable OPLL (2).
CT has become an increasingly common modality for detecting OPLL (3,4,13-17). In a previous study in which we examined whole-spine CT scans of 1,500 healthy Japanese people, the rate of CT-detectable ossification was 6.3% in the cervical region and 1.6% in the thoracic region (4). However, this radiographic study was limited because the presence or absence of neurological symptoms in these subjects was unknown. To date there have been no data showing how many OPLL patients are sufficiently symptomatic to require surgery. Our present data demonstrate that the number of patients who require surgery for OPLL is much smaller than the number of patients with radiographically detectable OPLL. These results suggest that most cases of radiographically detectable OPLL are low-symptomatic or asymptomatic. Indeed, there may be hundreds of radiographically detectable OPLL cases for every case that produces symptoms like myelopathy.
There have been no previous studies examining the incidence of symptomatic OPLL in Japan, but a nationwide database (National Health Insurance Database) study on this topic has been performed in Taiwan (18). Those researchers found that the incidence of OPLL-related admission was 0.6 per 100,000 people (18). These data and ours support the notion that symptomatic OPLL is a rare disease.
With the advancement of diagnostic imaging techniques, the number of patients with incidentally discovered OPLL is increasing. In the absence of data on the incidence of symptoms in OPLL, patients may become unnecessarily anxious upon learning that they have OPLL. However, our data suggest that patients with incidentally discovered OPLL are unlikely to require surgery or continued follow-up for this condition.
One reason why most radiographically detectable cases of OPLL are asymptomatic is that incidentally discovered OPLL tends to affect only a small portion of the ligament. Generally, myelopathy is caused by a complex combination of static compression and dynamic factors. Static compression is assessed according to the proportion of the width of the spinal canal that is occupied by OPLL. The mean proportion occupied by OPLL in patients who undergo surgery has been reported to range from 40% to 60% (19-23). In all patients with radiographically detected OPLL, in contrast, the mean proportion is 27% (4). Ossification occupying more than 40% of the spinal canal is rare in radiographically detected OPLL.
Patients with symptomatic OPLL were few in number, but they suffered from severe neurologic consequences. The mean JOA score of patients with symptomatic OPLL was 9 points. This score indicates that the average patient had moderate myelopathy, such as disturbance in gait and uncoordinated motor activity. Furthermore, 20% of the renewal group were first- or second-grade disabled, meaning that these patients were wheelchair-bound. There are several possible reasons for this high disability rate. First, the renewal patients tended to be older than the new-onset patients, and the improvements achieved through surgery for OPLL tend to fade after a few years (24). Second, the renewal patients tended to have more severe OPLL than the new-onset patients. Renewal patients had significantly higher rates of both cervical and thoracic OPLL than the new-onset patients, and thoracic OPLL is more difficult to treat than cervical OPLL. A multicenter study has reported that the rate of motor palsy as a postoperative complication is 32% after posterior surgery for thoracic OPLL (25).
The significantly lower JOA scores and inferior physical function in renewal patients compared to new-onset patients may suggest a problem with the current surgical treatment of OPLL. As mentioned earlier, the improvements achieved through surgery often peak a couple of years after surgery and then slowly diminish. The reasons for this are not well understood, but may include progression of ossification and decreased lordosis of the cervical spine (23). This may also be related to surgical approach, as the majority of surgeries for OPLL are laminoplasties from the posterior approach. A study comparing anterior decompression and fusion with laminoplasty reported an increase in JOA score over time in the anterior fusion group (26). Anterior fusion has been found to have more complications (21,26), however, and it was selected for only about 10% of the patients in the present cohort. On the other hand, posterior fusion is believed to yield improvements comparable to those of anterior fusion (27), and posterior fusion might be preferable to laminoplasty in terms of maintaining results over the long term.
