
Lumbar spine surgery reduces postoperative opioid use in the veteran population
Introduction
The United States (U.S.) has been experiencing a growing nationwide opioid crisis since the turn of the 21st century (1). The opioid crisis has come to the forefront of nationwide discussion especially during the past 6 years, and between January 2016 and June 2020 the U.S. mobilized $7.5 billion in response to the crisis (2). Despite this level of funding, opioid related deaths continue to rise, with 75,673 deaths recorded during the 12-month period ending in April 2021 compared to 56,064 deaths during the same period one-year prior (3). Institutional, state, and federal policies aimed at curbing opioid overprescribing have also been implemented in response (4). Pain management can be particularly challenging when dealing with lumbar spine pathology. Gerbershagen et al. demonstrated that spinal surgery was associated with one of the highest patient-reported pain scores of all procedures (5). As a result, pain management after spine surgery can be challenging and can require multimodal analgesia even beyond the postoperative period (6,7).
The U.S. veteran population is a large group which encompassed 20.3 million people in 2018 (8). This group has been demonstrated to have a higher burden of mental health comorbidities including post-traumatic stress disorder (PTSD), depression, anxiety, and substance abuse compared to the general population which makes opioid management more difficult and managing surgical outcomes more complex (9). These conditions have been independently associated with increased mortality in this vulnerable population even decades after the end of their service (10-12). Alcohol, opioids, and other substance abuse have also been demonstrated to be associated with an increased risk for homelessness and all-cause mortality in the veteran population (13,14).
Considering the large number of veterans who undergo lumbar surgery seeking to improve function and decrease pain, we set out to examine if having lumbar spine surgery would help this vulnerable population decrease their pain medication requirements postoperatively. We also examined the effect that opioid exposure prior to surgical intervention has on the proportion of patients who remain on opioids at one year postoperatively. Finally, we evaluated the percentage of opioid naive patients who were unable to discontinue opioids after their lumbar spine procedure. We present the following article in accordance with the STROBE reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-22-50/rc).
Methods
Data source and study design
Patient records were queried from the administrative claims database known as the Veterans Affairs Informatics and Computing Infrastructure (VINCI). The database contains deidentified patient data from the inpatient and outpatient settings of the Veterans Affairs (VA) healthcare system. Researchers extracted data using Current Procedural Technology (CPT) and International Classification of Diseases, Ninth and Tenth revision (ICD-9/ICD-10) codes. Data were queried from the period beginning January 1, 2010 to December 31, 2020. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study received Institutional Review Board (IRB) exemption from the Southeast Louisiana Veterans Health Care System (SLVHCS) IRB (registration #IRB00008177) (study ID #781) and the SLVHCS Research and Development Committee (study ID #781).
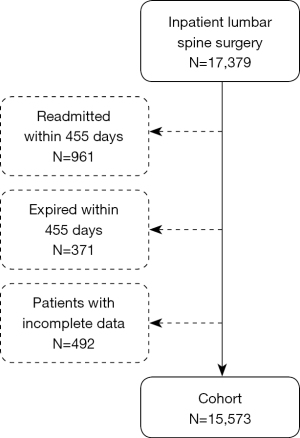
A retrospective cohort study was conducted to evaluate trends in opioid cessation among patients undergoing lumbar spine surgery. Patients were initially identified based on the presence of CPT codes 63005, 63011, 63012, 63030, 63042, and 63047 for lumbar decompression. Patients included in the cohort included patients who underwent decompression alone as well as patients who underwent decompression with fusion and all data was for inpatient procedures (Table S1). Patients who were readmitted within 455 days of initial admission were then excluded in order to minimize bias for postoperative opioid use due to another medical condition which necessitated readmission. Patients who expired within 455 days of initial admission and patients with incomplete data for any variable of interest were also excluded (Figure 1).
