
Traumatic intradural disc herniation following a cervical facet dislocation: a case report
Introduction
Unilateral cervical facet dislocations (CFD) account for about 6–10% of all cervical injuries (1). The most common causes of CFD include motor vehicle accidents, sports accidents, falls, and direct head-loading injuries (2). This type of injury mainly involves excessive flexion-distraction or flexion-rotation, resulting in the inferior facets of the superior vertebra shifting anteriorly relative to the superior facet of the inferior vertebra (3). Severe lower CFD are usually associated with compromise of the longitudinal ligaments, ligament flavum, apophyseal joint ligaments, annulus fibrosis, and interspinous ligaments (4). Due to the forces involved, complete or incomplete spinal cord injuries can be associated with these injuries (3).
In the setting of facet dislocations, the definitive surgical management may be influenced by whether a disc herniation is seen on the pre-operative magnetic resonance imaging (MRI) scan (5). In cases where a disc herniation is present, many surgeons will advocate an anterior approach to first decompress the spinal canal before any reduction is made to prevent the disc from “migrating” into the canal, causing more compression on the spinal cord (6). If there is no disc herniation, either a posterior or anterior approach will suffice (7).
We present a rare case of an intradural disc herniation following a left unilateral C5/6 facet dislocation despite his pre-operative MRI scan not showing an obvious large anterior disc fragment. If decompression and fixation surgery was performed with a posterior approach only, this may have been inadequate as the residual disc fragment would be retained. Here, we highlight the management of the intradural disc herniation and the associated large dural defect, and discuss some of the benefits of starting with an anterior approach, followed by the posterior approach if necessary. We present the following case in accordance with the CARE reporting checklist (8) (available at https://jss.amegroups.com/article/view/10.21037/jss-21-106/rc).
Case presentation
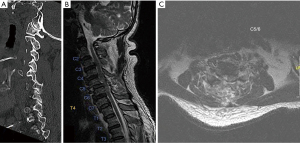
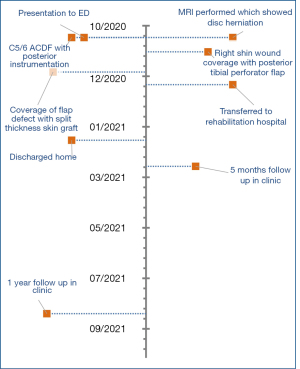
A 65-year-old Chinese gentleman presented after a fall into a 2 m deep drain after being intoxicated with alcohol. He was an otherwise fit gentleman who had a past medical history of hypertension and diabetes mellitus since September 2018 that is being treated with metformin. Premorbidly, he was able to perform his activities of daily living independently and ambulated without walking aids. On examination at presentation, his Glasgow Coma Scale (GCS) was 14. His power was full until the C6 myotome distribution bilaterally, his C7 power was 2 on the right and 3 on the left. Otherwise, his power was 0 from C8 downwards. His sensation was intact throughout and the bulbocavernous reflex was present. In addition, he had bilateral anterior distal shin wounds. Subsequently, he was diagnosed with an American Spinal Injury Association (ASIA) B incomplete spinal cord injury. On imaging of the cervical spine with computed tomography (CT), there was mild anterior spondylolisthesis at the C5/6 region on the middle sagittal cut. In addition, there was a left perched facet at C5/6 and mild joint space widening on the right side (Figure 1). The MRI of his cervical spine showed severe cord compression at C5/6 with an interspinous ligament injury from C4-6, resulting in a 3-column injury (Figure 1). The provisional diagnosis at this time was that of a C5/6 disc herniation secondary to a perched left C5/6 facet. There was diagnostic difficulty in identifying an intradural disc herniation based on MRI scan as this is usually identified intra-operatively (9), furthermore, the MRI was reported as having a C5/6 posterior right paracentral disc extrusion.
