
Spinal subarachnoid hemorrhage after percutaneous kyphoplasty: a case report and literature review
Introduction
Percutaneous balloon kyphoplasty (PBKP) is a standard procedure for the relief of pain caused by an osteoporotic vertebral compression fracture. Although PBKP is considered a minimally invasive treatment with a short duration of surgery, various complications and technical failures are known to occur (1). Among these, spinal intradural (subdural and subarachnoid) hematomas has extremely rarely been reported. Spinal intradural hematomas and bone cement leaks that can occur during PBKP are among the most serious iatrogenic complications. Symptoms might appear immediately after the procedure or several days later. These include severe neurologic symptoms that could be effectively managed with prompt surgery. Prevention is of utmost importance because complication can be very serious. There are very few reports of cases similar to the present case in the literature (2). We report a case of subarachnoid hemorrhage, and based on previous studies, we identify points to be noted and discuss preventive measures. We present the following case in accordance with the CARE reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-22-60/rc).
Case presentation
After a fall, an 80-year-old, slightly thin patient visited a hospital for low back pain and was diagnosed with a subacute compression fracture at L1. His medical history included chronic obstructive pulmonary disease, type 2 diabetes mellitus, hyperuricemia, and dyslipidemia, however he was not on antiplatelet or anticoagulant medications. The low back pain was resistant to medical treatment, and the patient underwent PBKP of L1. Subsequently, PBKP of T12 was performed as an additional treatment for prolonged back pain that did not improve with treatment at a local hospital. There were no complications during the first 2 days after the surgery. However, 2 days later, he developed paralysis of both lower limbs. The patient could not be treated at other hospitals and was referred to our hospital for emergency treatment.
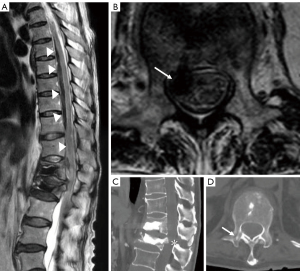
Magnetic resonance imaging revealed a massive intradural hematoma ventral to the spinal cord from thoracic spine T5 to T12 (Figure 1A,1B). Computed tomography (CT) showed that the vertebral body was filled with cement after percutaneous kyphoplasty (Figure 1C). However, at the T12 level, a percutaneous kyphoplasty entry pathway was found from the right pedicle, which seemed to have been through the spinal canal (Figure 1D). Spinal canal stenosis was observed at the T12/L1 level; below L1, the spinal fluid signal was confirmed, and no hematoma was observed.
Physical examination on admission revealed complete paralysis of the lower body (MMT 0/5) with loss of temperature and pain sensation below T11. Due to the difficulty in inserting a urinary catheter, bladder function could not be assessed. The patient had a loss of sensation around the anal area and complete paralysis of the anal sphincter. The intraspinal pressure was thought to be significantly increased, and significant spinal cord compression was suspected.
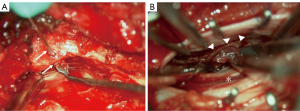
The patient underwent surgery in the prone position under general anesthesia. A bilateral laminectomy was performed from T11 to L1. The lamina and yellow ligaments were incised, exposing the dura mater. There was no epidural hematoma, and a tight dura was noted. The right pedicle at T12 was observed, and a small foramen was clearly seen near the pedicle, probably through the spinal canal (Figure 2A). The dura was incised from T11 to T12. There was no subdural hematoma, but a tense arachnoid was visible, and a spinal subarachnoid hematoma was observed at this point. The arachnoid was incised, and the hematoma was removed from around the cauda equina with careful washing (Figure 2B). Once the hematoma was removed, the flow of the spinal fluid was observed from the cranial side, indicating that adequate decompression was achieved. The dura was closed using absorbable sutures.
Postoperative images indicated adequate decompression, and neurological signs showed considerable improvement. Motor function improved from complete paraplegia to MMT4/5 in the lower limbs. The patient’s recovery was good, and he was able to ambulate with a walker. Finally, the patient was transferred to a rehabilitation hospital.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
PBKP has been frequently performed for osteoporotic vertebral fracture (OVF) in recent years and is widely recognized as a minimally invasive procedure. The incidence of OVF is the highest among osteoporosis-related fractures, and it has been proven that repeated OVF leads to decreased quality of life and increased mortality. The 5-year survival rate for patients clinically diagnosed with vertebral fractures is reported to be about 28%, which is higher than that for hip fractures (3). PBKP is a surgical procedure that usually has satisfactory results, including low risk of complications and decrease in pain, when performed carefully and for appropriate indications. Complications associated with vertebroplasty (VP) include cement leak, pulmonary embolism, infection, epidural hematoma (4), and vertebral fracture, which are not uncommon. There have been many reports of leakage of bone cement into and out of the dura mater (5-7), epidural hematoma, and intradural hematoma related to the conventional VP method (8-11). PBKP, a modified form of VP, has therapeutic advantages such as correction of local kyphosis and a low risk of cement leakage due to lower cementing pressure.