Baseline demographic data were obtained for all patient cohorts including age, sex, race, and year of lumbar spine surgery. Clinical characteristics obtained included length of stay (LOS) during the primary spine procedure, and the prevalence of diabetes mellitus, tobacco use, obesity, and other comorbidities is listed in Table 1. Comorbidities and complications were defined using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) and Tenth Revision (ICD-10-CM) codes as previously described by Elixhauser et al. and Quan et al. (15,16). Patients were then stratified into three groups based on preoperative opioid usage within the 365 days prior to the procedure: (I) opioid-naive (zero claims); (II) low usage (one to three claims); and (III) high usage (four or more claims). A claim is each instance that a patient filled a prescription for an opioid and the claim includes information on type of opioid, strength, and quantity for both inpatient and outpatient records. For groups (II) and (III), the proportion of patients with at least one postoperative opioid claim was calculated for four distinct postoperative time periods: (I) 0 to 30 days; (II) 31 to 90 days; (III) 91 to 180 days; and (IV) 181 to 365 days. Postoperative analysis was taken to day 455 in order to evaluate for 365 days beyond what was chosen to be the acute postoperative pain period of 90 days. Generic drug codes for the most commonly prescribed transdermal and oral opioid medications were used to quantify the number of patients who filed at least one opioid claim during each postoperative time interval. The list of opioids included are included in Table S2. Cumulative opioid usage for each patient was calculated as morphine milligram equivalents (MME) as outlined by the Center for Disease Control and Prevention (CDC) (17).
Table 1
| Characteristics | Opioid naive (n=7,671) | 1–3 prior claims (n=3,656) | >3 prior claims (n=4,246) | P value |
|---|---|---|---|---|
| Age (years), mean ± SD | 66.5±13.0 | 65.0±13.9 | 65.9±11.6 | <0.001* |
| Male sex, n (%) | 7,220 (94.1) | 3,428 (93.8) | 3,944 (92.9) | 1 |
| Fusion | 1,272 (16.6) | 559 (15.3) | 898 (21.1) | <0.001* |
| Number of levels with instrumentation | ||||
| Single level | 471 (6.1) | 213 (5.8) | 328 (7.7) | 0.027* |
| 3–6 levels | 562 (7.3) | 251 (6.9) | 403 (9.5) | <0.001* |
| 7–12 levels | 37 (0.5) | 11 (0.3) | 16 (0.4) | 1 |
| Race, n (%) | ||||
| White | 6,150 (80.2) | 2,937 (80.3) | 3,426 (80.7) | 1 |
| Black | 979 (12.8) | 477 (13.0) | 529 (12.5) | 1 |
| Asian | 43 (0.6) | 22 (0.6) | 8 (0.2) | 0.301 |
| Native | 72 (0.9) | 29 (0.8) | 35 (0.8) | 1 |
| Other | 427 (5.6) | 191 (5.2) | 248 (5.8) | 1 |
| Comorbidities, n (%) | ||||
| Tobacco | 851 (11.1) | 436 (11.9) | 682 (16.1) | <0.001* |
| Obesity | 666 (8.7) | 317 (8.7) | 356 (8.4) | 1 |
| Hypertension | 3,146 (41.0) | 1,453 (39.7) | 1,798 (42.3) | 1 |
| Diabetes mellitus | 1,281 (16.7) | 607 (16.6) | 733 (17.3) | 1 |
| Depression | 680 (8.9) | 347 (9.5) | 470 (11.1) | 0.021 |
| PTSD | 676 (8.8) | 362 (9.9) | 426 (10.0) | 1 |
| Anxiety | 266 (3.5) | 130 (3.6) | 157 (3.7) | 1 |
| Substance use disorder | 1,005 (13.1) | 520 (14.2) | 743 (17.5) | <0.001* |
| CCI, mean ± SD | 3.0±1.9 | 2.9±2.0 | 2.9±1.8 | 0.050 |
| Length of stay (days), mean ± SD | 4.4±11.9 | 4.8±16.9 | 4.4±11.6 | 0.306 |
*, P values indicate statistically significant results. SD, standard deviation; PTSD, post-traumatic stress disorder; CCI, Charlson comorbidity index.
Statistical analysis
All analyses were conducted using R statistical software (R Foundation for Statistical Computing, Vienna, Austria) with a significance level of 0.05. To compare baseline demographics of the cohorts, chi square test was used for categorical variables and Anova was used for continuous variables. The Cochran-Armitage test was used to perform trend analysis of opioid usage following lumbar surgery. For each stratified group, the distribution of cumulative MME was assessed using the Shapiro-Wilk normality test, which confirmed non-normality. The paired Wilcoxon signed rank test was subsequently used to compare cumulative preoperative MME (between days −365 and 0) to cumulative postoperative MME (between days 91 and 455). Multivariable logistic regression controlling for which controlled the significant differences between the cohorts including age, gender, race, year, tobacco use, obesity, hypertension, diabetes mellitus, depression, substance use disorder, anxiety, fusion, and number of levels treated was used to determine associations between covariates and opioid usage onwards of postoperative day 90 which was chosen as the acute pain period (as defined by at least 1 fill between postoperative days 91 and 455). Mann Whitney U test was used to compare cumulative MME from years 2010–2015 to cumulative MME from years 2016–2020. Chi square test was used to compare 30-day complication rates between the opioid naive, low preoperative opioid usage, and high preoperative opioid usage groups.
