
Stent-armed kyphoplasty in osteoporotic thoracolumbar fractures—clinical and functional results and a center experience over 10 years
Introduction
Osteoporosis is a common disease of the elderly population and a major problem for the present and future of human health at a global level. This pathology leads to disorganization of bone microarchitecture, loss of density and deterioration of bone tissue, resulting in compromised strength and consequent increased risk of fractures (1-4). Vertebral compressive fractures are the end of the line for osteoporotic disease, as they occur at a late stage in the course of the disease. Although vertebral fractures are often underdiagnosed, they are also, paradoxically, the most frequent osteoporotic fractures (4-8). In the presence of porotic bone, vertebral fractures can occur spontaneously or in the course of traumatic events and allow us to foresee an increased risk of new fragility fractures in different locations (1,5,6). In fact, osteoporosis is clinically unapparent until the diagnosis of bone fragility fractures is reached and although a third of vertebral fractures have no clinical translation, thoracolumbar fractures can be the cause of significant pain and functional limitations, often associated with prolonged immobility periods with consequent worsening of other diseases and risk of vertebral collapse and neurological injury (1,4,5,9). In light of current knowledge, the ideal treatment for osteoporotic vertebral fractures is still a controversial topic under discussion (10,11). Conservative treatment may be effective in some fractures. OF1, 2 and 3 fractures are its main indications [according to the classification of the German Orthopedic Society (8)], in cases of mild pain and in which the ability to verticalize the trunk is preserved, allowing the patient to sit and even walk. This approach includes multimodal analgesia and the use of thoracic lumbar sacral orthosis whenever trunk verticalization occurs, for a period of 2 to 3 months until bone healing is achieved. In situations of severe and persistent pain and inability to verticalize the trunk, surgical treatment is indicated (11-16). Minimally invasive techniques for vertebral body augmentation have become increasingly popular in the treatment of osteoporotic vertebral fractures thanks to their capacity to stabilize the anterior Denis column through posterior percutaneous approach, making it possible to achieve positive results regarding the convalescence pace, symptom relief, the restoration of the spine’s biomechanics and anatomy and the quality and function of life indices (17-20).
Kyphoplasty rose from vertebroplasty, associating its stabilizing and analgesic effects because of the application of intravertebral cement, with the fractured vertebral body’s height restoration, through the previous creation of intrasomatic cavities resorting to expansive balloons. Next, these bilateral balloon’s spaces are filled with bone cement and this way, the fractured vertebral body is reduced and stabilized. Furthermore, these previously created lower pressure intrasomatic cavities covered by the vertebral body’s walls and by body impacted bone trabeculae, minimize cement leakage risk, making it possible to diminish the possibility of complications due to this extravasation such as radicular pain, paraplegia or even death (14,17,21-23). Nevertheless, kyphoplasty is criticized based on the incapacity to keep the restored vertebral body height after removing the balloons and before cement application, which leads to vertebra flattening due to elastic recoil by annulotaxis and ligamentotaxis. Moreover, even if the patient is placed on the table with the spine in hyperextension, compression forces of about 110 Newtons keep impacting the fractured vertebra, therefore influencing its flattening (17,18-22,24-30).
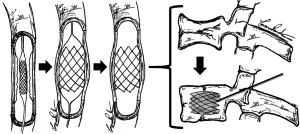
Intravertebral expansive implants present a controlled self-expansion capacity, being applied percutaneously through a posterior transpedicular access. These devices are placed into the fractured vertebral body, often with a compression fracture, with their expansion allowing for the reduction of the fracture of the vertebral body, thus restoring its integrity, height and stability. Armed kyphoplasty refers to the application of intravertebral expansive implants, also permitting prompt analgesia and stabilization advantages of kyphoplasty and vertebroplasty. Moreover, it allows for the preservation of the restored vertebral height over the medium to long term, which has been demonstrated in several studies (11,12,13,17-19,25-27,31-33). Expanded devices mechanically support vertebral platforms, functioning as an interior sustentaculum or a supporting endoskeleton, preventing flattening of the vertebrae, reducing the hazard of post-traumatic local and segmental kyphosis, and also assuring consistent anterior support at the vertebral body’s level (15,17,18,34-36). Therefore, intravertebral expansive implants have become popular regarding the treatment of vertebral body compression fractures, as they ensure a consistent anterior support at the vertebral body’s level provided by a posterior percutaneous transpedicular approach (15,16,34). The first intravertebral expansive implant developed was the VBS® (Vertebral Body Stenting) implant, which emerged as an adaptation of vascular stents to spinal surgery, now being applied and expanded inside the vertebral body (Figure 1) (7,11,12-14,16-19,25,27,31,32,36,37).
The present study aims to investigate the clinical (analgesia, functional disability and degree of evolution perceived by the patient) and imaging (reestablishment and maintenance of vertebral body heights) results achieved by armed kyphoplasty with the VBS® system, when applied to compressive burst thoracolumbar fractures of osteoporotic nature. Furthermore, it intends to analyze the evolution of the aforementioned variables and recognize possible correlations between them, identifying the most influential factors in relation to the final outcomes. We present the following article in accordance with the STROBE reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-22-59/rc).