There were some limitations to our study. One of these is that, because participating in the registration system and receiving a certificate of medical subsidy is not mandatory, there may be more patients with symptomatic OPLL in Japan who did not appear in our database. Some patients who have undergone surgery and recovered may choose to discontinue clinical follow-up and not renew their certificates. For new-onset patients, however, the registration rate is expected to be high. The existence of a medical subsidy system for OPLL is well known among both physicians and patients as it started more than 30 years ago. Patients have an economic incentive to apply for a certificate of medical subsidy because the subsidy covers their medical costs. In particular, patients who undergo surgery are highly likely to apply for the certificate of medical subsidy, because surgery costs are high. This is supported by the fact that 90% of the patients with a certificate of medical subsidy underwent surgery. Another limitation was that only about 73% of all clinical records have been digitized. Although we believe that a digitization rate of 73% is high enough that the digitized records accurately represent the other 27% of records, there might be some bias because the digitization rate was different among prefectures. After the Intractable Disease Health Care Act was revised in 2015, the paper form used to create clinical records was replaced with a form that can be automatically digitized by an optical character reader. Although the records from that era have yet to be disclosed to researchers, the digitization rate of clinical records will be higher in future studies.
Despite these limitations, we believe that there is no better source of information on the prevalence of symptomatic OPLL than the present registry system. Our data will be useful for future medical policy decisions. Patients with incidentally detected OPLL tend to have mild symptoms and little need for medical assistance. Once neurological symptoms appear, however, patients can develop severe symptoms, and early surgery is desirable. Decisions about whether to provide medical assistance should be based not only on imaging tests but also on neurological symptoms.
Conclusions
Based on the number of certificates of medical subsidy issued for OPLL, the incidence and the one-year period prevalence of symptomatic OPLL in Japan are 0.005% and 0.027%, respectively. This rate is less than one-hundredth of the rate of radiographically detected OPLL. This means that most radiographically detected OPLL cases are low-symptomatic or asymptomatic. On the other hand, although symptomatic OPLL is a rare disease, these patients suffer severe disability. These results will be useful for future medical policy decisions.
Acknowledgments
Chris Rowthorn provided professional English-language editing of this article.
Funding: This work was supported by a grant from the Japanese Ministry of Health, Labor and Welfare (201610008B).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://dx.doi.org/10.21037/jss-21-78
Data Sharing Statement: Available at https://dx.doi.org/10.21037/jss-21-78
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/jss-21-78). Drs. TF, TK and MI report that the grant is from the Japanese Ministry of Health, Labor and Welfare. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work and ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of the Japan Community Healthcare Organization, Osaka Hospital (IRB 2018-52) and the requirement for individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Okawa A, Matsumoto M, Iwasaki M, et al. OPLL. 3rd ed: Springer; 2020.
- Matsunaga S, Sakou T. Ossification of the posterior longitudinal ligament of the cervical spine: etiology and natural history. Spine (Phila Pa 1976) 2012;37:E309-14. [Crossref] [PubMed]
- Fujimori T, Le H, Hu SS, et al. Ossification of the posterior longitudinal ligament of the cervical spine in 3161 patients: a CT-based study. Spine (Phila Pa 1976) 2015;40:E394-403. [Crossref] [PubMed]
- Fujimori T, Watabe T, Iwamoto Y, et al. Prevalence, Concomitance, and Distribution of Ossification of the Spinal Ligaments: Results of Whole Spine CT Scans in 1500 Japanese Patients. Spine (Phila Pa 1976) 2016;41:1668-76. [Crossref] [PubMed]
-
Japan Intractable Diseases Information Center - Kanatani Y, Tomita N, Sato Y, et al. National Registry of Designated Intractable Diseases in Japan: Present Status and Future Prospects. Neurol Med Chir (Tokyo) 2017;57:1-7. [Crossref] [PubMed]
- Takemura S, Sone T. Research and development on intractable & rare diseases in Japan: Contribution of the National Institute of Public Health to research program management. J Natl Inst Public Health 2019;68:45-64.