Results
Study populations
A total of 17,397 veterans who underwent lumbar spine surgery were identified. Of these 961 were excluded for readmission, 371 were excluded for expiring within 455 days, and 492 patients were excluded for incomplete data (Figure 1). After applying exclusion criteria, a total of 15,573 veterans who underwent lumbar surgery were identified. Of the 15,573 patients in the cohort, 93.7% were male and 80.4% were white. The three cohorts were significantly different in age, percentage undergoing fusion, number of levels with instrumentation, tobacco use, and substance use disorder. The follow-up period was 455 days for all patients. Regarding preoperative opioid usage, 7,671 (49.3%) were opioid-naive, 3,656 (23.5%) had low preoperative opioid claims, and 4,246 (27.3%) had high preoperative opioid claims. LOS was not significantly different between the three cohorts (P=0.306) (Table 1).
Postoperative opioid usage by group
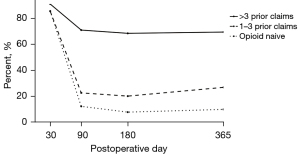
The proportion of patients in the high preoperative opioid claims group with at least one opioid claim dropped from 91.0% at postoperative day 30 to 69.4% by postoperative day 365. The proportion of patients in the low preoperative claims group dropped from 85.4% at postoperative day 30 to 26.9% at postoperative day 365. The proportion of patients in the opioid-naive group dropped from 85.6% at postoperative day 30 to 10.0% at postoperative day 365. Postoperative opioid claims rates were significantly different among the three groups at each timepoint (P<0.001) (Figure 2).
Median preoperative versus postoperative opioid MME by group
Median cumulative preoperative opioid consumption among all patients was significantly greater than median cumulative postoperative opioid consumption (P<0.001). Stratifying the cohort by preoperative opioid usage demonstrated a significantly larger postoperative MME compared to preoperative MME in the opioid naive group (P<0.001). Median postoperative MME was significantly lower than that of median preoperative MME for both the low (P<0.001) and high preoperative opioid groups (P<0.001) (Table 2). Preoperative opioid usage of more than 3 claims was the covariate most significantly associated with continued postoperative opioid usage [odds ratio 11.84, 95% confidence interval (CI): 10.87–12.89]. A history of depression (odds ratio 1.19, 95% CI: 1.04–1.35), substance use disorder (odds ratio 1.20, 95% CI: 1.05–1.38), and any surgical complication (odds ratio 1.20, 95% CI: 1.02–1.42) were also associated with continued postoperative opioid usage.
Table 2
| Groups | Preoperative median MME (median, IQR) |
Postoperative median MME (median, IQR) |
P value |
|---|---|---|---|
| All | 60 [0–1,935] | 0 [0–900] | <0.001* |
| Opioid naive | 0 [0–0] | 0 [0–0] | <0.001* |
| 1–3 prior claims | 450 [200–900] | 0 [0–376.9] | <0.001* |
| >3 prior claims | 6,641.3 [3,000–14,560] | 3,945 [225–12,986.3] | <0.001* |
*, P values indicate statistically significant results. MME, morphine milligram equivalent; IQR, interquartile range.
Yearly trends in preoperative opioid prescriptions and sustained postoperative use
The number of lumbar surgeries per year steadily declined from 1,700 in 2010 to 814 in 2020 (Figure 3A). During this same time period, the proportion of patients with preoperative opioid claims decreased (58.8% to 34.8%). The proportion of patients with opioid claims after postoperative day 90 also decreased from 43.8% to 19.8%. Notably, rates of both preoperative opioid claims and patients with sustained opioid use after postoperative day 90 dropped consistently after 2015 (Figure 3B). Median cumulative preoperative MME was also significantly higher between the years 2010 and 2015 compared to that of years 2016 to 2020 (P<0.001). Patients with low preoperative opioid claims (1–3 prior claims) had a 48.8% decrease in median cumulative preoperative MME between years 2010–2015 and 2016–2020 (P<0.001), while patients with high preoperative opioid claims (>3 prior claims) had a 15.2% decrease (P<0.001) (Table 3).