Methods
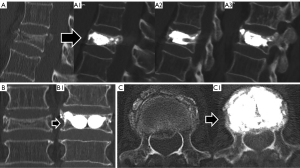
The present scientific investigation consists of a retrospective observational study in which we studied all patients with osteoporotic thoracolumbar compression burst vertebral fractures with involvement of one or both platforms and of more than one fifth of the posterior wall [included in types OF3 and OF4 of the classification of the German Society of Orthopedics (8)], who underwent armed kyphoplasty with VBS® stents (or stentoplasty) filled with polymethylmethacrylate bone cement over 10 years (between 2012 and 2022) in the same center since the introduction of this technique. The surgical technique is illustrated and described in Figure 2 and the characteristics of the implants are detailed in Table 1. Therapeutic indications for this type of osteoporotic fractures were as follows: when patients with osteoporotic thoracolumbar compression burst vertebral fractures were able to perform trunk verticalization, conservative treatment was initially chosen, with the use of thoracic lumbar sacral orthosis and symptomatic treatment. When patients with this type of fracture are immediately unable to perform trunk verticalization or when the symptoms do not improve and there is progression of vertebral flattening after a period of 3 to 4 weeks of conservative treatment, we opt for the surgical intervention of armed kyphoplasty with intrasomatic stents filled with polymethylmethacrylate bone cement.
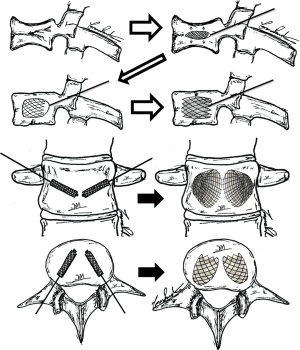
Table 1
| Implant name | VBS® | ||||||
|---|---|---|---|---|---|---|---|
| Morphology | Cylindrical shape network (stent). Two implants by bipedicular access | ||||||
| Material | Chromium-cobalt | ||||||
| Expansion direction | Circumferential and centrifugal in the coronal plane (craniocaudal + lateral) | ||||||
| Expansion mechanism | Hydraulic, by a kyphoplasty balloon (pressure and volume controlled) | ||||||
| Expansion force | Maximum pressure: 30 Atm; maximum expansion volumes: large stent: 5 mL; medium stent: 4.5mL; small stent: 4 mL | ||||||
| Goal | Fracture reduction and space filling | ||||||
| Rationale | VBS® refers to a space-filling and reduction implant system, as it has the potential to expand multidirectionally (laterally and vertically), being generally indicated in case of vertebral body’s replacement or reconstruction, with no need to await the healing of the vertebral fracture. Stents are implants that present two cavities which are coated by a casing of impacted trabeculae inside the vertebral body, with the expansion and impact of the encircling bony trabeculae. They give rise to cavities that replace a great part of the vertebral body interior, after being filled with bone graft or cement, padding and thus stabilizing it. Furthermore, these implants reduce cement extravasation by recreating the vertebral body’s walls through impaction of bony trabeculae with cement | ||||||
| Fragile bone (porotic or lithic) | → | Osteoporotic or neoplastic pathologic compression fractures | → | Need to reconstruct or replace the vertebral body = Fracture reduction + vertebral body filing | → | Implant to fill space by multidirectional expansion and creator of intrasomatic cavities to be filled with bone cement (VBS) | |
| ↓ | |||||||
| Aiming to replace the fragile vertebral body rather than waiting for fracture healing | |||||||
VBS, Vertebral Body Stenting; Atm, standard atmosphere.
Initially, through a percutaneous approach and fluoroscopy support, the bilateral transpedicular intraosseous path is carried out to the desired location within the vertebral body, by the sequential use of Jamshidi needle, guide wire, access cannula, drill and impactor, obtaining intraosseous tunnels from the posterior entry point to the vertebral body. Through these channels, kyphoplasty balloons surrounded by stents are applied bilaterally and inflated in a controlled manner. The balloons are removed after they are deflated and the expanded stents remain in place. Finally, bone cement is applied bilaterally inside the stents. There is also the option of previously inflating the kyphoplasty balloons without the stents, thus being able to predict the position and expansion of the latter, and then, with the pre-made intrasomatic cavities, expand the balloons with the stents again. Note the reduction of depressions in the upper and lower platforms after expansion of the implants and the final image with a gray stain representing the bone cement inside the stents. Also note in the sagittal, coronal and axial planes, the usual position occupied by non-expanded stents and after their expansion and filling with bone cement.
Patients who underwent armed kyphoplasty using the VBS® system with thoracolumbar osteoporotic compression burst vertebral fractures with a minimum follow-up time of 1 year were then identified. After the selection process (flowchart in Figure 3), we identified 41 operated patients, of whom 7 had already died. However, 4 more patients were excluded because they were uncontactable, resulting in a final sample of 30 patients, corresponding to 33 vertebrae that underwent surgery, as two patients had fractures at various levels.
Clinical and functional assessment was performed retrospectively based on clinical records regarding preoperative, immediate postoperative and current events. All patients were currently clinically evaluated using the visual analogue pain scale (VAS), the Oswestry Disability Index (ODI) and the Patient Global Impression of Change (PGIC) scale (38-40). The imaging assessment consisted of measuring the vertebral body heights both in the sagittal plane (anterior, intermediate and posterior heights) and in the coronal plane (right, central and left heights), as well as of carrying out the calculation of the Beck index (anterior height/posterior height), based on computed tomography obtained preoperatively, in the immediate postoperative period and at the end of the follow-up period.