Since the introduction of PBKP, there have been reports of bone cement leaks (12,13), but no serious cases have been reported. There have been sporadic reports of epidural hematomas (7) and only one case of subarachnoid hematoma has been reported (2). We summarized previous reports of spinal intradural hematoma after percutaneous kyphoplasty or VP (Table 1). The low incidence of postoperative epidural and intradural hematoma suggests that PBKP is superior to VP in terms of safety. Previously medically-induced spinal subarachnoid hematoma due to lumbar puncture has been reported, and the mechanism is remarkably similar to that of the subarachnoid hemorrhage associated with PBKP in the present case. Puncture of the outermost layer of the dura during lumbar puncture has a risk of injury to the radial artery and vein, and might be a possible cause of iatrogenic spinal subarachnoid hematoma. In the present case, the source of the hematoma was identified as the radial artery or vein based on the presence of a hematoma mass and contusion of the nerve tissue near the T12 nerve root. Considering the imaging and intraoperative findings, we concluded that the cause of the subarachnoid hematoma was a medial deviation of the needle in the pedicle, a simple error associated with the procedure. When the bleeding is massive and rapid or normal dilution is mechanically impeded, it can lead to a frank hematoma (14).
Table 1
| Author | Age, gender | Type of hematoma | Fracture level | Cause of fracture | Initial treatment |
SIH onset |
Symptoms | SIH level |
Additional treatment | Result |
|---|---|---|---|---|---|---|---|---|---|---|
| Cosar et al. (8) | 18 yr, male | SDH | L2-L4 | Traumatic | Vertebroplasty | 12 hours | Paraparesis | T1-L2 | Hemilaminectomy T1-L2 | Good |
| Cosar et al. (8) | 75 yr, female | SDH | L1 | Osteoporotic | Vertebroplasty | 12 hours | Paraparesis | T12-L3 | Laminectomy T12 | Good |
| Lee et al. (9) | 40 yr, female | SDH | T11-T12 | Traumatic | Vertebroplasty | 2 weeks | Back pain | T10-L5 | Conservative | Good |
| Mattei et al. (10) | 49 yr, female | SDH | T8 | Traumatic | Vertebroplasty | Immediate | Nomoparesis | C7-T9 | Laminectomy T7-T9 | Good |
| Tropeano et al. (11) | 63 yr, male | SDH | L1-L3 | Oncological | Vertebroplasty | 2 weeks | Paraparesis | conus | Laminectomy L2-L3 | Good |
| Becker et al. (12) | 63 yr, male | SAH | T12 | Osteoporotic | Kyphoplasty | 2 days | Complete pareplegia | T8-L3 | Laminectomy T8-L3 | Good |
| Our case | 80 yr, male | SAH | T12, L1 | Osteoporotic | Kyphoplasty | 2 days | Complete pareplegia | T5-T12 | Laminectomy T11-L1 | Good |
SIH, spinal intradural hematoma; SDH, spinal subdural hematoma; SAH, spinal subarachnoid hematoma.
The most difficult part of the PBKP procedure is the process from the puncture of the needle to the placement of the introducer. Although needle puncture in two directions with C-arm fluoroscopy is usually recommended, it can also be performed with single-plane fluoroscopy. Before initiating the procedure, it is important to clearly delineate the right and left pedicle with anteroposterior (A-P)fluoroscopy and align the spinous processes in the middle of the cortical lines inside the pedicle on both sides. The needle is inserted into the pedicle under A-P fluoroscopy, and the needle tip is placed into the vertebral body in the lateral view before passing through the medial cortex of the pedicle, thus preventing the needle from entering the spinal canal. Once the introducer is placed within the vertebral body, it is then essential to precisely check the position of the posterior wall of the vertebral body with the lateral C-arm to prevent the slowly injected cement from leaking into the spinal canal. We are confident that compliance with these important aspects will prevent complications such as bone cement leakage and hematoma in the spinal canal. In some cases, it is difficult to visualize the inside of the pedicle on fluoroscopy, such as in patients with morbidity obesity or patients who originally have atrophic pedicles at the level of the upper lumbar vertebrae.
The likelihood of intradural hematoma associated with PBKP is estimated to be comparable to the risk of percutaneous pedicle screw (PS) insertion. The reported rates of misplacement of thoracic and lumbar PSs percutaneously placed under 2D fluoroscopy range from 8% to 40%, and a study among 502 cases, three had a medial deviation of the PS, and one of them required revision surgery (15). Although lateral deviation of the percutaneous PS is usually reported more frequently, Spitz et al. (16) reported an overall accuracy of 96.7% in their report of percutaneous PS without a guidewire. In one case of grade 3 deviation, the patient had osteoporosis, and the screw insertion site was confirmed to be inside the original hole formed by the pedicle probe, and medial deviation was also noted. If the cortex of the medial side of the pedicle is fractured due to advanced osteoporosis, the needle might stray into the spinal canal: hence it is advisable to consider modifying the technique by limiting it to the contralateral side. If the internal plane of the pedicle cannot be cleanly delineated on A-P fluoroscopy, penetration of the pedicle using CT-based navigation or other safeguards is necessary. Umebayashi et al. (17) reported that 3D fluoroscopic PBKP can safely increase the injection volume of polymethyl methacrylate (PMMa) compared to the usual C-arm 2D method. In PBKP, the use of safety tools such as CT-based or robot-assisted navigation should be pre-planned in cases with poor pedicle delineation on C-arm fluoroscopy.
