
Clinical outcomes after bracing for vertebral compression fractures: a systematic review and meta-analysis of randomized trials
Highlight box
Key findings
• Bracing may reduce pain up to six months after vertebral compression fracture.
What is known and what is new?
• There is no consensus regarding nonoperative management strategies for vertebral compression fractures.
• This study clarifies the efficacy of bracing for vertebral compression fractures.
What is the implication, and what should change now?
• Providers should consider bracing as first line management for patients with painful vertebral compression fractures. Larger randomized studies are needed to establish stronger recommendations.
Introduction
Osteoporosis is common in post-menopausal women, prevalent in 18.8% of women 50 years of age and older (approximately 11.7 million US women) in 2017–2018 (1). Its prevalence is projected to increase by more than 30% from 2010–2030 (2). Osteoporosis is characterized by decreased bone density and increased fracture risk (3-7). Fragility fractures frequently manifest, resulting from low energy forces.
Vertebral compression fractures are the most common type of osteoporotic fragility fracture, with an annual incidence of over 700,000 patients in the United States (8-10). This represents a major cause of morbidity and significant cost to the healthcare system (11-15). From 2017–2018 the mean all-cause healthcare cost associated with a single osteoporotic fracture was $34,855. Factors associated with decreasing costs are early fracture identification, early treatment of index fracture, and prevention of future fractures with osteoporosis management (16).
The management of acute vertebral compression fractures remains controversial. Differences in management strategies may arise from the fact that these injuries are managed by primary care physicians, emergency physicians, neurosurgeons, orthopedic surgeons, and radiologists. In general, management of these injuries is divided into operative and nonoperative treatment. The goal of treatment is pain control, early mobilization, and neurologic stability. Operative treatment includes vertebroplasty, kyphoplasty, or posterior spinal instrumentation. While these injuries are primarily managed nonoperatively, there is no consensus regarding the ideal nonoperative treatment protocol.
A current option for nonoperative treatment isbracing. This method of treatment is blurred by a wide variety of soft and rigid braces on the market. In the present study, we aim to elucidate the effect of nonoperative management with soft and rigid bracing for acute thoracic and lumbar compression fractures when compared to using no brace. We hypothesize that there will be no difference in clinical or radiographic outcomes in the management of an acute vertebral compression fractures, regardless of brace usage. We present this article in accordance with the PRISMA reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-22-78/rc).
Methods
Literature search strategy
A literature search of Embase, Ovid, and the Cochrane Library was performed on October 25, 2021 to identify relevant studies. The following MeSH terms and their combinations were used for title/abstract searches: spine, vertebral body, wedge or compression fracture, A1, thoracolumbosacral orthosis, or brace. A manual search of reference lists was also performed. A detailed description of search strategies is included in Appendix 1.
Inclusion and exclusion criteria
Titles and abstracts were screened to identify studies that met the following inclusion criteria: (I) prospective randomized controlled trials comparing the treatment of thoracolumbar compression fractures in neurologically intact adult patients with or without an orthosis; (II) a minimum duration of follow-up of 3 months; and (III) evaluation of clinical or radiographic outcomes following conservative treatment. The exclusion criteria included (I) retrospective comparative studies (case control, cohort), (II) studies comparing surgical versus nonsurgical treatments, and (III) studies on thoracolumbar burst fractures. Editorials, review articles, case reports, and animal studies were also excluded. Levels of evidence were assigned to the studies according to the criteria described in Clinical Orthopaedics and Related Research, which are adapted from the Oxford Centre for Evidence-based Medicine levels of evidence. Only Level 1 studies were included.
Search result screening
Two of the authors independently reviewed all titles and/or abstracts, with the senior author available to resolve disputes. All irrelevant titles were excluded, and full-text papers were obtained when titles were deemed relevant or when eligibility was unclear. Two of the authors independently assessed these full-text manuscripts.
Data extraction
Outcome data and study characteristics were extracted in duplicate by two of the authors. Missing data were collected by using WebPlotDigitzer software (version 4.5; released August 15, 2021) to extract numerical values from figures and graphs.
The following data were extracted from included studies: (I) study identifiers (authors, publication year, title); (II) study characteristics (design, region, sample sizes, sex, age, smoking status, level of injury); (III) clinical outcomes Short-Form-36 Physical component and Mental Component (SF-36 PCS, SF-36 MCS), pain, satisfaction, Oswestry Disability Index (ODI), Limitations of Daily Living (LDL), Japanese Orthopaedic Association Back Pain Evaluation Questionnaire (JOABPEQ), well-being, EuroQol-5 Dimension-3 Level (EQ-5D-3L), opioid use; and (IV) radiographic outcomes (body compression ratio, regional kyphosis angle). Orthosis patient groups (soft or rigid) were determined by existing groups within the included studies, and by author discretion. We considered rigid braces those that inhibit spinal motion, and soft braces those that provide support but allow motion.