Statistical analysis
All the patients were under bisphosphonates and calcium supplement since its osteoporotic fracture. Statistical analysis was performed using the IBM SPSS Statistics for Windows, Version 28.0 (IBM Corp., Armonk, NY, USA) software. The Shapiro-Wilk normality test identified asymmetric variable distributions, and nonparametric statistical tests were applied. P values <0.05 were considered statistically significant.
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The research project was approved by the Ethics Committee for Health of Coimbra University Hospital Center (No. OBS.SF.042-2022). All patients included in the study signed an informed consent.
Results
The mean age of patients was 73.3±7.3 years (range, 56–88 years). The sample included 24 female subjects, aged between 56 and 88 years, with a mean of 73.6±7.6 years, and 6 male subjects, aged between 65 and 80 years, with a mean of 72.0±6.6 years. The mean follow-up time was 4.5 years, with a minimum follow-up of 1 year and a maximum of 10 years. The mechanisms of osteoporotic vertebral fractures were: fall from standing height (23.3%), fall from a higher height (73.3%) and road accident (3.3%). The ability to verticalize the trunk was evaluated after the fracture, in the context of the emergency department, and it was preserved in 19 individuals (63.3%) and compromised in the remaining 11 (36.7%). After diagnosis, conservative therapy was the first approach in 12 patients (40.0%), while the remaining 18 (60.0%) were immediately proposed for surgical treatment of armed kyphoplasty with the VBS® system.
In terms of clinical and functional results, before the surgical treatment (after the fracture), there was an average VAS value of 9.6±0.8, ranging between 7 and 10. After surgery, the average perception of pain was of 2.2±1.6, varying only between 0 and 5, which corresponds to an average reduction of 6.7 (range, 3–9). In addition, the application of the ODI allowed the assessment of functional disability, which assumed an average of 89.3% (range, 48.9–100%) prior to surgery and decreased to 19.7% (range, 0–35.6%) after the intervention (Figure 4). In both variables, the difference verified between the preoperative period and in the current evaluation was statistically significant (P<0.01). Regarding the PGIC, it ranged between 6 and 7, with an average of 6.6 and a standard deviation of 0.5. Direct correlations were identified between PGIC and the remaining clinical variables—pain reduction (Rho =0.373) and functional disability reduction (Rho =0.425). Clinical results were also analyzed according to whether or not initial conservative therapy was performed and a statistically significant difference was identified (P=0.03) between the two groups. The group that underwent exclusive surgical therapy showed a greater decrease in the degree of disability (33.14±5.53) compared to the initial conservative therapy group (28.17±8.67).
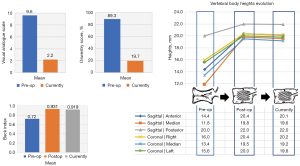
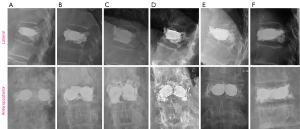
Regarding the imaging data, these are presented in Figure 4 and Table 2. Several cases present in this series are also illustrated, both in anteroposterior and lateral radiographs and computed tomography in several planes in Figures 5-7. There was a statistically significant increase in all measurements performed both in the coronal and in the sagittal planes between preoperative and immediate postoperative period and at the end of follow-up time (P<0.01) (Figure 4 and Table 2). In relation to the heights of the immediate postoperative period, compared to the end of the follow-up, these decreased residually (maximum difference was of 2.6), however these differences were mostly statistically significant, although with less impact, as can be seen in Table 2 by the larger p-values. Nonetheless, there is an exception, which is the posterior height, whose difference between the immediate postoperative period and the end of the follow-up is not statistically significant (P=0.325).
Table 2
| Compared time periods | Plane | Height location | Difference (mm) | P value |
|---|---|---|---|---|
| Preoperative → immediate postoperative | Sagittal | Anterior | 11.5 | <0.01 |
| Median | 15.9 | <0.01 | ||
| Posterior | 5.0 | <0.01 | ||
| Coronal | Right | 10.5 | <0.01 | |
| Median | 11.4 | <0.01 | ||
| Left | 9.5 | <0.01 | ||
| Postoperative → currently | Sagittal | Anterior | 2.3 | 0.026 |
| Median | 2.5 | 0.016 | ||
| Posterior | 1.0 | 0.325 | ||
| Coronal | Right | 2.6 | 0.015 | |
| Median | 2.4 | 0.021 | ||
| Left | 2.4 | 0.023 | ||
| Preoperative → currently | Sagittal | Anterior | 10.7 | <0.01 |
| Median | 15.2 | <0.01 | ||
| Posterior | 5.0 | <0.01 | ||
| Coronal | Right | 6.7 | <0.01 | |
| Median | 11.6 | <0.01 | ||
| Left | 9.7 | <0.01 |
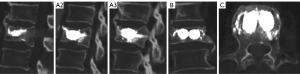
Concomitantly, the existence of a correlation between each of the measured vertebral heights and the clinical parameters was evaluated, and direct correlations were identified between the decrease in disability (ODI) and the heights in the coronal plane at the end of the follow-up period (right height with Rho =0.368 and P=0.035, median height with Rho =0.460 and P=0.007, left height with Rho =0.516 and P=0.002). Finally, the Beck Index was introduced in this analysis, showing a mean of 0.72 (range, 0.45–0.93) in the preoperative period, which rose to 0.93 (range, 0.69–1.25) in the immediate postoperative period, representing an average increase of 0.21 (range, 0.06–0.57). At the end of the follow-up period, there was a mean Beck index of 0.92 (range, 0.62–1.25) (Figure 4). A statistically significant difference ((P<0.01) was identified between the Beck Index figure before surgery and at the end of follow-up, demonstrating a decrease of 7.4. It is also worth mentioning the identification of a direct correlation (Rho =0.465), between the final Beck Index (assessed at the end of the follow-up period) and the decrease in functional disability (ODI), with statistical significance (P=0.006). Based on computed tomography, 7 cases of cement leakage (21.21% of the operated vertebrae) were identified, without any clinical translation. Regarding its location, we verified 6 cases of anterior leakage, one of inferior leakage and one of upper leakage. In this series, there was also one case of fracture at a level adjacent to the vertebra initially affected, which represents 3.03% of the operated vertebrae.