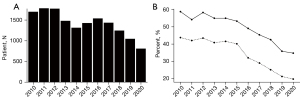
Table 3
| Groups | 2010–2015 (median, IQR) | 2016–2020 (median, IQR) | P value |
|---|---|---|---|
| All | 262.5 [0–3,150] | 0 [0–600] | <0.001* |
| Opioid naive | 0 [0–0] | 0 [0–0] | NA |
| 1–3 prior claims | 586.25 [250–1,095] | 300 [150–675] | <0.001* |
| >3 prior claims | 6,900 [3,150–15,027] | 5,850 [2,520–13,950] | <0.001* |
*, P values indicate statistically significant results. MME, morphine milligram equivalent; IQR, interquartile range.
Postoperative 30-day complications by opioid use
The opioid naive group had a lower overall complication rate (17.4%) compared to the low preoperative opioid usage group (18.9%) and the high preoperative opioid usage group (20.6%). Overall complication rate was significantly different between the three cohorts (P=0.012). Urinary tract infections (UTI) were also significantly different between the three cohorts (P=0.038). All other queried complications were statistically comparable between the cohorts (Table 4).
Table 4
| Complications, n (%) | Opioid naive (n=7,671) | 1–3 prior claims (n=3,656) | >3 prior claims (n=4,246) | P value |
|---|---|---|---|---|
| Any complication | 1,336 (17.4) | 691 (18.9) | 875 (20.6) | 0.012* |
| Wound infection | 104 (1.4) | 55 (1.5) | 81 (1.9) | 0.630 |
| Dural tear | 494 (6.4) | 244 (6.7) | 302 (7.1) | 1 |
| Pulmonary complication | 289 (3.8) | 142 (3.9) | 165 (3.9) | 1 |
| Cardiovascular complication | 95 (1.2) | 44 (1.2) | 45 (1.1) | 1 |
| Urinary tract infection | 182 (2.4) | 118 (3.2) | 141 (3.3) | 0.038* |
| Sepsis | 87 (1.1) | 39 (1.1) | 51 (1.2) | 1 |
| Pneumonia | 50 (0.7) | 31 (0.8) | 47 (1.1) | 0.335 |
*, P values indicate statistically significant results.
Discussion
This study demonstrated that there was a significant reduction in the postoperative MME compared to preoperative MME in both the low and high preoperative opioid groups following surgery supporting the value added in quality adjusted life years (18). At day 365, 30.6% of patients in the high preoperative group and 73.1% in the low preoperative group were no longer using opioids. The veteran population’s reduction in opioid use after lumbar spine surgery in preoperative opioid users is similar to prior studies of the general population. Dunn et al. demonstrated that 48.0% of patients in their study who used opioids preoperatively were able to discontinue them after surgery, while Warner et al. demonstrated that 77.8% of all patients undergoing spine surgery were able to successfully reduce their postoperative opioid use compared to preoperative (19,20). This affirms that despite being a high-risk population, the veteran population has a similar response to lumbar spine surgery as the general population in regards to postoperative opioid dependence. This also reinforces prior findings that lumbar spine surgery can be utilized to successfully reduce postoperative opioid use in patients who meet criteria for lumbar decompression.
There was a 24.0% decrease in the proportion of patients with any preoperative opioid claims from 2010 to 2020 and a significant decrease in median cumulative preoperative MME in 2016–2020 compared to 2010–2015. Postoperatively there was a concomitant overall 24% decrease in patients still using opioids beyond postoperative day 90. One possible explanation is the increasing focus and legislation targeting the opioid epidemic within the medical community. In 2017, the VA healthcare system guidelines for opioid prescribing changed in response to the growing epidemic (21). In 2020, the VA announced a 64% reduction in prescription opioid use among veterans through the implementation of these guidelines and other initiatives (22). Statewide legislation has also been shown to be effective in reducing opioid utilization. Reid et al. demonstrated a reduction in 30-day and 30- to 90-day postoperative cumulative MME prescribed after the implementation of laws limiting postoperative opioid prescriptions in 28 U.S. states (23). Several studies have demonstrated that even smaller single center initiatives such as preoperative counseling of patients on opioids is associated with a significant reduction in postoperative opioid use in both adult and adolescent orthopaedic patients (24,25).