Quality assessment
A systematic assessment of bias in the randomized controlled trials was performed independently by two of the authors with the use of the Cochrane criteria (17). The items used for the assessment of each study were divided into the following sources of bias: selection (randomized), blinding, detection, attrition and management of drop-out, selective outcome reporting, and other potential sources of bias.
Statistical analysis
All meta-analyses were performed with the use of Review Manager 5.4.1 [RevMan (Computer program). Version 5.4.1, The Cochrane Collaboration, 2020]. Mean differences and standardized mean differences with 95% confidence intervals (CIs) in a random effects model were used to compare continuous variables. Odds ratios with 95% CIs in a random-effects model was used to compare dichotomous variables. A probability of P<0.05 was considered significant. An I2 test was used to calculate statistical heterogeneity, with a value of >50% representing substantial heterogeneity.
Assessment of evidence
GRADE (Grades of Recommendation Assessment, Development and Evaluation) criteria were applied to evaluate the quality of evidence relating to pain outcomes with or without rigid bracing. All three randomized trials were considered high quality studies for the assessment. The quality of the evidence was subject to downgrading based on risk of bias, inconsistency, indirectness, imprecision, and other considerations. A multi-domain risk of bias assessment was also performed using the Cochrane Risk of Bias tool.
Results
Search results
A search strategy flow diagram is summarized in Figure 1. A total of 1,497 articles were identified with the use of the previously outlined search strategy. An additional 5 articles were identified through snowballing. After duplicates were removed, 1,415 articles remained. Titles and abstracts were reviewed, and 1,401 articles were excluded. Of the remaining 14 articles, 11 were excluded during comprehensive full-text evaluation. These studies were excluded for various reasons including follow-up less than 3 months, nonrandomized or retrospective designs, and inclusion of burst fractures. A list of the 11 excluded studies is provided in Appendix 2. The remaining 3 studies met the inclusion criteria and were included in the meta-analysis (Figure 1). These had a total of 447 patients (96% female). Fifty-four patients were managed without a brace, and 393 with a brace (195 rigid, 198 soft).
Study characteristics and quality assessment
Of the three included studies, there were two randomized controlled trials and one randomized cross-over study (18-20) (Table 1). All three studies limited inclusion to acute or subacute single-level osteoporotic compression fractures. Two of the studies were limited to female patients. Minimum participant age ranged from 50 years and older to 65 years and older. All studies demonstrated random sequence generation, allocation concealment, blinding of outcome assessment and data analysis, low attrition, and low risk of reporting bias. There was generally a high risk of bias due to participant knowledge of orthosis group.
Table 1
| Study | Design | Level of evidence | Region | No. of centers | Age, years (mean) | Sample size (No. of patients) | |||
|---|---|---|---|---|---|---|---|---|---|
| Total | No orthosis | Rigid | Soft | ||||||
| Kato et al. 2019 (19) | RCT | I | Japan | 71 | 75.5 | 284 | – | 141 | 143 |
| Kim et al. 2014 (18) | RCT | I | South Korea | 1 | 70.2 | 55 | 18 | 18 | 19 |
| Pfeifer et al. 2011 (20) | RCT | I | Germany | 1 | 71.6 | 108 | 36 | 36 | 36 |
RCT, randomized controlled trial.
Patients in the study by Kim et al. were randomized into three groups: rigid brace, soft brace, or no brace. These patients’ outcomes were analyzed for 12 weeks. Pfeifer et al. also randomized patients into one of three groups: Spinomed, Spinomed Active, or no brace. We considered the Spinomed brace as rigid, and the Spinomed Active brace as soft. In their study, the no brace control group were transitioned to a Spinomed brace after six months; therefore, we excluded data past this time point. A total of six months of data was reported and used for this analysis. Kato et al. randomized patients into either a soft or rigid brace group, with 48 weeks of total follow-up data. Importantly, among all patients in the included studies, several were lost to follow-up due to one patient in a rigid brace and one patient in a soft brace with severe collapse progression, three patients in a soft brace requiring spinal surgery, one patient in a soft brace developing a neurological deficit, and three patients without a brace undergoing kyphoplasty.