Discussion
The treatment of osteoporotic fractures of the thoracolumbar spine has been the subject of intense debate, ranging from conservative to posterior stabilization, with or without corporectomy, and cementoplasty techniques. As patients with this condition are usually elderly, we highlight the practically immediate capacity of cementoplasty techniques (vertebroplasty and kyphoplasty) to provide pain relief and consequent standing up and walking after a few hours’ time, no pain, and no restriction of activity usually within 24 hours (17-20). The advantage of armed kyphoplasty with expansive intravertebral implants over classic vertebroplasty and kyphoplasty is mainly the superior preservation of restored vertebral height, as it is mechanically supported by the expanded devices (they work as a supporting endoskeleton or interior sustentaculum), which has been shown in diverse studies regarding medium and long-term follow-up (11,12,13,17-19,25-28,31-36). The authors of the present study defend, in the case of acute burst osteoporotic vertebral fractures [OF3 and OF4 of the classification of the German Orthopedic Society (8)], in which the patient is unable to verticalize the trunk or with an unfavorable evolution after an attempt of a conservative treatment, the surgical intervention of armed kyphoplasty, that is, fracture reduction and stabilization with expansive intravertebral implants which are filled with bone cement. Particularly in compression fractures of vertebral bodies, we defend the importance of anatomical restoration or the most similar to this (at the angle of vertebral kyphosis, vertebral height and vertebral endplates morphology), as in other joints of the human body, so as to ensure a spine which is functionally and biomechanically closer to the one existent before the fracture. While in young individuals, an anatomical reduction of the vertebral body is sought to prevent progression to osteodegenerative and disc changes in that vertebral segment as well as adjoining levels, in the elderly, often with osteoporosis, the objective of anatomical reduction is mainly to prevent anterior overload of adjacent bodies, this way reducing the peril of adjacent vertebral fractures (11,12,17,18,25,41,42). It is now recognized that in osteoporotic vertebral fractures, restoring the height of the vertebral body at the time of the first fracture is pivotal to avoid the disease’s domino effect, that is, the consecutive occurrence of osteoporotic fractures in adjacent vertebrae due to overload of the anterior column after the first uncorrected vertebral wedge fracture. The wedge of the vertebrae progressively shifts the load axis to a more anterior position, exposing the fragile osteoporotic vertebral bodies to excessive anterior loads, favoring a cascade of consecutive pathological fractures and the kyphotization of the spine (11,20,25,43).
Expansive intravertebral implants are associated to the concept of direct fracture reduction, which is performed through an expanded implant at the accurate fracture location, inside the vertebral body (11,25). If the fracture takes place through a compression mechanism, those implants will act the other way round: they cause the vertebral body to expand, contrarily to the mechanism which led to the fracture. This way, it can be considered a very efficient method of fracture reduction. The problem of vertebral compression fractures is located at the vertebral body, which is fractured, thus, it is important to address some action targeting its reduction and direct stabilization (42-45). Several studies have shown that the idea that the expansive intravertebral implant may increase the posterior wall retropulsion in compression burst fractures is not verified with the correct positioning of the implants. On the contrary, due to the effect of ligamentotaxis and annulotaxis when the implants are expanded, the increase in body height makes the posterior wall move to anterior, deviating from the vertebral canal and moving closer to its original position, recovering posterior vertebral height and provoking an indirect decompression of the vertebral canal (12,13,17,46-54). The rarefaction, fragility and marked destruction of the intrasomatic bone trabeculae of osteoporotic burst fractures [osteoporotic fractures types OF3 and OF4 (8)] makes it necessary to replace most of the interior of the empty vertebral body with other material, in order to provide it with rigidity and stability, restoring its structural support function to the spine. In view of this, in the authors’ opinion, in burst osteoporotic fractures, the intravertebral expansive implants of choice to perform armed kyphoplasty are intrasomatic stents (also known as stentoplasty) (Figure 3). The rationale is that intrasomatic stents (VBS®), in addition to being reducing implants, are also space occupiers, since they are cylindrical implants of considerable size with multidirectional expansion (vertical and lateral). On account of their expansion and impaction of encircling bone trabeculae, they configure two cavities inside the vertebral body, coated by a casing of impacted trabeculae, which, after being filled with bone cement, substitute a major part of the vertebral body’s interior, also filling and steadying it promptly. Therefore, it makes sense that intrasomatic stents are applied for interior replacement or reconstruction of the weakened vertebral body. In these fractures, typically in the elderly, immediate stabilization of the fracture is regarded as a solution to achieve quick relief of symptoms and functional restoration. It is not essential for older patients to obtain a vertebra that is biomechanically similar to the others and is not the objective to wait for the fracture to heal, but only to ensure its immediate stabilization with the vertebral height restored as much as possible. The metallic mesh of cement-filled stents (bone-stent-cement complex) simulates the concept of reinforced concrete in civil construction, that is, the vertebral body is internally replaced by a metallic endoskeleton filled with bone cement, which guarantees its stable and resistant reconstruction. In short, intravertebral expansive stents filled with bone cement reduce and internally replace the flattened, fragile and destroyed vertebral body, with no intention of waiting for bone healing. In theory, another advantage pointed out to stentoplasty compared to traditional kyphoplasty is that these implants reduce cement leakage by rebuilding the vertebral body’s walls through the impaction of bone trabeculae during their expansion, containing the cement inside (11,25,36,55). In addition, expansion of the balloons surrounded by the stents occurs more uniformly and predictably compared to traditional kyphoplasty, which may have advantages in fracture reduction capability and in reducing the risk of cement leakage. Since it is not rigid, the balloon expansion will most probably insinuate itself through regions characterized by lower pressure, and generating abnormal cavities, reducing the effectiveness and predictability of direct reduction of the vertebral body and increasing the risk of cement leakage (11,25,36,55).
