
Total en bloc spondylectomy in the treatment of postoperative chronic osteomyelitis: a case report
Introduction
Infection of the spine can appear after surgical procedures or de novo and this is an increasing problem (1) compromising the life of the patient, the stability of the spine, as well as the neurological function. Postoperative infection is one of the most dreaded complications of spinal fusion surgery. The incidence ranges from 1% to 4% in the lumbar area (2) and the number of cases to be treated is increasing, due to the higher number of surgeries performed. It poses a significant burden in terms of patient morbidity, so it is advisable to know the treatment options available (3).
According to the literature, early infection occurs in the first 30 postoperative days and usually presents with local signs (erythema, increased temperature, wound exudate, etc.). Late infection can occur up to years after surgery and typically presents with chronic pain, implant failure or no fusion, and bone loss. Both differ in clinical presentation and treatment strategy (3).
In early infections, the treatment of choice includes early surgical lavage and debridement, along with intense antibiotic therapy. Instrumentation and grafting should be maintained as segment stability promotes healing (2).
Late infections are usually caused by biofilm-producing pathogens, so the usual treatment of choice is debridement and removal of osteosynthesis material (2), also considering the extent of the lesion, the quality of fixation, patient comorbidities, and the pathogen involved (3). The anterior column is most commonly involved since the posterior elements are only affected in 5% of cases (4). In some patients, bone destruction caused by infection destroys the anterior support of the spine. Subsequently, an important kyphotic deformity can be developed causing pain and seriously compromising the neurological function. The reconstruction of this problem must reach two goals: to eradicate the necrotic and infected tissue and to obtain a correct spinal profile which is stable and with a good biological field that permits to obtain a solid fusion mass.
For this reason, many authors have recommended the posterolateral or double approach, anterior and posterior, to remove the infected and necrotic tissue, replacing it with implants and biological interfaces (5-9) but destruction by chronic infection affects the whole vertebral body and it is impossible to make a complete resection unless by an intralesional approach.
We present the case of a female patient who underwent T9-S1 instrumentation and developed chronic osteomyelitis secondary to spinal spondylodiscitis of T8-T9 with residual segmental kyphosis due to extensive anterior destruction. Treatment was performed by total en bloc spondylectomy of the affected segments following the Tomita technique (10). We present the following case in accordance with the CARE reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-22-14/rc).
Case presentation
Statement of informed consent
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Case
The patient is a 66-year-old woman, with no medical history of interest, who underwent multiple spinal procedures at another center, detailed below. In 2006, a primary L3-L4 fusion was performed due to spinal stenosis, extended in several surgical procedures to the T11-S1 segment by repeated failures at adjacent levels. The pain was poorly managed, so a medullary neurostimulation device was implanted. Finally, the T9-T11 segment was fixed after verifying instability.
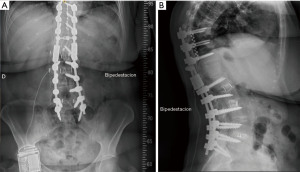
Six months after the last surgery the patient had daily fever and pain. The blood count showed leukocytosis with 81% polymorphonuclear cells and elevated C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). Plain radiographs showed angular thoracic kyphosis in T8-T9 secondary to disc destruction and mirror-image bone loss pattern of adjacent vertebrae (Figure 1A,1B).
Magnetic resonance imaging (MRI) and computerized axial tomography (CT) showed bone destruction and paravertebral involvement, diagnosed as osteomyelitis.
Blood cultures were positive for methicillin-resistant staphylococcus hominis and staphylococcus epidermidis. No intralesional samples were taken for culture. The preantibiotic sample blood test shown 7,300 leukocytes with an 81% of polymorphonuclear, CRP 21,25 (reference value <5) and an ESR of 32. Antibiotic treatment was performed for 3 months according to blood culture results. Blood analytical results returned to normal (CRP 6 and ESR 19), but the patient mentioned disabling chest pain not irradiated to the lower limbs and was referred to our center for evaluation. The preoperative visual analog scale (VAS) was 7/10.
Physical examination
Severe thoracic kyphosis was evident on inspection. The appearance of the surgical wound was good, with no signs of infection. Neurological examination was normal.
Complementary tests
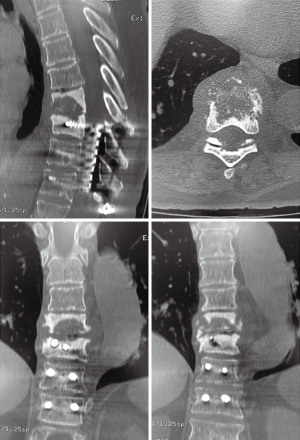
New imaging tests, MRI and CT scans, were performed and compared with previous studies. There was evidence of progression of spondylodiscitis at the T8-T9 level with extensive bone destruction in the anteroinferior portion of the T8 body, along with T9 screw displacement with osteolysis and collapse of the T8-T9 disc, without bone fusion (Figure 2). There was no epidural involvement.