Clinical outcome measures
Pain
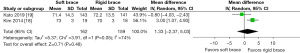
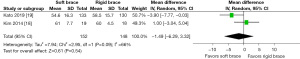
Kato et al. and Kim et al. reported pain on a 10-point visual analog scale (VAS). Pfeifer et al. measured pain on Miltner’s 4-point scale. We analyzed pain outcomes at baseline, and at 3–6 months given the available data. Comparisons using standardized mean differences were made between rigid and soft brace, rigid and no brace, and soft and no brace. Soft vs. rigid bracing did not show statistical significance at baseline (SMD =0.05, 95% CI: −0.24 to 0.35, P=0.72, I2=36%), or at 3–6 months (SMD 0.04, CI: −0.24 to 0.31, P=0.79, I2=28%). Soft bracing vs. no brace did not show statistical significance at baseline (SMD −0.13, CI: −0.66 to 0.41, P=0.65, I2=44%) or at 3–6 months (SMD =−1.23, CI: −2.50 to 0.05, P=0.06, I2=88%). Rigid bracing vs. no brace was not statistically different at baseline (SMD =−0.01, CI: −0.39 to 0.38, P=0.97, I2=0%). However, rigid bracing vs no brace at 3–6 months was significantly different, with less pain favoring the rigid brace group (SMD =−1.32, 95% CI: −1.89 to −0.76, P<0.05, I2=41%) (Figure 2). Subgroup analysis including both rigid and soft bracing groups similarly showed significantly less pain favoring the brace group (SMD =−1.27, 95% CI: −1.84 to −0.70, P<0.05, I2=70%) (Figure 3).


Kim et al. reports non-significant decreases in VAS scores at 3 months of brace usage, with a 2.98-point decrease in the no brace group at, a 4.27-point decrease in the soft brace group, and a 4.8-point decrease in the rigid brace group. Kato et al. similarly reported non-significant decreases in VAS scores at 3 months, with a 4.83-point reduction in the soft bracing group, and a 4.32-point reduction in the rigid bracing group (P=0.95). Of note, although the VAS differences in both studies were not significant in relation to one another, they all achieved a minimum clinically important difference (MCID) of at least 1.2 as described by Copay et al. (21). By 48 weeks, the soft brace group in the Kato et al. study had a 0.19 lower average pain score compared to rigid bracing, which was not significant (P=0.43)
Function
Function was reported by Kato et al. as JOABPEQ lumbar function scores. Kim et al. reported function using the Oswestry Disability Index (ODI). Alternatively, Pfeifer et al. used the Limitations of Daily Living scale devised by Leidig-Bruckner et al. (22). Soft vs. rigid bracing was not statistically different at baseline (SMD =0.18, CI: −0.19 to 0.55, P=0.35, I2=55%) or at 3–6 months (SMD =0.10, CI: −0.21 to 0.40, P=0.53, I2=37%). Soft bracing vs. no brace was not statistically different at baseline (SMD =−0.01, CI: −0.40 to 0.37, P=0.95, I2=0%) or at 3–6 months (SMD =−0.67, CI −2.28 to 0.95, P=0.42, I2=93%). Rigid bracing vs. no brace was not statistically different at baseline (SMD =0.41, CI: −0.06 to 0.87, P=0.09, I2=26%) or at 3–6 months (SMD =−0.67, CI: −1.47 to 0.13, P=0.10, I2=73%).
Quality of Life
Measures extracted for quality of life include the SF-36 MCS, EQ-5D, and the well-being score as described by Begerow et al. (23). Data was available at baseline and 3–6 months. There were no differences between any type of brace usage at baseline or at 3–6 months. Soft vs. rigid bracing was similar at baseline (SMD =−0.19, CI: −0.67 to 0.29, P=0.44, I2=72%) and 3–6 months (SMD =0.10, CI: −0.10 to 0.30, P=0.33, I2=0%). Soft bracing vs. no brace was similar at baseline (SMD =0.06, CI: −0.33 to 0.44, P=0.77, I2=0%) and 3–6 months. Rigid bracing vs. no brace was similar at baseline (SMD =0.41, CI: −0.69 to 1.50, P=0.47, I2=85%) and 3–6 months (SMD =0.95, CI: −0.22 to 2.14, P=0.28, I2=94%).