In our study, a statistically significant improvement in all clinical and functional parameters was observed after the intervention. After surgery, the maximum degree of disability (ODI) reported was 35.6% (moderate disability), representing an average decrease of 69.6% compared to the disability reported prior to surgery, when it assumed average figures of 89.3% (disability). These results are in agreement with several studies that report that kyphoplasty with stents as a surgical treatment for osteoporotic vertebral fractures has positive results in terms of analgesia and improvement in functional disability (7,11,12-14,16-19,25,27,31,32,36,37). The assessment of the PGIC is one of the innovative topics addressed in this study and that allows to understand patients’ perception of the impact of the surgical intervention on their quality of life in relation to the preoperative period. As expected, it was observed that more accentuated decreases in pain and in the degree of functional disability translate into greater PGIC. We found that in 63.2% of patients with burst osteoporotic fractures and preserved trunk verticalization capacity, in whom conservative treatment with multimodal analgesia and thoracolumbar orthosis was initiated, this type of treatment was ineffective and they underwent armed kyphoplasty, which represents a considerable number. In addition, it was found that patients who underwent surgical therapy at the outset experienced greater reductions in functional disability, compared to those who had a previous attempt at conservative treatment and were only operated on after its failure. These data lead us to reflect on the repercussions of delaying the surgery in these fractures, since in these cases it was harmful to the patients and caused worse clinical results. Therefore, we consider that a better definition of surgical criteria for burst osteoporotic fractures may be necessary, namely by reducing the threshold for surgical indication, even in patients capable of verticalizing the trunk, seeking to avoid the suffering of conservative treatment over several weeks and, above all, the risk of its failure. The results of the present study demonstrate that stent-armed kyphoplasty allows for an adequate reduction of these fractures, with restoration of vertebral body heights, which are maintained in the medium-long term, as also indicated in previous studies (7,11,12-14,16-19,25,27,31,32,36,37). There was a statistically significant difference regarding the height of the vertebral body in its different regions, between the pre- and post-operative moments, which indicates the biomechanical efficacy and fracture reduction potential of this technique. In addition, a statistically significant increase in vertebra heights observed between preoperative and end-of-follow-up moments was confirmed [increase of 10.7-15.2-5.0 mm (anterior-median-posterior) in the sagittal plane and 6.7-11.6-9.7 mm (right-median-left) in the coronal plane], which indicates its ability to maintain fracture reduction. Another parameter used to analyze the imaging data was the Beck index, which reflects the relationship between the anterior and posterior height of the vertebral body. Thus, fractures with uniform flattening of the vertebra, that is, with similar anterior and posterior heights, originate Beck indices close to one. On the other hand, vertebrae whose fracture causes a more pronounced flattening of one of the anterior or posterior ends lead to Beck indices other than one. In the present study, the significance of the differences between the Beck indices recorded in the following pairs was investigated: pre and postoperative, preoperative and follow-up, postoperative and follow-up. Statistically significant differences were observed between all times; however, we would like to point out that the absolute mean decrease in the Beck index between the immediate postoperative period and at the end of the follow-up period is only 0.01 mm, which, despite having statistical significance, is hardly of clinical interest, reflecting only very residual anterior flattening. In this study, a statistically significant correlation was established between the right, median and left heights of the vertebral body evaluated at the end of the follow-up period and the decrease in functional disability (ODI). Thus, the study suggests that vertebrae with more heights restored in the coronal plane ensure greater improvements in patients’ functional disability. Concomitantly, a direct and statistically significant correlation was identified between the final Beck index (recorded at the end of the follow-up period) and the degree of disability improvement (ODI). Thus, it is demonstrated that the most effective restoration of the anterior height of the vertebral body and its consequent approximation to the posterior height, as well as the greater restoration of heights in the coronal plane, by recreating the original morphology of the vertebral body more faithfully, are associated with more satisfactory functional results, which makes our study one of the first to establish a correlation between functional and imaging clinical data (anatomical restoration in both sagittal and coronal planes) regarding the surgical treatment of osteoporotic fractures.