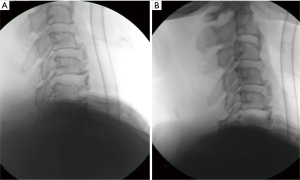
He then underwent an emergency closed reduction of the facet dislocation and surgical decompression at C5/6 through a combined anterior and posterior approach. He was initially positioned supine for a closed reduction under general anaesthesia (GA) with a Mayfield clamp. This was performed using slight traction under intraoperative imaging (II) guidance which was successful. Reduction of the dislocation was checked to be satisfactory based on 3 criteria. The first was a palpable clunk, the second was the satisfactory posterior vertebral body line based on II (Figure 2), and the last was the restored alignment of the facet joints.
Following which, an anterior cervical discectomy and fusion (ACDF) at C5/6 was performed. A right sided approach to the cervical spine was utilised to expose the cervical vertebrae beneath the anterior longitudinal ligament. During the discectomy process, it was discovered that there was a large intradural disc fragment causing severe cord compression (Video 1). In addition, the dura and posterior longitudinal ligament (PLL) were completely torn over the ventral surface. There was also continuous cerebral spinal fluid (CSF) leakage after the annulotomy was performed. Once the discectomy and decompression were accomplished, a size 8 Nuvasive Coroent lordotic cage was then inserted into the C5/6 space with a 2-level anterior cervical plate secured with 4 screws. The dura defect was not reparable and we also did not inject any sealants e.g., duraseal given the possibility of it migrating down the spinal cord. The soft tissue layers were closed sequentially and a lantern drain was inserted concurrently.
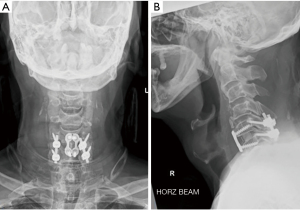
Following the completion of the ACDF procedure, he was then turned 180° to a prone position on a Jackson table for the posterior instrumentation and fusion at the C5/6 level. The skin overlying the C5/6 spinous processes was dissected and the lamina and facet joints were exposed. Lateral mass screws were then inserted with care at the C5 and C6 levels and screw position checked using II guidance. The rods were then placed over the screw heads and secured with set screws, bone graft was then placed in the posterolateral gutters for further bone fusion and stability. The skin was then closed in layers with a Radivac drain left in situ posteriorly.
Postoperatively, there was concern regarding high volumes of CSF accumulation in the anterior component of the spinal cord. Initially, the volume of CSF in the lantern drain was 263 mls on post-operative day (POD) 1, however this decreased to 35 mls on POD2, and the drain was removed on POD3. A Radivac drain was also placed in the posterior compartment of the cervical spine which yielded 110 mls of haemoserous fluid on POD1 and was eventually removed on POD6. There were fluctuations in the lower limb neurological examination on POD1, with periods of flickers of movement in his toes and periods with no movement in his lower limbs. On POD2, there was a dramatic improvement in his left lower limb power, his power was 5 proximally and 3 distally. His wound was then exposed on POD14 with minimal signs of infection or dehiscence. Post-operative imaging of his cervical spine on POD14 revealed stable implant positions and no loosening of the screws (Figure 3). He was subsequently transferred to a rehabilitation hospital for further reconditioning on POD57 and discharged home 4 months after his surgery. On his review in clinic 5 months post-op, his power was mostly 4–5 in all 4 limbs except for 3 in his right C8 and L4 myotomes and 2 in his right T1 myotome. His radiographic images at follow up showed stable implants and no screw loosening. He was largely ambulating with a walking frame at home. There was an improvement in his subsequent follow up at 1 year after his operation, his power was mostly 4–5 in all 4 limbs except for 3 in his right T1 myotome distribution. He was ambulating with a walking stick at home and regained the ability to write again (Figure 4).
“All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013).” Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Unilateral facet dislocations of the cervical spine constitute an important subgroup of cervical spine injuries. These are unstable fractures that often have coexisting spinal cord and nerve root injuries (10). The prevalence of disc herniations in CFD can range from 27% to 56% (11,12). In addition, these injuries are a common occurrence that often require surgical fixation, however there is no consensus on the optimal treatment (13).
