
Impact of human immunodeficiency virus on 2-year revision rates following lumbar fusion for degenerative spinal conditions: a retrospective cohort study
Introduction
The success of antiretroviral treatments has drastically improved the life expectancy of seropositive patients with human immunodeficiency virus (HIV) (1). As the population of patients with a diagnosis of HIV ages, these patients become more at risk of developing chronic conditions associated with older age, such as spinal degenerative disorders (2,3). For patients with degenerative spine conditions that fail conservative treatment, spinal arthrodesis is a successful treatment option. The incidence of HIV-positive patients undergoing spinal fusion has increased more than 3-fold over the past 10 years (4). Despite the significant increase in spinal surgery among HIV-positive patients (5), few studies exist that examine the impact of HIV status long term on surgical outcomes for degenerative spinal conditions.
Previous research on one-year outcomes in patients undergoing lumbar fusions show HIV positive patients have an increased risk for respiratory complications (OR 5.43; 95% CI: 3.40–8.67; P<0.001), wound complications (OR 2.60; 95% CI: 1.37–4.96; P=0.004), neurologic complications (OR 1.96; 95% CI: 1.04–3.73; P=0.039), and higher mortality rates (OR 39.91; 95% CI: 14.99–106.30; P<0.001) compared with non-HIV patients (6). HIV positive patients undergoing spinal surgery have worse short and long-term clinical outcomes, including higher rates of 30-day readmission (11.1% vs. 2.2%, P=0.04), one-year pseudoarthrosis (17.8% vs. 4.4%, P=0.02) and one-year infectious complication rate (13.3% vs. 3.3%, P=0.06) (7). While it is established that HIV-positive patients have a higher incidence of hospital mortality and complications (5), there are no studies that evaluate its effects on revision rates beyond one year in this specific cohort.
Patients with HIV have higher rates of risk factors associated with two-year spinal surgery revision such as low bone mineral density (BMD) (8), infection (7,9,10) and pseudoarthrosis (11). However, there are no long-term studies that evaluate whether these risk factors affect revision rates in HIV-positive patients undergoing elective lumbar fusions for degenerative spinal conditions. Patients with HIV have an increased risk of osteopenia and osteoporosis due to traditional risk factors that disproportionately affect HIV-infected individuals, such as Vitamin C deficiency and low body weight (8). Additionally, patients with HIV have low BMD due to alterations in bone metabolism caused by antiretroviral therapy (ART), HIV viral proteins and chronic inflammation (8). Patients with low BMD undergoing lumbar fusions have an elevated risk of postoperative complications that may require revision surgery—including pedicle screw loosening, nonunion, proximal junctional kyphosis, and adjacent segment fractures (12-16). Additionally, low BMD is associated with higher rates of two-year pseudarthrosis and revision surgery for non-HIV patients undergoing a single-level lumbar fusion for degenerative spondylolisthesis compared to patients with normal bone mineral densities (11).
Patients with a diagnosis of HIV have been previously shown to be at an increased risk of surgical site infection (SSI) after orthopedic procedures (OR 1.4; 95% CI: 0.5–3.8) (9,10). Infection increases the production of biologic inflammatory markers such as cyclooxygenase-2, interleukin-1β, and tumor necrosis factor-α, all of which suppress local bone growth and contribute to lack of arthrodesis (17). Non-HIV patients undergoing spinal fusion for degenerative thoracolumbar scoliosis who experience early SSI have an increased risk of failure and revision surgery, with time from SSI to removal of instrumentation at an average of 16 months (P=0.025) (18).
We performed a retrospective cohort study using past patient records from a national database to evaluate the effects of HIV-positive status, among asymptomatic patients and patients with acquired immunodeficiency syndrome (AIDS), on 2-year revision rates after primary lumbar fusion. We hypothesized that HIV-positive patients will have increased complication rates and worse post-surgical outcomes compared to the HIV negative cohort. Additionally, we predicted that there will be a higher infection rate within 90 days post-surgery in the HIV-positive cohort compared to the control cohort.
We present the following article in accordance with the STROBE reporting checklist (available at https://dx.doi.org/10.21037/jss-21-84).
Methods
Data source and collection
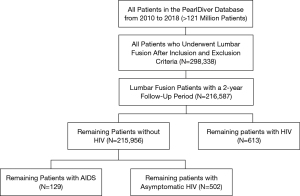
The PearlDiver Patient Records Database (www.pearldiverinc.com; 10435 Marble Creek Circle Colorado Springs, CO 80908) was used to perform a retrospective cohort analysis. The Mariner dataset was utilized, including all payer’s claim information for over 121 million patients from 2010–2019. Patients who underwent lumbar fusion were identified using International Classification of Diseases (ICD) procedure codes as well as Current Procedural Terminology (CPT) codes. Only patients who met the inclusion and exclusion criteria and who had at least a 2-year follow-up period after their initial operation were included in this study. The Mariner dataset provides active longitudinal follow-up based upon unique patient identifier codes that are not limited to changes in insurance status, minimizing loss to follow-up in the system. Therefore, patients with 2-year follow-up were determined as any patient with continued coverage two years following lumbar fusion.