Diagnosis
Chronic osteomyelitis secondary to spinal spondylodiscitis at the T8-T9 level and residual segmental kyphosis in a patient with T9-S1 instrumentation.
Surgical technique
Total en bloc spondylectomy of the affected segments T8-T9 was performed according to the Tomita technique (10).
In the prone position, through a posterior approach, caudal instrumentation was connected with in-line connectors for 5.5–6.35 up to two levels proximal to the vertebral resection.
Two-level en bloc spondylectomy was performed according to the Tomita technique (Figure 3) with bilateral preganglionic section of the T8-T9 roots. Complete discectomy of T7-8 and T9-10 was performed until obtaining a bleeding bed in the lower plate of T7 and upper plate of T10, last, implanting a titanium mesh with cancellous allograft. The final rods were placed and attached to previous instrumentation (Figure 4). During the procedure, the neurostimulator was not removed to avoid possible injury due to dural adhesions. The posterior cranial and caudal structures were scraped, and a cortico-cancellous bone allograft was placed over the posterior elements.
To finish the instrumentation in a favorable area in the sagittal plane, the spondylectomy area was reinforced with double-rod and finished with less rigid instrumentation in T4 using 5.5-mm titanium rods. The procedure was performed under neurophysiological control with no events, recording 600 cc of intraoperative bleeding that required the administration of two red blood cell concentrates in the postoperative period.
Postoperative evolution
After a 25-month follow-up, patient evolution has been favorable. The VAS score shows a 3/10 value. There were no complications in the postoperative period and radiographic control was satisfactory (Figure 5A,5B).

The microbiological study of the surgical specimen was negative for bacteria, fungi, and mycobacteria. Pathology revealed fibrosis, necrosis, and chronic inflammation compatible with chronic osteomyelitis, with no evidence of malignancy. With these results we opted for no antibiotic treatment.
No external orthosis was used in the postoperative period.
Currently, neurological examination and analytical results are normal, and the patient reports favorable pain control with analgesics from the first level of the World Health Organization.
Discussion
Traditionally, spinal infection has been treated using one or two surgical approaches aimed at removing the infectious focus and necrotic material, along with mechanical reconstruction of the area (5-9). The disadvantages of this procedure include using two surgical approaches and removing infected and necrotic tissue from the interior of the lesion, which is sometimes insufficient and causes surrounding contamination. Other authors (11) proposed to do it by a posterolateral approach with a radical debridement the ability to make an anterior and posterior reconstruction and a quicker recovery. The difference with the technique we propose is that the en bloc spondylectomy permits a radical resection of the whole affected area without violating the necrotic and infected tissue. This provides a safe and radical excision of the infected area (11-13). In patients with an acute infection, the ability to perform a surgery surrounding the infected tissue is lower and we have doubts using it in those kinds of patients.
In our patient, to avoid these adverse effects, necrotic and infected tissues were removed proceeding as if it were chronic osteomyelitis of long bones and performing en bloc resection with clear margins (14), that is, applying the criteria of oncological surgery to this chronic infection. This approach allows the complete and safe removal of infected and necrotic tissue, until reaching biologically viable healthy tissue in the vertebrae immediately cranial and caudal to the two healthy discs without entering the affected area. This technique has been reported as high-risk technique and with a high rate of complications (15). We have a very low rate of complications in oncologic patients avoiding a double approach and allowing the removal of all the necrotic or infected tissue.
After resection, the sagittal plane is reconstructed in the affected segment, restoring the normal distance between the two healthy vertebrae and the mechanical stability of the spine.
Total en bloc spondylectomy is a technically complex surgery, traditionally used to treat primary and metastatic vertebral tumors and not without major risks such as spinal injury or bleeding (10). In addition, multilevel vertebrectomy increases the risk of instability and is associated with a greater number of complications related to instrumentation, especially in the thoracic segment (16,17).
Despite the few studies on its use in cases of chronic vertebral osteomyelitis (17), it is an extensively described and well-known technique proven beneficial in our patient, allowing the treatment of infection and correction of angular thoracic kyphosis, reconstructing the sagittal plane, and providing the mechanical stability necessary to control infection and manage pain.
In our case, we consider infection has been controlled since all necrotic tissue has been removed and culture of the surgical specimen has been negative. We propose total en bloc spondylectomy as a reasonable treatment option in complicated spondylodiscitis progressing to extensive chronic osteomyelitis and compromising spinal stability due to a significant loss of bone material. To apply this oncologic designed technique to the infected spine permits experienced surgeons to reach the whole infected specimen while minimizing the possibility of contaminating the surrounding tissues doing suboptimal resections.