In this investigation, there was only one adjacent fracture case, resulting in a fracture rate of 3.3%, which represents a figure slightly lower than that reported in similar studies (7,12,13,17,18,27,31,32,36,37). The small rate of adjacent vertebral fractures in the present study may be the result of the adequate anatomical restoration obtained from the vertebral bodies and, above all, their maintenance over the follow-up period. Although it remains a controversial topic, perceiving, whether these fractures are a complication of surgery or if they represent the natural progression of osteoporotic spinal disease, in the authors’ opinion, maintained anatomical reduction of the vertebral body avoids overloading the spine after a first uncorrected vertebral wedge fracture, preventing the domino effect of subsequent fractures in adjacent vertebrae and the onset of the kyphotizing osteoporotic cascade (11,25,32). In the present study, the cement leakage rate was 21.2%, compared to the total number of operated vertebrae, which is in agreement with the literature (7,11,12-14,16-19,25,27,31,32,36,37). The extravasation was accurately detected on computed tomography and not on radiographs; however, this is only an imaging finding, as none of the cases had any clinical translation. We consider that despite this extravasation rate, it is more controlled compared to traditional vertebroplasty or kyphoplasty, as in the present technique, uniform low pressure intrasomatic cavities are surrounded by the cylindrical metal meshes of the implants and by impacted bone trabeculae, such as previously mentioned. In this way, only slight leakages were identified on the anterior surface of the implants (where the cylinder is open) and never laterally or posteriorly, which are places of greater clinical risk for this leakage. Although cylinder implants are also open on the posterior surface, the absence of posterior leakage can be explained by the fact that we usually apply the cement with the cannulas located in the middle portion of the interior of the stents and always stop the cement injection when it reaches the posterior end of the implants. No cases of implant migration were identified, which, in our opinion, is due to the effective stabilization of the expanded stent integrated into the stent-impacted bone-cement complex.
The main limitations of this study are related to its retrospective nature and the reduced control for confounding factors that affect clinical outcomes and osteoporosis progression, small number of patients with this specific type of osteoporotic burst fractures, lack of control group and some heterogeneity in the follow-up periods, despite representing a 10-year-experience of a hospital center.
Conclusions
The posterior percutaneous transpedicular access and the ability to anatomically restore the fractured vertebra, as well as the recovery of vertebral height and the ability to maintain it in the medium-long term, make stent-armed kyphoplasty a significantly promising alternative regarding the treatment of osteoporotic compressive thoracolumbar fractures. In this study, it was found that that this technique enables an effective and uniform restoration of the anatomical structure of the vertebral body, as well as an approximation to its original morphology, which positively influences the clinical and functional results. Furthermore, this study demonstrates, in a pioneering way, regarding osteoporotic fractures, the existence of a clinical-morphological correlation regarding their surgical treatment, that is, it was possible to demonstrate that a more effective morphological restoration of vertebral heights in both sagittal and coronal planes is associated with more satisfactory functional clinical parameters. We conclude that stent-armed kyphoplasty is a safe and effective technique in the treatment of compressive burst osteoporotic fractures, with a reduced risk of adverse events, rapid recovery and encouraging results with regard to anatomical restoration, accompanied by significant reduction in pain and the degree of patients’ disability, which represents an improvement in their quality of life.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-22-59/rc
Data Sharing Statement: Available at https://jss.amegroups.com/article/view/10.21037/jss-22-59/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-22-59/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The research project was approved by the Ethics Committee for Health of Coimbra University Hospital Center (No. OBS.SF.042-2022). All patients included in the study signed an informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sözen T, Özışık L, Başaran NÇ. An overview and management of osteoporosis. Eur J Rheumatol 2017;4:46-56. [Crossref] [PubMed]
- Chandra A, Rajawat J. Skeletal Aging and Osteoporosis: Mechanisms and Therapeutics. Int J Mol Sci 2021;22:3553. [Crossref] [PubMed]
- Sanfélix-Genovés J, Hurtado I, Sanfélix-Gimeno G, et al. Impact of osteoporosis and vertebral fractures on quality-of-life. a population-based study in Valencia, Spain (The FRAVO Study). Health Qual Life Outcomes 2011;9:20. [Crossref] [PubMed]
- Johnston CB, Dagar M. Osteoporosis in Older Adults. Med Clin North Am 2020;104:873-84. [Crossref] [PubMed]
- Sahota O, Ong T, Salem K. Vertebral Fragility Fractures (VFF)-Who, when and how to operate. Injury 2018;49:1430-5. [Crossref] [PubMed]
- Kendler DL, Bauer DC, Davison KS, et al. Vertebral Fractures: Clinical Importance and Management. Am J Med 2016;129:221.e1-10. [Crossref] [PubMed]
- Heini PF, Teuscher R. Vertebral body stenting / stentoplasty. Swiss Med Wkly 2012;142:w13658. [PubMed]
- Schnake KJ, Blattert TR, Hahn P, et al. Classification of Osteoporotic Thoracolumbar Spine Fractures: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Global Spine J 2018;8:46S-9S. [Crossref] [PubMed]
- Prost S, Pesenti S, Fuentes S, et al. Treatment of osteoporotic vertebral fractures. Orthop Traumatol Surg Res 2021;107:102779. [Crossref] [PubMed]