- Natsuizaka M, Chiba H, Kuronuma K, et al. Epidemiologic survey of Japanese patients with idiopathic pulmonary fibrosis and investigation of ethnic differences. Am J Respir Crit Care Med 2014;190:773-9. [Crossref] [PubMed]
- Sato Y, Kazumata K, Nakatani E, et al. Characteristics of Moyamoya Disease Based on National Registry Data in Japan. Stroke 2019;50:1973-80. [Crossref] [PubMed]
- Sakushima K, Nishimoto N, Nojima M, et al. Epidemiology of Multiple System Atrophy in Hokkaido, the Northernmost Island of Japan. Cerebellum 2015;14:682-7. [Crossref] [PubMed]
- Matsuyama A, Akimaru H. Current status and utilization of the database of the designated intractable diseases 2018. Available online: https://www.mhlw.go.jp/stf/shingi2/0000193073.html
- e-Stat. Available online: https://www.e-stat.go.jp/
- Nishimura S, Nagoshi N, Iwanami A, et al. Prevalence and Distribution of Diffuse Idiopathic Skeletal Hyperostosis on Whole-spine Computed Tomography in Patients With Cervical Ossification of the Posterior Longitudinal Ligament: A Multicenter Study. Clin Spine Surg 2018;31:E460-5. [Crossref] [PubMed]
- Kawaguchi Y, Nakano M, Yasuda T, et al. Ossification of the posterior longitudinal ligament in not only the cervical spine, but also other spinal regions: analysis using multidetector computed tomography of the whole spine. Spine (Phila Pa 1976) 2013;38:E1477-82. [Crossref] [PubMed]
- Hirai T, Yoshii T, Nagoshi N, et al. Distribution of ossified spinal lesions in patients with severe ossification of the posterior longitudinal ligament and prediction of ossification at each segment based on the cervical OP index classification: a multicenter study (JOSL CT study). BMC Musculoskelet Disord 2018;19:107. [Crossref] [PubMed]
- Hirai T, Yoshii T, Iwanami A, et al. Prevalence and Distribution of Ossified Lesions in the Whole Spine of Patients with Cervical Ossification of the Posterior Longitudinal Ligament A Multicenter Study (JOSL CT study). PLoS One 2016;11:e0160117. [Crossref] [PubMed]
- Yoshii T, Hirai T, Iwanami A, et al. Co-existence of ossification of the nuchal ligament is associated with severity of ossification in the whole spine in patients with cervical ossification of the posterior longitudinal ligament -A multi-center CT study. J Orthop Sci 2019;24:35-41. [Crossref] [PubMed]
- Wu JC, Liu L, Chen YC, et al. Ossification of the posterior longitudinal ligament in the cervical spine: an 11-year comprehensive national epidemiology study. Neurosurg Focus 2011;30:E5. [Crossref] [PubMed]
- Matsuoka T, Yamaura I, Kurosa Y, et al. Long-term results of the anterior floating method for cervical myelopathy caused by ossification of the posterior longitudinal ligament. Spine (Phila Pa 1976) 2001;26:241-8. [Crossref] [PubMed]
- Iwasaki M, Kawaguchi Y, Kimura T, et al. Long-term results of expansive laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine: more than 10 years follow up. J Neurosurg 2002;96:180-9. [PubMed]
- Iwasaki M, Okuda S, Miyauchi A, et al. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: Part 2: Advantages of anterior decompression and fusion over laminoplasty. Spine (Phila Pa 1976) 2007;32:654-60. [Crossref] [PubMed]
- Iwasaki M, Okuda S, Miyauchi A, et al. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: Part 1: Clinical results and limitations of laminoplasty. Spine (Phila Pa 1976) 2007;32:647-53. [Crossref] [PubMed]
- Fujimori T, Iwasaki M, Okuda S, et al. Long-term results of cervical myelopathy due to ossification of the posterior longitudinal ligament with an occupying ratio of 60% or more. Spine (Phila Pa 1976) 2014;39:58-67. [Crossref] [PubMed]
- Kato Y, Iwasaki M, Fuji T, et al. Long-term follow-up results of laminectomy for cervical myelopathy caused by ossification of the posterior longitudinal ligament. J Neurosurg 1998;89:217-23. [Crossref] [PubMed]
- Imagama S, Ando K, Takeuchi K, et al. Perioperative Complications After Surgery for Thoracic Ossification of Posterior Longitudinal Ligament: A Nationwide Multicenter Prospective Study. Spine (Phila Pa 1976) 2018;43:E1389-97. [Crossref] [PubMed]
- Sakai K, Okawa A, Takahashi M, et al. Five-year follow-up evaluation of surgical treatment for cervical myelopathy caused by ossification of the posterior longitudinal ligament: a prospective comparative study of anterior decompression and fusion with floating method versus laminoplasty. Spine (Phila Pa 1976) 2012;37:367-76. [Crossref] [PubMed]
- Yoshii T, Sakai K, Hirai T, et al. Anterior decompression with fusion versus posterior decompression with fusion for massive cervical ossification of the posterior longitudinal ligament with a ≥50% canal occupying ratio: a multicenter retrospective study. Spine J 2016;16:1351-7. [Crossref] [PubMed]