While there was overall a large reduction in patients on opioids postoperatively in the high and low opioid groups, this study also demonstrated that greater preoperative opioid use was associated with a significantly increased risk of postoperative use beyond the immediate postoperative period (90–455 days). These results align with prior literature which has demonstrated greater preoperative opioid use to be a significant predictor of decreased postoperative opioid independence following spine surgery (26-29). This association is not limited to spine surgery and has also been demonstrated in other types of orthopaedic surgery including elective total joint arthroplasty (30). Brock et al. also demonstrated this increased risk for seven common orthopaedic procedures but found that for non-opioid naive patients a three-month opioid-free period before the procedures significantly decreased the risk of continued postoperative opioid use (31). Higher preoperative opioid usage was also associated with an increased risk of any complication and UTI. This association with preoperative opioid usage and postoperative complications has been demonstrated in several studies of different orthopaedic procedures including lumbar spine surgery (32-34). This increase in complications and UTI noted in this study and prior studies is possibly due to the immunomodulatory effect of opioids (35). Thus it may be advantageous for surgeons to engage in preoperative opioid counseling and attempt to get patients off opioids in the period leading up to surgery.
While there was a significant reduction in the percentage of patients still on opioids for the low and high preoperative opioid groups, it should be noted that the opioid naive group had 10.0% of patients still using opioids at day 365. Despite being the lowest percentage of the three groups, this demonstrates a notable 1 in 10 risk for opioid dependence in patients undergoing spine surgery who were opioid naive prior to the surgery. Opioid naive veterans in this study demonstrated a rate of postoperative opioid dependence that is within the range of these previous studies on the general population (19,36-38). Dunn et al. demonstrated a similar finding for opioid naive patients undergoing elective spinal fusion with 18.3% of patients in their study becoming opioid dependent postoperatively (19). Other studies on lumbar spine surgery have demonstrated between 2.0% and 7.5% of opioid naive patients becoming opioid dependent (36-38). As such, it is important for surgeons to consider emphasizing this risk in preoperative counseling of opioid naive patients as part of the informed decision-making process and implementing strategic time intervals for opioid reduction and cessation.
Limitations
There are several limitations in this study. First, claims data do not contain any information on the amount of the opioid prescription that patients actually take after filling it. Nor does this database include any information on opioids obtained and taken through illicit means or prescribed by a non-VA provider. Other analgesics were not queried in this study and over the counter analgesics (e.g., nonsteroidal anti-inflammatory drugs) are difficult to track. Thus, concomitant usage of other analgesics and their influence on opioid consumption postoperatively is not considered in this study. Additionally, the possibility of coding errors is inherent with any analysis of administrative claims data. However, such instances are rare and made up only 0.7% of Medicare and Medicaid payments in 2021 (39). One study of VA administrative data demonstrated that ICD-9 claims data had had generally high sensitivity, specificity, positive predictive value and negative predictive value. However, none of the data for the 9 diagnoses queried were 100% across all four statistical categories and one diagnosis had relatively low sensitivity of 42% (40). As such, because this analysis relied on claims data, it is possible that uncharted prescriptions and postoperative complications were not captured. Another limitation is that patients who were readmitted within 455 days of the initial admission were excluded from the study. This likely artificially decreased the number of postoperative complications observed in the study population as any individual that had a complication which required an inpatient readmission was excluded in the query. This also likely excluded patients who were more likely to need more opioids and for longer duration.