Exclusion and inclusion criteria
Patients with a diagnosis of HIV were identified using ICD-9/10 diagnosis codes. These patients were further categorized into symptomatic HIV (AIDS) (ICD-9-D-042 and ICD-9-D-B20) and asymptomatic HIV (AHIV) (ICD-10-D-V08 and ICD-10-D-Z21) using ICD billing codes described in the CDC guidelines for coding and reporting HIV infection (19,20). Our three groups of interest were identified as those who underwent lumbar fusion that (I) had a diagnosis of HIV, (II) had symptomatic HIV (AIDS) at the time of lumbar fusion, (III) or had asymptomatic HIV at the time of lumbar fusion. The control group consisted of patients who underwent lumbar fusion with no known diagnosis of HIV. Inclusion and exclusion criteria were based on a previous similar study (6). Patients that were less than 18 years of age were excluded. Patients who underwent lumbar fusion for infection, vertebral dislocation, traumatic spondylopathy, fracture, collapsed vertebrae, lesion/tumor removal, or who were post-laminectomy were excluded. Patients who underwent lumbar fusion for lumbar spondylosis, spinal stenosis, spondylolisthesis, intervertebral disc disorder, disc degeneration, postural lordosis, lumbar instability, lumbar radiculopathy, and sciatica were included in this study. This exclusion and inclusion criteria are shown in Figure 1. The number of patients in the database that met these criteria determined the sample size.
Demographics/comorbidities and outcome variables
Patient demographic and comorbidities observed include age, gender, osteoporosis and Elixhauser Comorbidity index comorbidities (congestive heart failure, arrhythmias, valvular disease, pulmonary circulatory disorders (PCD), peripheral vascular disease, hypertension, paralysis, chronic obstructive pulmonary disease, diabetes, hypothyroidism, chronic kidney disease, liver disease, peptic ulcer disease (PUD), lymphoma, metastatic cancer, non-metastatic cancer, rheumatoid arthritis and cardiovascular disease, coagulopathy, fluid and electrolyte disorders, anemia due to blood loss, anemia due to deficiency, alcohol abuse, drug abuse, psychoses, depression, obesity, and smoking status), collected using ICD-9 and ICD-10 diagnosis codes (21). The primary outcomes of this study were 2-year surgical and medical complications including all-cause revision, infection, digestive system complications, bowel and bladder dysfunction, neurologic complications, plegia, sensory deficit, and myelopathies within two years of lumbar fusion. Secondary outcomes included 90-day postoperative complications: acute renal failure, anemia, arrhythmia with and without atrial fibrillation, blood transfusion, bleeding complications, deep vein thrombosis (DVT), pulmonary thrombosis (PE), stroke, heart failure, respiratory complications, pneumonia, urinary tract infection (UTI), sepsis, and death. Primary and secondary outcomes were collected using ICD-9 and ICD-10 diagnosis codes.
Statistical analysis
Patient data on demographics, comorbidities, and postoperative outcomes were analyzed using univariate and multivariate analysis via R software provided by PearlDiver. Univariate analysis was conducted using Chi-squared and Student t-tests where appropriate. Any postoperative outcome with a P value less than 0.2 on univariate analysis was included as a separate dependent variable on multivariable analysis. Demographics and comorbidities with a P value less than 0.2 on univariate analysis were included as independent variables in multivariable regression to mitigate confounding variables and control for covariates. Multivariable regression was conducted using logistic regression using R software provided by Pearldiver. Results from the multivariate analysis were reported as odds ratios (ORs) and 95% confidence intervals (CIs). A P value of 0.05 was used at the level of significance.
Ethical statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was exempt from IRB approval by the George Washington University institutional review board and individual consent from this retrospective analysis was waved.
Results
Demographics
Overall, 216,587 patients who underwent lumbar fusion for degenerative spine indications were included in the analysis. There were 215,956 HIV negative patients and 631 (0.29%) HIV positive patients (HIV). Of the HIV positive patients, 129 (0.06%) had symptomatic HIV (AIDS) and 502 (0.23%) patients had asymptomatic HIV (AHIV). Compared to patients who did not have HIV, those with HIV were more likely to be younger (58.91 vs. 53.83 years old; P<0.001) and Male (68.94% vs. 31.06%; P<0.001). Patients with HIV were more likely to have an alcohol use disorder (2.54% vs. 1.39%; P=0.022), use illicit drugs (24.88% vs. 10.24%; P<0.001), have a psychotic disorder (8.40% vs. 3.91%; P<0.001), suffer from depression (55.63% vs. 40.28%; P<0.001) and smoke (41.36% vs. 24.47%; P<0.001) (Table 1).