- Halvachizadeh S, Stalder AL, Bellut D, et al. Systematic Review and Meta-Analysis of 3 Treatment Arms for Vertebral Compression Fractures: A Comparison of Improvement in Pain, Adjacent-Level Fractures, and Quality of Life Between Vertebroplasty, Kyphoplasty, and Nonoperative Management. JBJS Rev 2021; [Crossref] [PubMed]
- Moura DL, Gabriel JP. Expandable Intravertebral Implants: A Narrative Review on the Concept, Biomechanics, and Outcomes in Traumatology. Cureus 2021;13:e17795. [Crossref] [PubMed]
- Diel P, Röder C, Perler G, et al. Radiographic and safety details of vertebral body stenting: results from a multicenter chart review. BMC Musculoskelet Disord 2013;14:233. [Crossref] [PubMed]
- Thaler M, Lechner R, Nogler M, et al. Surgical procedure and initial radiographic results of a new augmentation technique for vertebral compression fractures. Eur Spine J 2013;22:1608-16. [Crossref] [PubMed]
- Vanni D, Galzio R, Kazakova A, et al. Third-generation percutaneous vertebral augmentation systems. J Spine Surg 2016;2:13-20. [Crossref] [PubMed]
- Maestretti G, Cremer C, Otten P, et al. Prospective study of standalone balloon kyphoplasty with calcium phosphate cement augmentation in traumatic fractures. Eur Spine J 2007;16:601-10. [Crossref] [PubMed]
- Muto M, Marcia S, Guarnieri G, et al. Assisted techniques for vertebral cementoplasty: why should we do it? Eur J Radiol 2015;84:783-8. [Crossref] [PubMed]
- Klezl Z, Majeed H, Bommireddy R, et al. Early results after vertebral body stenting for fractures of the anterior column of the thoracolumbar spine. Injury 2011;42:1038-42. [Crossref] [PubMed]
- Rotter R, Martin H, Fuerderer S, et al. Vertebral body stenting: a new method for vertebral augmentation versus kyphoplasty. Eur Spine J 2010;19:916-23. [Crossref] [PubMed]
- Vanni D, Pantalone A, Bigossi F, et al. New perspective for third generation percutaneous vertebral augmentation procedures: Preliminary results at 12 months. J Craniovertebr Junction Spine 2012;3:47-51. [Crossref] [PubMed]
- Wardlaw D, Cummings SR, Van Meirhaeghe J, et al. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet 2009;373:1016-24. [Crossref] [PubMed]
- Cornelis FH, Joly Q, Nouri-Neuville M, et al. Innovative Spine Implants for Improved Augmentation and Stability in Neoplastic Vertebral Compression Fracture. Medicina (Kaunas) 2019;55:426. [Crossref] [PubMed]
- McGirt MJ, Parker SL, Wolinsky JP, et al. Vertebroplasty and kyphoplasty for the treatment of vertebral compression fractures: an evidenced-based review of the literature. Spine J 2009;9:501-8. [Crossref] [PubMed]
- Papanastassiou ID, Phillips FM, Van Meirhaeghe J, et al. Comparing effects of kyphoplasty, vertebroplasty, and non-surgical management in a systematic review of randomized and non-randomized controlled studies. Eur Spine J 2012;21:1826-43. [Crossref] [PubMed]
- Feltes C, Fountas KN, Machinis T, et al. Immediate and early postoperative pain relief after kyphoplasty without significant restoration of vertebral body height in acute osteoporotic vertebral fractures. Neurosurg Focus 2005;18:e5. [Crossref] [PubMed]
- Moura DFL, Gabriel JP. Intravertebral expandable implants in thoracolumbar vertebral compression fractures. Acta Ortop Bras 2022;30:e245117. [Crossref] [PubMed]
- Verlaan JJ, van de Kraats EB, Oner FC, et al. The reduction of endplate fractures during balloon vertebroplasty: a detailed radiological analysis of the treatment of burst fractures using pedicle screws, balloon vertebroplasty, and calcium phosphate cement. Spine (Phila Pa 1976) 2005;30:1840-5. [Crossref] [PubMed]
- Muto M, Greco B, Setola F, et al. Vertebral Body Stenting System for the Treatment of Osteoporotic Vertebral Compression Fracture: Follow-up at 12 Months in 20 Cases. Neuroradiol J 2011;24:610-9. [Crossref] [PubMed]
- Rotter R, Schmitt L, Gierer P, et al. Minimum cement volume required in vertebral body augmentation--A biomechanical study comparing the permanent SpineJack device and balloon kyphoplasty in traumatic fracture. Clin Biomech (Bristol, Avon) 2015;30:720-5. [Crossref] [PubMed]
- Krüger A, Baroud G, Noriega D, et al. Height restoration and maintenance after treating unstable osteoporotic vertebral compression fractures by cement augmentation is dependent on the cement volume used. Clin Biomech (Bristol, Avon) 2013;28:725-30. [Crossref] [PubMed]
- Voggenreiter G. Balloon kyphoplasty is effective in deformity correction of osteoporotic vertebral compression fractures. Spine (Phila Pa 1976) 2005;30:2806-12. [Crossref] [PubMed]
- Hartmann F, Griese M, Dietz SO, et al. Two-year results of vertebral body stenting for the treatment of traumatic incomplete burst fractures. Minim Invasive Ther Allied Technol 2015;24:161-6. [Crossref] [PubMed]
- Werner CM, Osterhoff G, Schlickeiser J, et al. Vertebral body stenting versus kyphoplasty for the treatment of osteoporotic vertebral compression fractures: a randomized trial. J Bone Joint Surg Am 2013;95:577-84. [Crossref] [PubMed]
- Lin JH, Wang SH, Lin EY, et al. Better Height Restoration, Greater Kyphosis Correction, and Fewer Refractures of Cemented Vertebrae by Using an Intravertebral Reduction Device: a 1-Year Follow-up Study. World Neurosurg 2016;90:391-6. [Crossref] [PubMed]
- Maestretti G, Sutter P, Monnard E, et al. A prospective study of percutaneous balloon kyphoplasty with calcium phosphate cement in traumatic vertebral fractures: 10-year results. Eur Spine J 2014;23:1354-60. [Crossref] [PubMed]
- Fuentes S, Metellus P, Fondop J, et al. Percutaneous pedicle screw fixation and kyphoplasty for management of thoracolumbar burst fractures. Neurochirurgie 2007;53:272-6. [Crossref] [PubMed]
- Fürderer S, Anders M, Schwindling B, et al. Vertebral body stenting. A method for repositioning and augmenting vertebral compression fractures. Orthopade 2002;31:356-61. [PubMed]
- Schützenberger S, Schwarz SM, Greiner L, et al. Is vertebral body stenting in combination with CaP cement superior to kyphoplasty? Eur Spine J 2018;27:2602-8. [Crossref] [PubMed]
- Freyd M. The Graphic Rating Scale. Journal of Educational Psychology 1923;14:83-102.
- Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976) 2000;25:2940-52; discussion 2952. [Crossref] [PubMed]
- Dominges L, Cruz E. Adaptação Cultural e Contributo para a Validação da Escala Patient Global Impression of Change. Ifisionline 2011;2:31-7.
- Cinotti G, Della Rocca C, Romeo S, et al. Degenerative changes of porcine intervertebral disc induced by vertebral endplate injuries. Spine (Phila Pa 1976) 2005;30:174-80. [Crossref] [PubMed]
- Kerttula LI, Serlo WS, Tervonen OA, et al. Post-traumatic findings of the spine after earlier vertebral fracture in young patients: clinical and MRI study. Spine (Phila Pa 1976) 2000;25:1104-8. [Crossref] [PubMed]
- Grafe IA, Baier M, Nöldge G, et al. Calcium-phosphate and polymethylmethacrylate cement in long-term outcome after kyphoplasty of painful osteoporotic vertebral fractures. Spine (Phila Pa 1976) 2008;33:1284-90. [Crossref] [PubMed]
- Verlaan JJ, van Helden WH, Oner FC, et al. Balloon vertebroplasty with calcium phosphate cement augmentation for direct restoration of traumatic thoracolumbar vertebral fractures. Spine (Phila Pa 1976) 2002;27:543-8. [Crossref] [PubMed]
- Verlaan JJ, Somers I, Dhert WJ, et al. Clinical and radiological results 6 years after treatment of traumatic thoracolumbar burst fractures with pedicle screw instrumentation and balloon assisted endplate reduction. Spine J 2015;15:1172-8. [Crossref] [PubMed]
- Fredrickson BE, Edwards WT, Rauschning W, et al. Vertebral burst fractures: an experimental, morphologic, and radiographic study. Spine (Phila Pa 1976) 1992;17:1012-21. [Crossref] [PubMed]
- Harrington RM, Budorick T, Hoyt J, et al. Biomechanics of indirect reduction of bone retropulsed into the spinal canal in vertebral fracture. Spine (Phila Pa 1976) 1993;18:692-9. [Crossref] [PubMed]
- Krüger A, Schmuck M, Noriega DC, et al. Percutaneous Dorsal Instrumentation of Vertebral Burst Fractures: Value of Additional Percutaneous Intravertebral Reposition-Cadaver Study. Biomed Res Int 2015;2015:434873. [Crossref] [PubMed]
- Oner FC, van der Rijt RR, Ramos LM, et al. Changes in the disc space after fractures of the thoracolumbar spine. J Bone Joint Surg Br 1998;80:833-9. [Crossref] [PubMed]
- Noriega DC, Marcia S, Ardura F, et al. Diffusion-Weighted MRI Assessment of Adjacent Disc Degeneration After Thoracolumbar Vertebral Fractures. Cardiovasc Intervent Radiol 2016;39:1306-14. [Crossref] [PubMed]
- Olivier E, Beldame J, Ould-Slimane M, et al. Treatment of thoracolumbar junction burst fractures (Magerl A3) by balloon kyphoplasty: anatomic study. Rev Chir Orthop Reparatrice Appar Mot 2007;93:666-73. [Crossref] [PubMed]
- Verlaan JJ, Dhert WJ, Verbout AJ, et al. Balloon vertebroplasty in combination with pedicle screw instrumentation: a novel technique to treat thoracic and lumbar burst fractures. Spine (Phila Pa 1976) 2005;30:E73-9. [Crossref] [PubMed]
- Venier A, Roccatagliata L, Isalberti M, et al. Armed Kyphoplasty: An Indirect Central Canal Decompression Technique in Burst Fractures. AJNR Am J Neuroradiol 2019;40:1965-72. [Crossref] [PubMed]
- Krüger A, Oberkircher L, Figiel J, et al. Height restoration of osteoporotic vertebral compression fractures using different intravertebral reduction devices: a cadaveric study. Spine J 2015;15:1092-8. [Crossref] [PubMed]
- Cianfoni A, Distefano D, Pravatà E, et al. Vertebral body stent augmentation to reconstruct the anterior column in neoplastic extreme osteolysis. J Neurointerv Surg 2019;11:313-8. [Crossref] [PubMed]