Conclusions
In the veteran population, lumbar spine surgery was effective in getting 50% of patients who were on opioids preoperatively to discontinue opioids postoperatively. 10% of patients who were opioid naive prior to a lumbar surgical procedure were still receiving opioids at one year post surgery which stresses the importance of opioid counseling preoperatively and effective weaning strategies in the postoperative period. Even minimal exposure to opioids preoperatively resulted in a 2.69-time increase in risk of being on opioids at one year versus opioid naive patients, stressing the importance of physician and patient education on the judicious use of opioids in a preoperative setting. This study affirms that despite being a high-risk population, the veteran population has a similar response to lumbar spine surgery as the general population in regards to opioid dependence.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-22-50/rc
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-22-50/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-22-50/coif). MC is a paid speaker for Medtronic, Stryker and ATEC. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dhalla IA, Persaud N, Juurlink DN. Facing up to the prescription opioid crisis. BMJ 2011;343:d5142. [Crossref] [PubMed]
- Gallo C, Abram K, Hannah N, et al. Sustainability planning in the US response to the opioid crisis: An examination using expert and text mining approaches. PLoS One 2021;16:e0245920. [Crossref] [PubMed]
- Drug Overdose Deaths in the U.S. Top 100,000 Annually [Internet]. 2021 [cited 2022 Jun 2]. Available online: https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2021/20211117.htm
- Lott A, Hutzler LH, Bosco JA 3rd, et al. Opioid Prescribing Patterns in Orthopaedic Surgery Patients: the Effect of New York State Regulations and Institutional Initiatives. J Am Acad Orthop Surg 2020;28:1041-6. [Crossref] [PubMed]
- Gerbershagen HJ, Aduckathil S, van Wijck AJ, et al. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology 2013;118:934-44. [Crossref] [PubMed]
- Yoo JS, Ahn J, Buvanendran A, et al. Multimodal analgesia in pain management after spine surgery. J Spine Surg 2019;5:S154-9. [Crossref] [PubMed]
- Nielsen RV, Fomsgaard JS, Dahl JB, et al. Insufficient pain management after spine surgery. Dan Med J 2014;61:A4835. [PubMed]
- Planning O of P and. Veteran Population - National Center for Veterans Analysis and Statistics [Internet]. [cited 2022 May 12]. Available online: https://www.va.gov/vetdata/veteran_population.asp
- Trivedi RB, Post EP, Sun H, et al. Prevalence, Comorbidity, and Prognosis of Mental Health Among US Veterans. Am J Public Health 2015;105:2564-9. [Crossref] [PubMed]
- Boscarino JA. Posttraumatic stress disorder and mortality among U.S. Army veterans 30 years after military service. Ann Epidemiol 2006;16:248-56. [Crossref] [PubMed]
- Bramsen I, Deeg DJ, van der Ploeg E, et al. Wartime stressors and mental health symptoms as predictors of late-life mortality in World War II survivors. J Affect Disord 2007;103:121-9. [Crossref] [PubMed]
- Zivin K, Ilgen MA, Pfeiffer PN, et al. Early mortality and years of potential life lost among Veterans Affairs patients with depression. Psychiatr Serv 2012;63:823-6. [Crossref] [PubMed]
- Chwastiak LA, Rosenheck RA, Desai R, et al. Association of psychiatric illness and all-cause mortality in the National Department of Veterans Affairs Health Care System. Psychosom Med 2010;72:817-22. [Crossref] [PubMed]
- Iheanacho T, Stefanovics E, Rosenheck R. Opioid use disorder and homelessness in the Veterans Health Administration: The challenge of multimorbidity. J Opioid Manag 2018;14:171-82. [Crossref] [PubMed]
- Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care 1998;36:8-27. [Crossref] [PubMed]
- Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 2011;173:676-82. [Crossref] [PubMed]
- Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain - United States, 2016. MMWR Recomm Rep 2016;65:1-49. [Crossref] [PubMed]
- Devin CJ, Chotai S, Parker SL, et al. A Cost-Utility Analysis of Lumbar Decompression With and Without Fusion for Degenerative Spine Disease in the Elderly. Neurosurgery 2015;77:S116-24. [Crossref] [PubMed]
- Dunn LK, Yerra S, Fang S, et al. Incidence and Risk Factors for Chronic Postoperative Opioid Use After Major Spine Surgery: A Cross-Sectional Study With Longitudinal Outcome. Anesth Analg 2018;127:247-54. [Crossref] [PubMed]