Table 1
| Characteristics | All HIV patients | P value† | Asymptomatic HIV | P value† | AIDS | P value† | Control | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||||
| Total | 631 | 502 | 129 | 215,956 | |||||||
| Mean age (SD) | 53.83 | <0.001‡* | 53.466 | <0.001‡* | 55.25 | <0.001‡* | 58.91 | ||||
| Gender | <0.001‡* | <0.001‡* | <0.001‡* | ||||||||
| Male | 435 | 68.94 | 334 | 66.53 | 101 | 78.29 | 88,374 | 40.92 | |||
| Female | 196 | 31.06 | 168 | 33.47 | 28 | 21.71 | 127,582 | 59.08 | |||
| CHF | 72 | 11.41 | 0.943 | 56 | 11.16 | <0.001* | 16 | 12.40 | 0.781 | 24,272 | 11.24 |
| Arrhythm IAS | 226 | 35.82 | 0.085 | 168 | 33.47 | 0.687 | 58 | 44.96 | 0.003* | 70,234 | 32.52 |
| Valvular disease | 111 | 17.59 | 0.649 | 89 | 17.73 | 0.6341 | 22 | 17.05 | 1 | 36,353 | 16.83 |
| PULM CIRC disorders | 39 | 6.18 | 0.393 | 29 | 5.78 | 0.734 | 10§ | 7.75 | 0.306 | 11,523 | 5.34 |
| PVD | 123 | 19.49 | 0.696 | 100 | 19.92 | 0.922 | 23 | 17.83 | 0.576 | 43,615 | 20.20 |
| HTN | 409 | 64.82 | 0.929 | 327 | 65.14 | 1 | 82 | 63.57 | 0.0791 | 140,514 | 65.07 |
| Paralysis | 35 | 5.55 | <0.001* | 27 | 5.38 | <0.001* | 8§ | 6.20 | 0.091 | 6,895 | 3.19 |
| COPD | 292 | 46.28 | <0.001* | 227 | 45.22 | <0.001* | 65 | 50.39 | <0.001* | 73,535 | 34.05 |
| DM | 220 | 34.87 | 0.03* | 184 | 36.65 | <0.001* | 36 | 27.91 | 0.507 | 66,941 | 31.00 |
| Hypothyroidism | 116 | 18.38 | <0.001* | 100 | 19.92 | <0.001* | 16 | 12.40 | <0.001* | 55,223 | 25.57 |
| CKD | 141 | 22.35 | <0.001* | 103 | 20.52 | <0.001* | 38 | 29.46 | <0.001* | 29,935 | 13.86 |
| Liver disease | 210 | 33.28 | <0.001* | 162 | 32.27 | <0.001* | 48 | 37.21 | <0.001* | 30,495 | 14.12 |
| PUD | 13 | 2.06 | 0.448 | 10 | 1.99 | 0.603 | 3§ | 2.33 | 0.761 | 3,457 | 1.60 |
| Lymphoma | 0 | 0.00 | 0.157* | 7§ | 1.39 | 0.435 | 3§ | 2.33 | 0.252 | 2,063 | 0.96 |
| Cancer MET | 17 | 2.69 | 0.712 | 13 | 2.59 | 0.883 | 4§ | 3.10 | 0.81 | 5,161 | 2.39 |
| Cancer no MET | 77 | 12.20 | 0.679 | 58 | 11.55 | <0.001* | 19 | 14.73 | 0.33 | 25,042 | 11.60 |
| RA CVD | 118 | 18.70 | 0.208 | 101 | 20.12 | 0.741 | 17 | 13.18 | 0.043* | 44,959 | 20.82 |
| COAG DEF | 72 | 11.41 | <0.001* | 52 | 10.36 | <0.001* | 20 | 15.50 | <0.001* | 14,453 | 6.69 |
| Electrolytes | 266 | 42.16 | <0.001* | 210 | 41.83 | <0.001* | 56 | 43.41 | 0.005* | 68,129 | 31.55 |
| Anemia bloodloss | 26 | 4.12 | 0.88 | 22 | 4.38 | 0.6793 | 4§ | 3.10 | 0.799 | 8,474 | 3.92 |
| Anemia deficiency | 96 | 15.21 | 0.454 | 80 | 15.94 | 0.263 | 16 | 12.40 | 0.67 | 30,441 | 14.10 |
| Alcohol | 16 | 2.54 | 0.022* | 13 | 2.59 | 0.035* | 3§ | 2.33 | 0.592 | 2,992 | 1.39 |
| Drugs | 157 | 24.88 | <0.001* | 116 | 23.11 | <0.001* | 41 | 31.78 | <0.001* | 22,115 | 10.24 |
| Psychosis | 53 | 8.40 | <0.001* | 42 | 8.37 | <0.001* | 11 | 8.53 | 0.013* | 8,438 | 3.91 |
| Depression | 351 | 55.63 | <0.001* | 267 | 53.19 | <0.001* | 84 | 65.12 | <0.001* | 86,981 | 40.28 |
| Smoking | 261 | 41.36 | <0.001* | 205 | 40.84 | <0.001* | 56 | 43.41 | <0.001* | 52,847 | 24.47 |
| Obesity | 125 | 19.81 | 0.689 | 108 | 21.51 | 0.188 | 17 | 13.18 | 0.110 | 41,254 | 19.10 |
†, Pearson’s chi-squared test; ‡, analysis of variance; §, per HIPAA requirements, <11 cohort sizes are not reportable; *, significance P<0.05; CHF, congestive heart failure; Pulm Circ Disorder, pulmonary circulatory disorder; PVD, peripheral vascular disease; HTN, hypertension; COPD, chronic obstructive pulmonary disease; DM, diabetes mellitus; CKD, chronic kidney disease; PUD, peptic ulcer disease; Cancer Met, cancer with metastasis; Cancer no Met, cancer no metastasis; RA CVD, rheumatoid arthritis cardiovascular disease; Coag Def, coagulation deficiency; SD, standard deviation.
