
Are modular pedicle screws associated with a high complication rate following posterior spinal fixation?
Highlight box
Key findings
• The use of modular head pedicle screws for posterior thoracolumbar instrumentation is not associated with an increased complication rate.
What is known and what is new?
• It is known that modular screws increase visualization of the surgical field during bony work around them.
• Modular pedicle screws present a viable option to allow surgeons to place pedicle screws without the risk of extra complications.
What is the implication, and what should change now?
• The extra flexibility associated with modular screws, such as inserting the screw shank first prior to performing decompression, decortication under the screw head, and having access to the lateral gutter for bone graft, interbody fusion, or other bony work without the protruding tulip or tower being in the way, does not increase the complication rate.
Introduction
Upon their introduction, pedicle screws revolutionized posterior spinal instrumentation in the surgical treatment of different spinal disorders by providing a reliable, strong hardware-bone purchase, allowing for improved control of each spinal segment and powerful potential for deformity correction (1). By adequately stabilizing spine segments, pedicle screws increase fusion rates with an acceptable rate of complications (2,3). Dr. Roy-Camille is credited as the first surgeon to use pedicle screws to treat unstable spinal fractures. He used the screws in conjunction with narrow plates to achieve fixation (4). That was a major breakthrough in spinal fixation because the screws provided immediate stability and rigid spine immobilization, and it was not necessary for intact laminae, facet joints or spinous processes, in order to be implanted in the vertebrae (5). Since then, the design and applicability of pedicle screws have undergone drastic changes. Wider core screws, which were stronger and had a lower risk of breakage, were made to resist the high stresses at the junction of screws and rods. New, more durable materials were used to manufacture the screws. Newer generations of pedicle screws reportedly have a lower rate of complications in comparison to the older generations (6-9). The development of new surgical techniques and improved screw designs may result in lower rates of complications. Among such recent developments is the introduction of the modular head screw. This screw is comprised of a threaded shank and separate head that can be intraoperatively assembled to the shank at any subsequent point in the case prior to rod placement.
The advent of modular screws has opened a new horizon in posterior spinal instrumentation. The surgeon has the option of inserting the screw shank first and then performing decompression, decortication under the screw head, having access to the lateral gutter for bone graft, interbody fusion, or other bony work without the protruding tulip or tower being in the way. In addition to providing great visualization intraoperatively, modular screws allow the surgeon to change the construct configuration after their insertion by allowing for a range of connector options. Despite these advantages, there is a paucity of available large series and clinical follow-up data to evaluate the effect of modular screws on hardware complications. Some have expressed concerns regarding the risk of potential hardware-related complications, especially screw-head dissociation, with the use of modular screws. The aim of the present, retrospective study is to determine the complication rates associated with the use of a modular pedicle screw system. We present this article in accordance with the STROBE reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-22-99/rc).
Methods
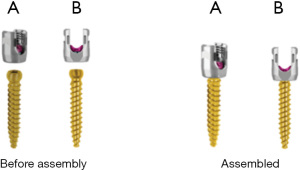
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Institutional Review Board (IRB) of The University of Iowa (No. 201912277). Informed consents were not obtained as it was a retrospective review of de-identified cases and the requirement was waived by the IRB. A retrospective chart review was performed on all adult patients undergoing posterior thoracolumbar spinal instrumentation and fusion for all indications with the use of a modular pedicle screw system (CREO AMP® Stabilization System, Globus Medical, Inc., Audubon, PA, USA) (Figure 1). All surgeries were performed at a single facility by a single surgeon between January 1, 2017, and December 31, 2019. Demographic and perioperative data were collected. All intra- and post-operative complications, which represented the primary outcome of the study, were recorded diligently. Length of hospital stay and follow-up, estimated blood loss, diagnosis, and comorbidities were other variables collected in the data set.
Statistical analysis
Descriptive statistical analysis was performed on the collected outcomes.
Results
There were 285 patients with varying indications (Table 1); 51% were female (144/285). The average age of patients was 61 (range, 23–86). Primary procedures were done in 186 cases (65%), while the 99 remaining cases (35%) underwent revision procedures. Length of hospital stay was 4.9 days on average (range, 1–25). The average follow-up was 17 months, with more than two-thirds of patients having more than a one-year follow-up. A total of 1,872 modular pedicle screws were inserted over the 3 years captured in this study. The average number of spinal levels instrumented per case was 3.7 (range, 1–23). As shown in Figure 2, cases with two levels of instrumentation had the highest frequency (82/285), followed by 1 level (73/285) and 3 levels (31/285).