- Warner NS, Habermann EB, Hooten WM, et al. Association Between Spine Surgery and Availability of Opioid Medication. JAMA Netw Open 2020;3:e208974. [Crossref] [PubMed]
- Beam E. VA/DoD clinical practice guideline for opioid therapy for chronic pain. 2017;198. Available online: https://www.va.gov/HOMELESS/nchav/resources/docs/mental-health/substance-abuse/VA_DoD-CLINICAL-PRACTICE-GUIDELINE-FOR-OPIOID-THERAPY-FOR-CHRONIC-PAIN-508.pdf
- Affairs O of P and I. VA reduces prescription opioid use by 64% during past eight years [Internet]. [cited 2022 Jun 2]. Available online: https://www.va.gov/opa/pressrel/pressrelease.cfm?id=5492
- Reid DBC, Shah KN, Shapiro BH, et al. Mandatory Prescription Limits and Opioid Utilization Following Orthopaedic Surgery. J Bone Joint Surg Am 2019;101:e43. [Crossref] [PubMed]
- Vincent S, Paskey T, Critchlow E, et al. Prospective Randomized Study Examining Preoperative Opioid Counseling on Postoperative Opioid Consumption after Upper Extremity Surgery. Hand (N Y) 2022;17:200-5. [Crossref] [PubMed]
- Williams BA, Magee LC, Makarewich CA, et al. Preoperative Opioid Informed Consent and Prescribing Practices in Children Undergoing Orthopaedic Trauma Surgery. J Am Acad Orthop Surg Glob Res Rev 2022; [Crossref] [PubMed]
- Armaghani SJ, Lee DS, Bible JE, et al. Preoperative opioid use and its association with perioperative opioid demand and postoperative opioid independence in patients undergoing spine surgery. Spine (Phila Pa 1976) 2014;39:E1524-30. [Crossref] [PubMed]
- Schoenfeld AJ, Belmont PJ Jr, Blucher JA, et al. Sustained Preoperative Opioid Use Is a Predictor of Continued Use Following Spine Surgery. J Bone Joint Surg Am 2018;100:914-21. [Crossref] [PubMed]
- Montgomery EY, Pernik MN, Johnson ZD, et al. Perioperative Factors Associated With Chronic Opioid Use After Spine Surgery. Global Spine J 2021; Epub ahead of print. [Crossref] [PubMed]
- Kowalski C, Ridenour R, McNutt S, et al. Risk Factors For Prolonged Opioid Use After Spine Surgery. Global Spine J 2021; Epub ahead of print. [Crossref] [PubMed]
- Ross BJ, Wu VJ, Mansour AA 3rd, et al. Opioid Claims Prior to Elective Total Joint Arthroplasty and Risk of Prolonged Postoperative Opioid Claims. J Am Acad Orthop Surg 2021;29:e1254-63. [Crossref] [PubMed]
- Brock JL, Jain N, Phillips FM, et al. Postoperative opioid cessation rates based on preoperative opioid use: analysis of common orthopaedic procedures. Bone Joint J 2019;101-B:1570-7. [Crossref] [PubMed]
- Ridenour R, Kowalski C, Yadavalli A, et al. Preoperative Opioid Use Is Associated With Persistent Use, Readmission and Postoperative Complications After Arthroscopic Knee Surgery. Arthroscopy 2021;37:1567-72. [Crossref] [PubMed]
- Jain N, Phillips FM, Weaver T, et al. Preoperative Chronic Opioid Therapy: A Risk Factor for Complications, Readmission, Continued Opioid Use and Increased Costs After One- and Two-Level Posterior Lumbar Fusion. Spine (Phila Pa 1976) 2018;43:1331-8. [Crossref] [PubMed]
- Sing DC, Barry JJ, Cheah JW, et al. Long-Acting Opioid Use Independently Predicts Perioperative Complication in Total Joint Arthroplasty. J Arthroplasty 2016;31:170-174.e1. [Crossref] [PubMed]
- Ninković J, Roy S. Role of the mu-opioid receptor in opioid modulation of immune function. Amino Acids 2013;45:9-24. [Crossref] [PubMed]
- Goyal A, Payne S, Sangaralingham LR, et al. Incidence and risk factors for prolonged postoperative opioid use following lumbar spine surgery: a cohort study. J Neurosurg Spine 2021; Epub ahead of print. [Crossref] [PubMed]
- Karhade AV, Cha TD, Fogel HA, et al. Predicting prolonged opioid prescriptions in opioid-naive lumbar spine surgery patients. Spine J 2020;20:888-95. [Crossref] [PubMed]
- Wright AK, Sikora M, Leveque JC. Characterizing the Risk of Long-Term Opioid Utilization in Patients Undergoing Lumbar Spine Surgery. Spine (Phila Pa 1976) 2020;45:E54-60. [Crossref] [PubMed]
- 2021 Medicare Fee-for-Service Supplemental Improper Payment Data|CMS. Accessed June 11, 2022. Available online: https://www.cms.gov/httpswwwcmsgovresearch-statistics-data-and-systemsmonitoring-programsmedicare-ffs-compliance/2021-medicare-fee-service-supplemental-improper-payment-data
- Szeto HC, Coleman RK, Gholami P, et al. Accuracy of computerized outpatient diagnoses in a Veterans Affairs general medicine clinic. Am J Manag Care 2002;8:37-43. [PubMed]