Comorbidities
Relative to patients without HIV, patients who have HIV were more likely to have comorbidities, including paralysis (5.55% vs. 3.19%; P<0.001) chronic pulmonary disorders (46.28% vs. 34.05%; P<0.001), diabetes (34.87% vs. 31.00%; P=0.03), chronic kidney disease (22.35% vs. 13.86%; P<0.001), liver disease (33.28% vs. 14.12%; P<0.001), coagulation deficiency (11.41% vs. 6.69%; P<0.001), and electrolyte deficiency (42.16% vs. 31.55%; P<0.001). Patients without HIV were more likely to have hypothyroidism (25.57% vs. 18.38%; P<0.001). There was no significant difference in the rates of osteoporosis between patients with HIV and the control group (0.48% vs. 0.82%; P=0.758) (Table 1).
Compared to HIV negative patients, patients with AIDS were more likely to have congestive heart failure (12.40% vs. 11.24%; P=0.003). However, when comparing the rates of CHF between HIV negative patients and AHIV patients, there was no significant difference (11.16% vs. 11.24%; P=0.687) (Table 1).
90-day medical complications
Univariate analysis showed that compared to patients who did not have HIV, those with HIV were more likely to develop renal failure (4.60% vs. 2.87%; P=0.013), pneumonia (4.28% vs. 2.02%; P<0.001), and respiratory complications (2.54% vs. 1.46%; P<0.038) within 90 days of lumbar fusion. Patients with HIV were more likely to experience a longer length of stay (LOS) in the hospital (3.84 vs. 3.475 days; P<0.001) (Table 2). When subdividing HIV positive patients into AHIV and AIDS, patients with AHIV had an average length of stay of 3.649 and those with a diagnosis of AIDS had an average length of stay of 8.12 days. Patients with AIDS were more likely to have pneumonia (10.08% vs. 2.02%; P<0.001), respiratory complications (5.43% vs. 1.46%; P<0.001) and sepsis (5.43% vs. 1.37%; P<0.001) within 90 days of the procedure compared to HIV negative patients.
Table 2
| Complications | All HIV Patients | P value† | Asymptomatic HIV | P value† | AIDS | P value† | Control | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||||
| Total | 631 | 502 | 129 | 215,956 | |||||||
| Renal failure | 29 | 4.60 | 0.013* | 15 | 2.99 | 0.981 | 14 | 10.85 | <0.001* | 6,198 | 2.87 |
| Anemia | 69 | 10.94 | 0.149 | 51 | 10.16 | 0.073* | 18 | 13.95 | 0.834 | 27,956 | 12.95 |
| Arrhythmia with AFIB | 38 | 6.02 | 0.058 | 26 | 5.18 | 0.018* | 12 | 9.30 | 0.759 | 17,655 | 8.18 |
| Arrhythmia without AFIB | 32 | 5.07 | 0.823 | 21 | 4.18 | 0.288 | 11§ | 8.53 | 0.159 | 11,556 | 5.35 |
| Blood transfusion | 33 | 5.23 | 1 | 29 | 5.78 | 0.67 | 12 | 9.30 | 0.182 | 11,342 | 5.25 |
| Bleeding complications | 5§ | 0.79 | 0.623 | 5§ | 1.00 | 1 | 0 | 0.00 | 0.449 | 2,319 | 1.07 |
| Death | 1§ | 0.16 | 1 | 1§ | 0.20 | 1 | 0 | 0.00 | 1 | 456 | 0.21 |
| DVT | 10§ | 1.58 | 0.975 | 9§ | 1.79 | 0.708 | 1§ | 0.78 | 0.759 | 3,218 | 1.49 |
| Heart failure | 11 | 1.74 | 0.12 | 8§ | 1.59 | 0.185* | 3§ | 2.33 | 1 | 5,706 | 2.64 |
| Pulmonary embolism | 4§ | 0.63 | 0.52 | 4§ | 0.80 | 0.878 | 0 | 0.00 | 0.503 | 2,081 | 0.96 |
| Pneumonia | 27 | 4.28 | <0.001* | 14 | 2.79 | 0.288 | 13 | 10.08 | <0.001* | 4,364 | 2.02 |
| Respiratory complications | 16 | 2.54 | 0.038* | 9§ | 1.79 | 0.665 | 7§ | 5.43 | <0.001* | 3,155 | 1.46 |
| Sepsis | 14 | 2.22 | 0.096 | 7§ | 1.39 | 1 | 7§ | 5.43 | <0.001* | 2,953 | 1.37 |
| CVA | 3§ | 0.48 | 0.375 | 3§ | 0.60 | 0.652 | 0 | 0.00 | 0.546 | 1,913 | 0.89 |
| UTI | 39 | 6.18 | 0.615 | 30 | 5.98 | 0.54 | 9§ | 6.98 | 1 | 14,606 | 6.76 |