The options for surgical fixation include the anterior approach, posterior approach and combined approach. These have their advantages and disadvantages, and their application varies depending on the injury sustained. The anterior approach is commonly utilised for anterior disc herniations or vertebral body fragments displacing into the spinal canal (14,15). The advantages of the anterior approach include tackling anterior disc herniations, technical ease and familiarity, relative short fusion construct, good stability, maintaining lordosis, less surgical trauma, and less perioperative pain (7,13,16,17). The disadvantages of the anterior approach include higher rates of postoperative kyphosis, incomplete reduction, risks of dysphagia and oseophageal injury (7,16). The posterior approach is commonly used for open reduction of facet dislocations and in stabilising posterior ligamentous disruptions (16). The advantages of the posterior approach include increased stability with stronger constructs, better visualisation of the dislocation allowing for direct reduction, and avoiding oesophageal injury (7,14). The disadvantages of the posterior approach include longer operating durations, longer hospital stay, increased blood loss, increased infection rates, and ineffectiveness in tackling anterior cord compression due to disc herniations (7,17). The other alternative includes the combined approach which utilises the anterior approach followed by the posterior approach. This provides the strongest fixation, significantly limits motion, and increases fusion rate (7). The disadvantage of the combined approach include a longer operative time, and increased morbidity (7). In our case, we utilised the combined anterior-posterior approach to achieve decompression from the herniated disc anteriorly and to also attain a stronger fixation posteriorly given the high energy trauma with a three column Injury.
While many other studies have shown minimal differences in outcomes between the anterior and posterior approach, the anterior approach alone for CFD is becoming increasingly accepted in the literature (13,14,17). A systemic review by Lee et al. in 2020 looked at the anterior approach for CFD and showed its efficacy, safety, and low revision rate (18). There were no occurrences of non-union or new neurological deficits in these cases. Sethy et al. studied 19 patients with facet dislocation managed by ACDF or anterior cervical corpectomy and fusion (ACCF) alone and concluded that the anterior approach is an effective treatment with good patient-reported outcomes, structural stability, and less blood loss (19). In their study, there was an improvement of mean segmental kyphosis angle from 12.2°±4.4° at presentation to −7.2°±2.5°, with improvement in the visual analogue scale, Oswestry Disability Index, and spinal cord independence measure score. Only 1 patient in the ACDF group needed secondary posterior fixation for instability due to difficulty with facetal reduction. Fortunately, the anterior approach was utilised first in our patient. This allowed us to discover the intradural disc herniation even though it was not obvious on the cervical spine MRI. Through this approach, we were able to achieve good decompression and tackle the underlying issue.
Intradural herniations can pose a challenge in the operative management of CFD. Lee et al. described their protocol of managing CSF leaks from cervical spinal traumas (20). The damaged PLL in these settings were not resected to avoid worsening the instability of the cervical spine, furthermore dural repair and duroplasty were not performed due to the wide and rough defect of the dura. Crutcher et al. studied patients with cervical spine gunshot injuries with CSF leakage and advocated against dural primary closure due to the significant amount of devitalised tissue and risks of infection (21). Wound drains were inserted during closure and were removed within 24 hrs if there was accumulation of CSF to prevent over drainage of CSF, pneumocephalus, and meningitis (20). Accumulations of CSF in the subcutaneous tissue were treated conservatively unless there was airway compromise. In addition, Feng et al. described using a vacuum sealing device (VSD) for unrepaired dural tears to aid with cavity shrinkage and wound healing (22). However, there have been reports that VSD may result in worsening CSF leakage and hinder dural healing (23). Other measures of managing dural herniations include bed rest, propping the patient’s head up to 30°, and continuing with prophylactic antibiotics (22,24,25). Lee et al. reported contrasting post-operative management techniques, whereby patients were not given bed rest and encouraged to mobilise (20). There were no CSF related complications like fluid collection, wound dehiscence, meningitis, and pseudomeningocele in these patients (20). In our case, we present a unique case of a CSF leak as a result of an intradural disc herniation. To our knowledge, this has not been reported in the literature previously. Our patient had a lantern drain inserted for 3 days, was propped up in bed to 30°, and was not able to ambulate initially, ultimately, he had a good recovery from his injury.