In conclusion, early management of a patient with complete paralysis of the lower extremities due to a spinal subarachnoid hematoma associated with complications of PBKP resulted in a favorable neurological outcome. Percutaneous surgery through the pedicle might cause hematoma and bone cement leakage into the spinal canal. This can be a serious complication: hence prevention is important.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-22-60/rc
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-22-60/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-22-60/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Saliou G, Rutgers DR, Kocheida EM, et al. Balloon-related complications and technical failures in kyphoplasty for vertebral fractures. AJNR Am J Neuroradiol 2010;31:175-9. [Crossref] [PubMed]
- von der Brelie C, Fiss I, Rohde V. Multilevel Spinal Combined Subdural/Subarachnoid Hemorrhage Resulting in Paraplegia: An Unusual Complication of Kyphoplasty. J Neurol Surg A Cent Eur Neurosurg 2019;80:220-2. [Crossref] [PubMed]
- Johnell O, Kanis JA, Odén A, et al. Mortality after osteoporotic fractures. Osteoporos Int 2004;15:38-42. [Crossref] [PubMed]
- Kreppel D, Antoniadis G, Seeling W. Spinal hematoma: a literature survey with meta-analysis of 613 patients. Neurosurg Rev 2003;26:1-49. [Crossref] [PubMed]
- Chen YJ, Tan TS, Chen WH, et al. Intradural cement leakage: a devastatingly rare complication of vertebroplasty. Spine (Phila Pa 1976) 2006;31:E379-82. [Crossref] [PubMed]
- Sabuncuoğlu H, Dinçer D, Güçlü B, et al. Intradural cement leakage: a rare complication of percutaneous vertebroplasty. Acta Neurochir (Wien) 2008;150:811-5. [Crossref] [PubMed]
- Park SY, Modi HN, Suh SW, et al. Epidural cement leakage through pedicle violation after balloon kyphoplasty causing paraparesis in osteoporotic vertebral compression fractures - a report of two cases. J Orthop Surg Res 2010;5:54. [Crossref] [PubMed]
- Cosar M, Sasani M, Oktenoglu T, et al. The major complications of transpedicular vertebroplasty. J Neurosurg Spine 2009;11:607-13. [Crossref] [PubMed]
- Lee KD, Sim HB, Lyo IU, et al. Delayed onset of spinal subdural hematoma after vertebroplasty for compression fracture: a case report. Korean J Spine 2012;9:285-8. [Crossref] [PubMed]
- Mattei TA, Rehman AA, Dinh DH. Acute Spinal Subdural Hematoma after Vertebroplasty: A Case Report Emphasizing the Possible Etiologic Role of Venous Congestion. Global Spine J 2015;5:e52-8. [Crossref] [PubMed]
- Tropeano MP, La Pira B, Pescatori L, et al. Vertebroplasty and delayed subdural cauda equina hematoma: Review of literature and case report. World J Clin Cases 2017;5:333-9. [Crossref] [PubMed]
- Becker S, Meissner J, Tuschel A, et al. Cement leakage into the posterior spinal canal during balloon kyphoplasty: a case report. J Orthop Surg (Hong Kong) 2007;15:222-5. [Crossref] [PubMed]
- Abdelgawaad AS, Ezzati A, Govindasamy R, et al. Kyphoplasty for osteoporotic vertebral fractures with posterior wall injury. Spine J 2018;18:1143-8. [Crossref] [PubMed]
- Pai SB, Krishna KN, Chandrashekar S. Post lumbar puncture spinal subarachnoid hematoma causing paraplegia: a short report. Neurol India 2002;50:367-9. [PubMed]
- Heintel TM, Berglehner A, Meffert R. Accuracy of percutaneous pedicle screws for thoracic and lumbar spine fractures: a prospective trial. Eur Spine J 2013;22:495-502. [Crossref] [PubMed]
- Spitz SM, Sandhu FA, Voyadzis JM. Percutaneous "K-wireless" pedicle screw fixation technique: an evaluation of the initial experience of 100 screws with assessment of accuracy, radiation exposure, and procedure time. J Neurosurg Spine 2015;22:422-31. [Crossref] [PubMed]
- Umebayashi D, Yamamoto Y, Nakajima Y, et al. Balloon Kyphoplasty under Three-dimensional Radiography Guidance. Neurol Med Chir (Tokyo) 2017;57:489-95. [Crossref] [PubMed]