| Cellulitis | 16 | 2.54 | 0.936 | 9§ | 1.79 | 0.453 | 7§ | 5.43 | 0.051 | 5,198 | 2.41 |
| Neuro complications | 2§ | 0.32 | 0.6125 | 2§ | 0.40 | 0.887 | 0 | 0.00 | 0.808 | 1,177 | 0.55 |
| Readmit | 45 | 7.13 | 0.1213 | 34 | 6.77 | 0.3103 | 11 | 8.53 | 0.216 | 12,154 | 5.63 |
| LOS | 3.475 | <0.001 | 3.649 | 0.138 | 8.115 | <0.001 | 3.475 | 0.00 | |||
†, Pearson’s chi-squared test; §, per HIPAA requirements, <11 cohort sizes are not reportable; *, significance P<0.05; Arrhythmia with AFIB, arrhythmia without atrial fibrillation; Arrhythmia without AFIB, arrhythmia without atrial fibrillation; DVT, deep vein thrombosis; CVA, cerebrovascular accident; UTI, urinary tract infection; LOS, length of stay.
2-year surgical and medical complications
On univariate analysis, there was no significant difference between the control cohort and patients with HIV in any of the 2-year surgical complications analyzed. There was no significant difference in risk of revision rates, SSI, neurological complications, digestive complications, plegia, sensory deficit, bowel/bladder dysfunction or myelopathies between the HIV negative patients and HIV positive patients. No significant difference was seen when comparing risk of 2-year complications between the control group and the asymptomatic HIV and AIDS groups individually (Table 3).
Table 3
| Outcomes | ALL HIV patients | P value† | Asymptomatic HIV | P value† | AIDS | P value† | Control | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||||
| Total | 631 | 502 | 129 | 215,956 | |||||||
| Revision | 11 | 1.74 | 0.8385 | 8§ | 1.59 | 0.695 | 3§ | 2.33 | 0.998 | 4,178 | 1.93 |
| SSI | 28 | 4.44 | 0.4383 | 20 | 3.98 | 0.892 | 10§ | 7.75 | 0.223 | 8,140 | 3.77 |
| Neurological complications | 1§ | 0.16 | 0.07 | 0 | 0.00 | 0.053 | 1§ | 0.78 | 1 | 2,007 | 0.93 |
| Digestive complications | 1§ | 0.16 | 0.893 | 1§ | 0.20 | 1 | 0 | 0.00 | 1 | 573 | 0.27 |
| Plegia | 2§ | 0.32 | 0.3054 | 1§ | 0.20 | 0.243 | 1§ | 0.78 | 1 | 1,616 | 0.75 |
| Sensory defecit | 39 | 6.18 | 0.881 | 32 | 6.37 | 1 | 7§ | 5.43 | 0.784 | 13,836 | 6.41 |
| Bowel bladder dysfunction | 32 | 5.07 | 0.13 | 22 | 4.38 | 0.051 | 10§ | 7.75 | 0.747 | 14,373 | 6.66 |
| Myelopathies | 1§ | 0.16 | 0.36 | 1§ | 0.20 | 0.535 | 0 | 0.00 | 0.864 | 1,065 | 0.49 |
†, Pearson’s chi-squared test; §, Per HIPAA requirements, <11 cohort sizes are not reportable; *, significance P<0.05; SSI, surgical site infection; arrhythmia with AFIB, arrhythmia without atrial fibrillation; arrhythmia without AFIB, arrhythmia without atrial fibrillation; DVT, deep vein thrombosis; CVA, cerebrovascular accident; UTI, urinary tract infection; LOS, length of stay.
Multivariate analysis
Following adjustment on multivariate analysis to control for demographics and comorbidities, patients with HIV had greater odds of 90-day postoperative pneumonia (OR 1.592; 95% CI: 1.048–2.314; P=0.021). Specifically, AIDS patients had greater odds of any 90-day respiratory complications (OR 2.585; 95% CI: 1.075–5.264; P=0.017) (Table 4). There was no significant difference in odds of 90-day sepsis between HIV negative and HIV positive patients (OR 1.202; 95% CI: 0.668–1.982; P=0.505), but when sub-stratifying the HIV positive group, patients with AIDS were at greater odds of having septic complications (OR 2.702; 95% CI: 1.122–5.514; P=0.013). Patients with asymptomatic HIV were found to have lesser odds of 2-year bowel/bladder dysfunction compared to the control cohort (OR 0.568; 95% CI: 0.358–0.854; P=0.011) (Table 4).