Radiographic assessment
Kato et al. and Kim et al. both assessed radiographic progression using AVBCP measurements at baseline and at 3 months. Outcomes for soft vs. rigid bracing were analyzed and similar at both time points (Figures 4,5). Of note, 24- and 48-week AVBCP values reported by Kato et al. showed no significant difference between soft and rigid bracing.
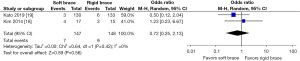
Opioid use
Both Kato et al. and Kim et al. reported the percentage of patients using opioid medications at three months post-injury in both soft and rigid bracing groups. 4.8% of patients treated with a soft brace used opioids at three months, whereas 6.1% of patients treated with a rigid brace used opioids (17,18). Our analysis showed no difference between these bracing modalities at three months (Figure 6).
Heterogeneity
High heterogeneity between studies was found in several comparisons. For pain this includes soft bracing vs. no brace at 3–6 months. For function this includes soft bracing vs. no brace at 3–6 months and soft vs. rigid bracing at 3–6 months. For quality of life this includes soft vs. rigid bracing at baseline, rigid bracing vs. no brace at baseline, and rigid vs. no bracing at 3–6 months. All other comparisons, including our finding of significant pain reduction for rigid bracing vs. no brace at 3–6 months, exhibited low to moderate heterogeneity. Factors leading to heterogeneity are difficult to assess given the small number of studies, but may be attributed to differences in sample size, treatment method, outcomes measures used, and follow-up length.
Grade of evidence
We found moderate quality evidence in support of rigid bracing for pain reduction in compression fractures within 3–6 months after injury (Table 2). Evidence was downgraded from high to moderate due to risk of bias in the study by Pfeifer et al., as the research was conducted by the company that created the orthoses. Low risk of bias was found in the studies by Kato et al. and Kim et al. A multi-domain assessment of bias was also performed and revealed some concerns in measurement and adherence due to the patients being aware of their treatment in all included studies, as well as an incomplete evaluation of compliance. This led to a high risk of bias for the domain evaluating deviation from intervention. Low risk of bias was found in randomization, outcome data, and selection domains.
Table 2
| No. of trials | Certainty assessment | No. of patients | Absolute effect (95% CI) | Certainty | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Rigid brace | No brace | ||||
| 3 | Serious | Not serious | Not serious | Not serious | None | 54 | 51 | SMD −1.32 (−1.89 to −0.76) | ⨁⨁⨁○ MODERATE | |
⨁⨁⨁○, signifies a moderate GRADE certainty. GRADE, Grades of Recommendation Assessment, Development and Evaluation; CI, confidence interval; SMD, standardized mean difference.
Discussion
Current knowledge regarding conservative management for thoracolumbar compression fractures is inadequate. Appropriate medical management for these osteoporotic injuries is paramount. Additionally, given the controversial indications surrounding kyphoplasty and vertebroplasty (24), a better understanding of the utility of conservative management is of utmost importance. Until recently, nonoperative management of vertebral compression fractures was difficult to study given the lack of available randomized controlled trials on the subject. We found three level 1 evidence studies between 2011 and 2019 that adequately analyzed the outcomes of bracing on compression fractures. Our analysis included 447 patients and found moderate quality evidence supporting the use of rigid bracing for pain reduction up to 6 months after injury. All comparisons for function, quality of life, radiographic kyphotic progression, and opioid use displayed statistically insignificant differences between bracing modalities.
Interestingly, two of our studies found similar clinically significant decreases in VAS pain scores after 3 months of brace usage, but no differences in outcomes between brace treatments. The third study (Pfeifer et al.) noted a significant benefit with bracing in terms of pain, function, and quality of life outcomes. However, these differences vanished when comparing soft to rigid bracing. Li et al. performed a randomized controlled trial of female patients over the age of 55 years that were treated for one week with a rigid TLSO and then transitioned to a separate rigid or soft brace for an additional two weeks. They found a significant improvement in pain and daily living limitations within both groups; however, there were no differences when comparing the brace groups to each other, and only three weeks of follow-up data were analyzed (25). In a prospective, nonrandomized trial, Meccariello et al. found that dynamic bracing provided superior pain reduction compared a 3-point brace at 3 and 6 months after injury (26). No difference in functional or radiographic outcomes was found.
Several prospective nonrandomized studies have failed to find results that would advocate for or against orthotic use (27,28). Murata et al. found improved function with rigid TLSO use as reported by the JOABPEQ at 3 and 6 months after injury; however, the study was limited to a single treatment arm (29). Other prospective, single arm studies have reported improved pain and function with use of a rigid brace from 3 to 9 months after injury (30,31).