One limitation of our case report was that it only involved a short term 1 year follow up of the patient. Having a longer term follow up will allow us to accurately evaluate the outcomes of the surgical intervention. Our case was unique in the sense that no large disc herniation was seen in the pre-operative MRI, hence a single posterior approach could theoretically have been utilised. It is known in the literature that intradural disc herniation can be difficult to diagnose with MRI alone and can be concealed as minor disc herniation (26,27). If a posterior approach alone was chosen, it is likely that the intradural disc herniation would have been missed, therefore leading to residual disc fragments in the dura with persistent neurological deficits. We would like to highlight yet another benefit of approaching facet dislocations from the anterior approach first, which can be useful to address the disc herniations that are not obvious on initial MRI scans.
Conclusions
We described a unique case of a unilateral CFD with a traumatic intradural tear. While there are various techniques to treat this injury, we highlight the utility of the anterior approach in allowing the clinician to tackle intradural disc herniations that are not clearly seen on the preoperatively MRI scan. In addition, the anterior approach alone is also becoming an increasingly accepted technique for CFD surgery and the rationale for this is discussed.
Patient perspective
The patient was intoxicated upon arrival and but was able to consent for surgery once he was sober. He had surgery done the 2nd day of admission. Post-operatively, he was unable to walk and had little power in his lower limbs. During his recovery process in hospital, he described having little confidence in walking with physiotherapists due to his poor strength. He also described having cold sensations in his lower limb which gradually improved during his course of rehabilitation. He is glad to have regained back near full power in his lower limbs and is able to walk at home with a walking stick.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-21-106/rc
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-21-106/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. “All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013).” Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dvorak M, Vaccaro AR, Hermsmeyer J, et al. Unilateral facet dislocations: is surgery really the preferred option? Evid Based Spine Care J 2010;1:57-65. [Crossref] [PubMed]
- Chakravarthy V, Mullin JP, Abbott EE, et al. Neurologically intact patient following bilateral facet dislocation: case report and review of literature. Ochsner J 2014;14:108-11. [PubMed]
- Miao DC, Qi C, Wang F, et al. Management of severe lower cervical facet dislocation without vertebral body fracture using skull traction and an anterior approach. Med Sci Monit 2018;24:1295-302. [Crossref] [PubMed]
- Ivancic PC, Pearson AM, Tominaga Y, et al. Mechanism of cervical spinal cord injury during bilateral facet dislocation. Spine (Phila Pa 1976) 2007;32:2467-73. [Crossref] [PubMed]
- Botolin S, VanderHeiden TF, Moore EE, et al. The role of pre-reduction MRI in the management of complex cervical spine fracture-dislocations: an ongoing controversy? Patient Saf Surg 2017;11:23. [Crossref] [PubMed]
- Feng G, Hong Y, Li L, et al. Anterior decompression and nonstructural bone grafting and posterior fixation for cervical facet dislocation with traumatic disc herniation. Spine 2012;37:2082-8. [Crossref] [PubMed]
- Lins CC, Prado DT, Joaquim AF. Surgical treatment of traumatic cervical facet dislocation: anterior, posterior or combined approaches? Arq Neuropsiquiatr 2016;74:745-9. [Crossref] [PubMed]