Table 4
| Multivariate | ALL HIV patients | Asymptomatic HIV | AIDS | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Odds ratio | 25% | 75% | P value† | Odds ratio | 25% | 75% | P value† | Odds ratio | 25% | 75% | P value† | |||
| Neurological complications | 0.127 | 0.007 | 0.560 | 0.039* | 5.32E-06 | 1.95E-33 | 2.31E-34 | 0.908 | – | – | – | – | ||
| Bowel bladder dysfunction | 0.646 | 0.441 | 0.911 | 0.018* | 0.568 | 0.358 | 0.854 | 0.011* | – | – | – | – | ||
| Myelopathies | – | – | – | – | – | – | – | – | – | – | – | – | ||
| Osteoporosis | – | – | – | – | 0.223 | 0.013 | 0.988 | 0.134 | 2.765 | 0.673 | 7.488 | 0.087 | ||
| Renal failure | 1.251 | 0.827 | 1.821 | 0.265 | – | – | – | – | 2.912 | 1.521 | 5.213 | 0.001* | ||
| Anemia | 0.934 | 0.718 | 1.197 | 0.601 | 0.866 | 0.638 | 1.152 | 0.340 | – | – | – | – | ||
| Arrhythmia with AFIB | – | – | – | – | 0.641 | 0.418 | 0.939 | 0.030* | – | – | – | – | ||
| Arrhythmia without AFIB | – | – | – | – | – | – | – | – | 1.323 | 0.650 | 2.463 | 0.406 | ||
| Heart failure | 0.633 | 0.323 | 1.109 | 0.142 | 0.632 | 0.276 | 1.265 | 0.231 | – | – | – | – | ||
| Blood transfusion | – | – | – | – | – | – | – | – | 0.605 | 0.185 | 1.451 | 0.327 | ||
| Pulmonary embolism | – | – | – | – | – | – | – | – | – | – | – | – | ||
| Cellulitis | 1.656 | 0.693 | 3.337 | 0.202 | ||||||||||
| Pneumonia | 1.592 | 1.048 | 2.314 | 0.021* | – | – | – | – | 3.564 | 1.883 | 6.207 | 0.001* | ||
| Respiratory complications | 1.326 | 0.767 | 2.127 | 0.275 | – | – | – | – | 2.585 | 1.075 | 5.264 | 0.017* | ||
| Sepsis | 1.202 | 0.668 | 1.982 | 0.505 | – | – | – | – | 2.702 | 1.122 | 5.514 | 0.013* | ||
†, Pearson’s chi-squared test; *, significance P<0.05.
Discussion
There has been a significant increase in spinal surgery in HIV-positive patients (5) with spine surgeries increasing at a 0.094 incidence per 100,000 in the year 2000 and 0.303 in 2009, but few studies examine the impact of HIV status on long-term surgical outcomes for degenerative spinal conditions. Therefore, there is varying evidence in the literature regarding post-surgical outcomes in HIV-positive patients undergoing lumbar fusion. It had been shown that HIV-positive patients undergoing spinal surgery for degenerative spine disease have a higher incidence of hospital mortality and complications (5), but no studies have evaluated the effect of an HIV-positive diagnosis on revision rates beyond one year. HIV populations are more likely to have low BMD and carry a higher risk of implant infection (9,10), all of which are associated with an increased risk of fusion failure and revision after one year (18). With effective therapies available to treat HIV (1), the life-span of patients with a positive HIV status as well as their development of chronic conditions and comorbidities (2,3) continues to increase. Therefore, understanding long-term complications in this patient population is crucial to optimizing outcomes and patient satisfaction.
Our study’s main focus was on HIV patients who received primary elective lumbar fusions for degenerative spinal conditions. By controlling for patient comorbidities, our study was able to focus on HIV-positive status, with HIV patients further categorized into asymptomatic and AIDS groups to account for discrepancies. We predicted that the HIV- positive population would experience a significant increase in complications and adverse postoperative outcomes, including postoperative infections and increased 2-year revision rates compared to the non-HIV patient cohort. Specifically, patients with AIDS would have increased 90-day complications and worse 2-year outcomes. Our hypothesis was rejected as no significant differences in infectious complications and 2-year revision rates were found between the HIV-positive and the HIV-negative patients in the study. Additionally, there were no significant differences in the rates of osteoporosis between the HIV groups and control cohort. Among the asymptomatic and the AIDS cohorts, greater odds of respiratory complications (OR 2.585; 95% CI: 1.075–5.264; P=0.017) and septic complications (OR 2.702; 95% CI: 1.122–5.514; P=0.013) were seen among the AIDS cohort.