Theoretically, limiting motion with a rigid brace has the advantage of better postural maintenance and less motion at the fracture site, which may prevent fracture collapse, reducing pain and risk for neurologic compromise. Our analysis revealed an equal number of included patients lost to follow-up for fracture collapse, but a larger number of patients in a soft brace requiring spinal surgery during brace treatment. However, rigid orthoses tend to be more cumbersome for patients. They may also put patient’s at risk for respiratory compromise and skin breakdown, leading to poor compliance rates (17). Given the lack of a convincing difference in outcomes between individual brace treatments as noted in the paragraphs above, as well as significant pain reduction at 6 months when analyzing both rigid and soft bracing combined (Figure 3), soft or dynamic bracing may be a reasonable alternative to rigid bracing.
Strengths of our meta-analysis include the presence of high-quality randomized trials, with comparable patient demographics and a large patient sample. Other systematic reviews have been performed on the topic of bracing for compression fractures, including a 2021 review of 7 studies that included a mix of randomized controlled trials and cohort studies (32). However, our study is the first of our knowledge to include only high-quality randomized controlled trials. Several limitations also exist within our study. First, we analyzed a small number of studies. This was limited by the low volume of randomized controlled trials with appropriate follow-up data available on the subject. Second, the included studies utilize various brands and types of braces, as well as variable treatment algorithms for how long each brace should be worn. Third, the study by Pfeifer et al. was funded by the company who developed the SpinoMed orthoses, resulting in potential publication bias. Fourth, there are many different brace types and manufacturers, and the lack of clearly defined criteria between brace types make comparisons less meaningful. Lastly, our study is limited to mostly female patients over the age of 50, making our results less generalizable to other patient groups.
Conclusions
Moderate quality evidence supports the use of rigid bracing for thoracic and lumbar compression fractures up to 6 months after injury in females over 50 years of age. There appear to be no benefits to patient function, quality of life, radiographic kyphosis, or opioid use, regardless of brace usage. There was no difference in outcomes between rigid and soft bracing; therefore, soft bracing may provide an adequate alternative if tolerated better by the patient. This data can be used to counsel patients on brace use following these injuries, as well as to direct future research in this area. More randomized-controlled trials with longer follow-up and more generalizable patient populations are required to further clarify treatment recommendations.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-22-78/rc
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-22-78/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-22-78/coif). RP reports that he received royalties from Globus, and consulting fees from Globus and Bioventus. IA has received consulting fees from Globus and research support from Orthofix and Nuvasive. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wright NC, Looker AC, Saag KG, et al. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res 2014;29:2520-6. [Crossref] [PubMed]
- Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res 2007;22:465-75. [Crossref] [PubMed]
- Srivastava M, Deal C. Osteoporosis in elderly: prevention and treatment. Clin Geriatr Med 2002;18:529-55. [Crossref] [PubMed]
- Miller PD. Management of severe osteoporosis. Expert Opin Pharmacother 2016;17:473-88. [Crossref] [PubMed]
- Lane JM, Russell L, Khan SN. Osteoporosis. Clin Orthop Relat Res 2000;139-50. [Crossref] [PubMed]
- Sambrook PN. Osteoporosis. Med J Aust 1996;165:332-6. [Crossref] [PubMed]
- Wang Y, Tao Y, Hyman ME, et al. Osteoporosis in china. Osteoporos Int 2009;20:1651-62. [Crossref] [PubMed]
- McCarthy J, Davis A. Diagnosis and Management of Vertebral Compression Fractures. Am Fam Physician 2016;94:44-50. [PubMed]
- Musbahi O, Ali AM, Hassany H, et al. Vertebral compression fractures. Br J Hosp Med (Lond) 2018;79:36-40. [Crossref] [PubMed]
- Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine; current options and considerations for treatment. Spine J 2006;6:479-87. [Crossref] [PubMed]