According to the available literature, adequate debridement of necrotic bone is of paramount importance for eradication of infection in chronic vertebral osteomyelitis. However, the role of total en bloc spondylectomy as treatment is yet to be defined. In our case, we achieved mechanical stability and the infection was eradicated. This may help to improve treatment outcome in patients in the future.
However, further studies may be required to develop a treatment algorithm for chronic vertebral osteomyelitis with use of this surgical technique.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-22-14/rc
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-22-14/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-22-14/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Butler JS, Shelly MJ, Timlin M, et al. Nontuberculous pyogenic spinal infection in adults: a 12-year experience from a tertiary referral center. Spine (Phila Pa 1976) 2006;31:2695-700. [Crossref] [PubMed]
- Chang CW, Fu TS, Chen WJ, et al. Management of Infected Transforaminal Lumbar Interbody Fusion Cage in Posterior Degenerative Lumbar Spine Surgery. World Neurosurg 2019;126:e330-41. [Crossref] [PubMed]
- Kowalski TJ, Berbari EF, Huddleston PM, et al. The management and outcome of spinal implant infections: contemporary retrospective cohort study. Clin Infect Dis 2007;44:913-20. [Crossref] [PubMed]
- Babinchak TJ, Riley DK, Rotheram EB Jr. Pyogenic vertebral osteomyelitis of the posterior elements. Clin Infect Dis 1997;25:221-4. [Crossref] [PubMed]
- Ruf M, Stoltze D, Merk HR, et al. Treatment of vertebral osteomyelitis by radical debridement and stabilization using titanium mesh cages. Spine (Phila Pa 1976) 2007;32:E275-80. [Crossref] [PubMed]
- Dimar JR, Carreon LY, Glassman SD, et al. Treatment of pyogenic vertebral osteomyelitis with anterior debridement and fusion followed by delayed posterior spinal fusion. Spine (Phila Pa 1976) 2004;29:326-32; discussion 332. [Crossref] [PubMed]
- Fukuta S, Miyamoto K, Masuda T, et al. Two-stage (posterior and anterior) surgical treatment using posterior spinal instrumentation for pyogenic and tuberculotic spondylitis. Spine (Phila Pa 1976) 2003;28:E302-8. [Crossref] [PubMed]
- Przybylski GJ, Sharan AD. Single-stage autogenous bone grafting and internal fixation in the surgical management of pyogenic discitis and vertebral osteomyelitis. J Neurosurg 2001;94:1-7. [PubMed]
- Fayazi AH, Ludwig SC, Dabbah M, et al. Preliminary results of staged anterior debridement and reconstruction using titanium mesh cages in the treatment of thoracolumbar vertebral osteomyelitis. Spine J 2004;4:388-95. [Crossref] [PubMed]
- Tomita K, Kawahara N, Baba H, et al. Total en bloc spondylectomy for solitary spinal metastases. Int Orthop 1994;18:291-8. [Crossref] [PubMed]
- Gorensek M, Kosak R, Travnik L, et al. Posterior instrumentation, anterior column reconstruction with single posterior approach for treatment of pyogenic osteomyelitis of thoracic and lumbar spine. Eur Spine J 2013;22:633-41. [Crossref] [PubMed]
- Purea T, Vettivel J, Hunt L, et al. Radiographic Features Associated With Increased Surgical Invasiveness in Pyogenic Vertebral Column Osteomyelitis. Global Spine J 2021;11:881-8. [Crossref] [PubMed]
- Skovrlj B, Guzman JZ, Caridi J, et al. Posterior-Only Circumferential Decompression and Reconstruction in the Surgical Management of Lumbar Vertebral Osteomyelitis. Global Spine J 2016;6:e35-40. [Crossref] [PubMed]
- Taki H, Krkovic M, Moore E, et al. Chronic long bone osteomyelitis: diagnosis, management and current trends. Br J Hosp Med (Lond) 2016;77:C161-4. [Crossref] [PubMed]
- Amendola L, Cappuccio M, De Iure F, et al. En bloc resections for primary spinal tumors in 20 years of experience: effectiveness and safety. Spine J 2014;14:2608-17. [Crossref] [PubMed]
- Yoshioka K, Murakami H, Demura S, et al. Risk factors of instrumentation failure after multilevel total en bloc spondylectomy. Spine Surg Relat Res 2017;1:31-9. [Crossref] [PubMed]
- Ackshota N, Nash A, Bussey I, et al. Outcomes of multilevel vertebrectomy for spondylodiscitis. Spine J 2019;19:285-92. [Crossref] [PubMed]