Based on the present literature, we had expected the HIV cohort to experience an increase in infectious complications following lumbar fusions (7). However, this single-center, retrospective data review from 2010 to 2016 yielded a total of 4,968 patients who underwent spine surgery, of which 45 patients had an HIV infection. This resulted in a much smaller sample size than our study, which had 216,587 patients that underwent lumbar fusion with 631 patients having HIV infection. Given the difference in sample size, our study was more robust to capture more nuanced differences in outcomes.
Prior retrospective studies found that symptomatic HIV-positive patients had increased complications but were not associated with poorer surgical outcomes compared to patients with asymptomatic HIV (22). Our study showed a significantly longer LOS among AIDS patients compared to HIV-negative patients (8.115 vs. 3.475 days; P<0.001), putting them at increased risk for further hospital acquired complications (23) and increased healthcare costs.
Similar to our study, a retrospective review of the National Inpatient Sample (NIS) database that was propensity-score matched found that aside from respiratory complications, AHIV status did not adversely impact the overall perioperative course of patients undergoing spinal fusion for degenerative disc disease (22,24). Our study showed that the AHIV cohort was not more likely of having major complications such as DVT, PE, heart failure, or death within 90-day of lumbar fusion when compared with the HIV-negative cohort. Therefore, adequate control of HIV viral load to maintain an asymptomatic state can potentially help reduce adverse outcomes. Additionally, maintaining a low viral load and reducing the complication rate can ultimately reduce a patient’s length of stay and overall costs.
Furthermore, as association between HIV and smoking, and COPD, has been previously described by Lovy et al. (25) Patients with HIV in our study were more likely to have COPD (46.28% vs. 34.05%; P<0.001) and smoke (41.36% vs. 24.47%; P<0.001). These factors could be associated with the increased incidence of respiratory complications and pneumonia seen in the HIV-positive cohort.
There are numerous strengths to this study. The use of the Pearldiver database utilized data from numerous institutions resulting in a large sample size, which helped to strengthen the internal and external study validity. However, there are several limitations due to the nature of the database. One limitation is that our analysis utilized CPT billing codes to determine procedures as well as inclusion and exclusion criteria. The final data could have been affected by human error when billing for the lumbar fusion procedures included in this study. Additionally, it is possible that some patients required postoperative surgical revisions beyond the two-year period analyzed, which could affect the additional outcomes included in this analysis. To address this limitation, future studies should include longer follow-up time periods for postoperative outcomes, such as analysis of 5- and 10-year postoperative outcomes. A third limitation is the inability to evaluate patient reported outcome measures following the operation as well as additional environmental and social factors which may correspond to a patient’s overall wellbeing and satisfaction. It is important to note that PearlDiver does not provide CD4+ count on any HIV patient. These numbers would have been beneficial to understanding the level of immune restoration for AHIV patients.
To our knowledge, this is the only article to evaluate HIV positive status on revision rates in lumbar fusions using a large database. Our results indicate that HIV-positive status does not affect 2-year revision rates following lumbar fusion. If appropriate prophylaxis strategies are taken before and after the procedure, HIV-positive patients may be successful lumbar fusion candidates, especially with a well-controlled HIV viral load. However, future studies should investigate the impact of HIV antiretroviral therapies on surgical spine outcomes to determine whether an association between medications and outcomes exists for HIV positive patients. As the number of HIV positive patients undergoing elective surgery increases, it is imperative that surgeons carefully weigh the risks and benefits of operating on patients with a diagnosis of HIV and monitor their patients closely postoperatively to mitigate potential complications.