- Gagnier JJ, Kienle G, Altman DG, et al. The CARE guidelines: consensus-based clinical case reporting guideline development. BMJ Case Rep 2013;2013:bcr2013201554. [Crossref] [PubMed]
- Luszczyk MJ, Blaisdell GY, Wiater BP, et al. Traumatic dural tears: what do we know and are they a problem? Spine J 2014;14:49-56. [Crossref] [PubMed]
- Lifeso RM, Colucci MA. Anterior fusion for rotationally unstable cervical spine fractures. Spine (Phila Pa 1976) 2000;25:2028-34. [Crossref] [PubMed]
- Grant GA, Mirza SK, Chapman JR, et al. Risk of early closed reduction in cervical spine subluxation injuries. J Neurosurg 1999;90:13-8. [PubMed]
- Vaccaro AR, Falatyn SP, Flanders AE, et al. Magnetic resonance evaluation of the intervertebral disc, spinal ligaments, and spinal cord before and after closed traction reduction of cervical spine dislocations. Spine (Phila Pa 1976) 1999;24:1210-7. [Crossref] [PubMed]
- Kwon BK, Fisher CG, Boyd MC, et al. A prospective randomized controlled trial of anterior compared with posterior stabilization for unilateral facet injuries of the cervical spine. J Neurosurg Spine 2007;7:1-12. [Crossref] [PubMed]
- Brodke DS, Anderson PA, Newell DW, et al. Comparison of anterior and posterior approaches in cervical spinal cord injuries. J Spinal Disord Tech 2003;16:229-35. [Crossref] [PubMed]
- Ren C, Qin R, Li Y, et al. Anterior reduction and fusion for acute unilateral cervical facet dislocation without severe spinal cord injuries. J Clin Neurosci 2020;78:102-7. [Crossref] [PubMed]
- Duggal N, Chamberlain RH, Park SC, et al. Unilateral cervical facet dislocation: biomechanics of fixation. Spine (Phila Pa 1976) 2005;30:E164-8. [Crossref] [PubMed]
- Ren C, Qin R, Wang P, et al. Comparison of anterior and posterior approaches for treatment of traumatic cervical dislocation combined with spinal cord injury: Minimum 10-year follow-up. Sci Rep 2020;10:10346. [Crossref] [PubMed]
- Lee W, Wong CC. Anterior-alone surgical treatment for subaxial cervical spine facet dislocation: a systematic review. Global Spine J 2021;11:256-65. [Crossref] [PubMed]
- Sethy SS, Ahuja K, Ifthekar S, et al. Is anterior-only fixation adequate for three-column injuries of the cervical spine? Asian Spine J 2021;15:72-80. [Crossref] [PubMed]
- Lee SE, Chung CK, Jahng TA, et al. Dural tear and resultant cerebrospinal fluid leaks after cervical spinal trauma. Eur Spine J 2014;23:1772-6. [Crossref] [PubMed]
- Crutcher CL 2nd, Wilson JM, Morrow KD, et al. Management of cerebrospinal fluid leak from cervical gunshot wounds with external ventricular drainage: a small case series. J Surg Case Rep 2020;2020:rjaa484.
- Feng C, Qianqian S, Jianhua H, et al. Treatment experience for full-thickness wound dehiscence with cerebrospinal fluid leakage following posterior primary spine surgery: Three case reports. Medicine (Baltimore) 2019;98:e15126. [Crossref] [PubMed]
- Lei Y, Liu L, Du SH, et al. The use of a skin-stretching device combined with vacuum sealing drainage for closure of a large skin defect: a case report. J Med Case Rep 2018;12:264. [Crossref] [PubMed]
- Du YQ, Duan WR, Chen Z, et al. Risk factors and management of dural defects in anterior surgery for cervical ossification of the posterior longitudinal ligament. World Neurosurg 2018;111:e527-38. [Crossref] [PubMed]
- Hannallah D, Lee J, Khan M, et al. Cerebrospinal fluid leaks following cervical spine surgery. J Bone Joint Surg Am 2008;90:1101-5. [Crossref] [PubMed]
- Luo D, Ji C, Xu H, et al. Intradural disc herniation at L4/5 level causing cauda equina syndrome: a case report. Medicine (Baltimore) 2020;99:e19025. [Crossref] [PubMed]
- Hammad A, Geiger F, Redder A, et al. Concealed intradural disc herniation: a case report. Arch Clin Med Case Rep 2020;4:504-11. [Crossref]