- Parreira PCS, Maher CG, Megale RZ, et al. An overview of clinical guidelines for the management of vertebral compression fracture: a systematic review. Spine J 2017;17:1932-8. [Crossref] [PubMed]
- Garg B, Dixit V, Batra S, et al. Non-surgical management of acute osteoporotic vertebral compression fracture: A review. J Clin Orthop Trauma 2017;8:131-8. [Crossref] [PubMed]
- Wood KB, Li W, Lebl DR, et al. Management of thoracolumbar spine fractures. Spine J 2014;14:145-64. [Crossref] [PubMed]
- Hoyt D, Urits I, Orhurhu V, et al. Current Concepts in the Management of Vertebral Compression Fractures. Curr Pain Headache Rep 2020;24:16. [Crossref] [PubMed]
- Shah LM, Jennings JW, Kirsch CFE, et al. ACR Appropriateness Criteria. J Am Coll Radiol 2018;15:S347-S64. [Crossref] [PubMed]
- Williams SA, Chastek B, Sundquist K, et al. Economic burden of osteoporotic fractures in US managed care enrollees. Am J Manag Care 2020;26:e142-9. [Crossref] [PubMed]
- Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. [Crossref] [PubMed]
- Kim HJ, Yi JM, Cho HG, et al. Comparative study of the treatment outcomes of osteoporotic compression fractures without neurologic injury using a rigid brace, a soft brace, and no brace: a prospective randomized controlled non-inferiority trial. J Bone Joint Surg Am 2014;96:1959-66. [Crossref] [PubMed]
- Kato T, Inose H, Ichimura S, et al. Comparison of Rigid and Soft-Brace Treatments for Acute Osteoporotic Vertebral Compression Fracture: A Prospective, Randomized, Multicenter Study. J Clin Med 2019;8:198. [Crossref] [PubMed]
- Pfeifer M, Kohlwey L, Begerow B, et al. Effects of two newly developed spinal orthoses on trunk muscle strength, posture, and quality-of-life in women with postmenopausal osteoporosis: a randomized trial. Am J Phys Med Rehabil 2011;90:805-15. [Crossref] [PubMed]
- Copay AG, Glassman SD, Subach BR, et al. Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the Oswestry Disability Index, Medical Outcomes Study questionnaire Short Form 36, and pain scales. Spine J 2008;8:968-74. [Crossref] [PubMed]
- Leidig-Bruckner G, Minne HW, Schlaich C, et al. Clinical grading of spinal osteoporosis: quality of life components and spinal deformity in women with chronic low back pain and women with vertebral osteoporosis. J Bone Miner Res 1997;12:663-75. [Crossref] [PubMed]
- Begerow B, Pfeifer M, Pospeschill M, et al. Time since vertebral fracture: an important variable concerning quality of life in patients with postmenopausal osteoporosis. Osteoporos Int 1999;10:26-33. [Crossref] [PubMed]
- Longo UG, Loppini M, Denaro L, et al. Conservative management of patients with an osteoporotic vertebral fracture: a review of the literature. J Bone Joint Surg Br 2012;94:152-7. [Crossref] [PubMed]
- Li M, Law SW, Cheng J, et al. A comparison study on the efficacy of SpinoMed® and soft lumbar orthosis for osteoporotic vertebral fracture. Prosthet Orthot Int 2015;39:270-6. [Crossref] [PubMed]
- Meccariello L, Muzii VF, Falzarano G, et al. Dynamic corset versus three-point brace in the treatment of osteoporotic compression fractures of the thoracic and lumbar spine: a prospective, comparative study. Aging Clin Exp Res 2017;29:443-9. [Crossref] [PubMed]
- Dionyssiotis Y, Trovas G, Thoma S, et al. Prospective study of spinal orthoses in women. Prosthet Orthot Int 2015;39:487-95. [Crossref] [PubMed]
- Hoshino M, Tsujio T, Terai H, et al. Impact of initial conservative treatment interventions on the outcomes of patients with osteoporotic vertebral fractures. Spine (Phila Pa 1976) 2013;38:E641-8. [Crossref] [PubMed]
- Murata K, Watanabe G, Kawaguchi S, et al. Union rates and prognostic variables of osteoporotic vertebral fractures treated with a rigid external support. J Neurosurg Spine 2012;17:469-75. [Crossref] [PubMed]
- Piazzolla A, Solarino G, Lamartina C, et al. Vertebral Bone Marrow Edema (VBME) in Conservatively Treated Acute Vertebral Compression Fractures (VCFs): Evolution and Clinical Correlations. Spine (Phila Pa 1976) 2015;40:E842-8. [Crossref] [PubMed]
- Shah S, Goregaonkar AB. Conservative Management of Osteoporotic Vertebral Fractures: A Prospective Study of Thirty Patients. Cureus 2016;8:e542. [Crossref] [PubMed]
- Kweh BTS, Lee HQ, Tan T, et al. The Role of Spinal Orthoses in Osteoporotic Vertebral Fractures of the Elderly Population (Age 60 Years or Older): Systematic Review. Global Spine J 2021;11:975-87. [Crossref] [PubMed]