Acknowledgments
We want to thank the Orthopaedic Department at Johns Hopkins University and Dr. Savyasachi Thakkar for their contribution to making this article Open Access.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://dx.doi.org/10.21037/jss-21-84
Data Sharing Statement: Available at https://dx.doi.org/10.21037/jss-21-84
Peer Review File: Available at https://dx.doi.org/10.21037/jss-21-84
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/jss-21-84). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was exempt from IRB approval by the George Washington University institutional review board and individual consent from this retrospective analysis was waved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wandeler G, Johnson LF, Egger M. Trends in life expectancy of HIV-positive adults on antiretroviral therapy across the globe: comparisons with general population. Curr Opin HIV AIDS 2016;11:492-500. [Crossref] [PubMed]
- Best MJ, Buller LT, Eismont FJ. National Trends in Ambulatory Surgery for Intervertebral Disc Disorders and Spinal Stenosis: A 12-Year Analysis of the National Surveys of Ambulatory Surgery. Spine (Phila Pa 1976) 2015;40:1703-11. [Crossref] [PubMed]
- Pretell-Mazzini J, Subhawong T, Hernandez VH, et al. HIV and Orthopaedics: Musculoskeletal Manifestations and Outcomes. J Bone Joint Surg Am 2016;98:775-86. [Crossref] [PubMed]
- Yoshihara H, Yoneoka D. National trends and in-hospital outcomes in HIV-positive patients undergoing spinal fusion. Spine (Phila Pa 1976) 2014;39:1694-8. [Crossref] [PubMed]
- Farias FAC, Dagostini CM, Falavigna A. HIV and Surgery for Degenerative Spine Disease: A Systematic Review. J Neurol Surg A Cent Eur Neurosurg 2021;82:468-74. [Crossref] [PubMed]
- Donnally CJ 3rd, Kalakoti P, Buskard ANL, et al. Inpatient Outcomes After Elective Lumbar Spinal Fusion for Patients with Human Immunodeficiency Virus in the Absence of Acquired Immunodeficiency Syndrome. World Neurosurg 2018;116:e913-20. [Crossref] [PubMed]
- Ishida W, Ramhmdani S, Perdomo-Pantoja A, et al. Matched-pair cohort study of spinal surgery in HIV-infected patients: Minimum one-year follow-up. J Spine 2018;18:S152-3. [Crossref]
- Hileman CO, Eckard AR, McComsey GA. Bone loss in HIV: a contemporary review. Curr Opin Endocrinol Diabetes Obes 2015;22:446-51. [Crossref] [PubMed]
- Harrison WJ, Lewis CP, Lavy CB. Wound healing after implant surgery in HIV-positive patients. J Bone Joint Surg Br 2002;84:802-6. [Crossref] [PubMed]
- Kigera JW, Straetemans M, Vuhaka SK, et al. Is there an increased risk of post-operative surgical site infection after orthopaedic surgery in HIV patients? A systematic review and meta-analysis. PLoS One 2012;7:e42254. [Crossref] [PubMed]
- Khalid SI, Nunna RS, Maasarani S, et al. Association of osteopenia and osteoporosis with higher rates of pseudarthrosis and revision surgery in adult patients undergoing single-level lumbar fusion. Neurosurg Focus 2020;49:E6. [Crossref] [PubMed]
- Park SB, Chung CK. Strategies of spinal fusion on osteoporotic spine. J Korean Neurosurg Soc 2011;49:317-22. [Crossref] [PubMed]
- Díaz-Romero Paz R, Sosa Henríquez M, Armas Melián K, et al. Trends and attitudes of spine surgeons regarding osteoporosis. Neurocirugia (Astur : Engl Ed) 2019;30:268-77.
- Morris MT, Tarpada SP, Tabatabaie V, et al. Medical optimization of lumbar fusion in the osteoporotic patient. Arch Osteoporos 2018;13:26. [Crossref] [PubMed]
- Uei H, Tokuhashi Y, Maseda M, et al. Exploratory analysis of predictors of revision surgery for proximal junctional kyphosis or additional postoperative vertebral fracture following adult spinal deformity surgery in elderly patients: a retrospective cohort study. J Orthop Surg Res 2018;13:252. [Crossref] [PubMed]
- Chin DK, Park JY, Yoon YS, et al. Prevalence of osteoporosis in patients requiring spine surgery: incidence and significance of osteoporosis in spine disease. Osteoporos Int 2007;18:1219-24. [Crossref] [PubMed]
- Thomas MV, Puleo DA. Infection, inflammation, and bone regeneration: a paradoxical relationship. J Dent Res 2011;90:1052-61. [Crossref] [PubMed]
- Gjolaj JP. P20. Surgical site infection as a risk factor for long-term instrumentation failure in patients with spinal deformity: a retrospective cohort study. Spine J 2020;20:S156-7. [Crossref]
- Official authorized addenda: Human immunodeficiency virus infection codes and official guidelines for coding and reporting ICD-9-CM. 2013.
- ICD-10-CM official guidelines for coding and reporting FY 2021 – UPDATED January 1, 2021 (October 1, 2020 - September 30, 2021). 2021:20-22. Available online: https://www.cdc.gov/mmwr/preview/mmwrhtml/00032908.htm
- Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care 1998;36:8-27. [Crossref] [PubMed]
- Horberg MA, Hurley LB, Klein DB, et al. Surgical outcomes in human immunodeficiency virus-infected patients in the era of highly active antiretroviral therapy. Arch Surg 2006;141:1238-45. [Crossref] [PubMed]
- Jeon CY, Neidell M, Jia H, et al. On the role of length of stay in healthcare-associated bloodstream infection. Infect Control Hosp Epidemiol 2012;33:1213-8. [Crossref] [PubMed]
- Shah NV, Lettieri MJ, Scheer R, et al. 19. Does asymptomatic human immunodeficiency virus (AHIV)-positive status in patients undergoing spinal fusion for degenerative disc disease (DDD) increase risk for adverse postoperative outcomes? Spine J 2020;20:S10. [Crossref]
- Lovy AJ, Guzman JZ, Skovrlj B, et al. Prevalence, comorbidities, and risk of perioperative complications in human immunodeficiency virus-positive patients undergoing cervical spine surgery. Spine (Phila Pa 1976) 2015;40:E1128-34. [Crossref] [PubMed]