Table 1
| Indications | Number | Frequency |
|---|---|---|
| Trauma | 15 | 5% (15/285) |
| Spondylolisthesis | 64 | 22% (64/285) |
| Deformity | 65 | 23% (65/285) |
| Pseudarthrosis | 10 | 4% (10/285) |
| Spinal stenosis | 48 | 17% (48/285) |
| Lumbar radiculopathy, degenerative disk disease, ASD | 48 | 17% (48/285) |
| Tumor (primary and secondary) | 21 | 7% (21/285) |
| Infection (osteomyelitis, discitis, epidural abscess) | 14 | 5% (14/285) |
ASD, adjacent segment disease.
Complications
The overall rate of complications was 20.8%. The rate of all hardware-related complications combined is 5.3%. Table 2 presents the complications that occurred during index hospitalization and after discharge. There were 25 reoperations: six due to non-union and rod breakage, five for screw loosening, seven for adjacent segment disease, one for acute postoperative radiculopathy, one for epidural hematoma, two for a deep surgical site infection, and three for a superficial surgical site infection. There were nine cases of superficial and two cases of deep surgical wound infections. All infections were detected less than 6 weeks after surgery and managed accordingly without sequelae. Dural tears occurred in 6 cases (2%). None of the 1,872 modular pedicle screws in this series had any screw head dissociation or failure at the rod screw junction. However, there were 6 cases of rod breakage (2%) and screw loosening (2%). Two screws migrated (0.7%) and one screw broke (0.3%) during postoperative period. There were no cases of screw head disassembly from the shank reported in the study. There was one death during hospitalization, due to respiratory failure, of a 66-year-old male with metastatic renal cell carcinoma who had undergone T11-pelvic instrumentation.
Table 2
| Complication type | Number of events, N (%) | Number of reoperations, N (%) |
|---|---|---|
| Medical complications | 5 (1.8) | |
| Pneumonia | 2 (0.7) | |
| Respiratory failure | 1 (0.3) | |
| Myocardial ischemia | 1 (0.3) | |
| Stroke | 1 (0.3) | |
| Surgical complications | 22 (7.7) | |
| Dural tear | 6 (2.0) | |
| Wound infection and dehiscence | 11 (4.0) | 5 (0.7) |
| Nerve root injury | 3 (1.0) | 1 (0.3) |
| Hematoma | 2 (0.7) | 1 (0.3) |
| Hardware-related complications | 15 (5.3) | |
| Rod breakage | 6 (2.0) | |
| Screw loosening | 6 (2.0) | 5 (1.7) |
| Screw pullout/migration | 2 (0.7) | |
| Screw breakage | 1 (0.3) | |
| Long-term complications | 17 (6.0) | |
| Adjacent segment disease | 7 (2.5) | 7 (2.5) |
| Proximal junctional kyphosis | 2 (0.7) | |
| Nonunion | 8 (3.0) | 6 (2.0) |
Discussion
In this series, 285 consecutive cases were reported in which modular head pedicle screws were utilized for posterior instrumentation of the thoracolumbar spine for a variety of indications. Modular screw systems have the potential risk of screw separation from the modular head or separation of screw head from the rod early in the postoperative period.
In this study, the authors reported a low overall hardware-related complication rate and not a single separation of a modular screw head from the screw in 1,872 consecutively inserted modular pedicle screws. The rate of other implant-related complications was comparable to or lower than other pedicle screw systems reported in the literature.
The rate of screw loosening, which is a multifactorial complication, has been reported to be between less than 1% (in non-osteoporotic patients) (10) and up to 60% (in osteoporotic cases) (11). The rate of pedicle screw loosening in this study was 2%. All cases occurred in patients older than 60 years old who were at high risk for age-related osteoporosis. Zhao et al. reported 8 cases (1.1%) of screw breakage in 781 patients treated for thoracolumbar fracture with posterior fixation (12). In this study, among 1,872 modular screws inserted, there was a single case (0.3%) of pedicle screw breakage at S1 that was detected 13 months following surgery for degenerative scoliosis in a 75-year-old male.
In the current study, there was also a single case of screw pullout detected 4 months after surgery for a degenerative scoliosis treated by fusion from T9 to pelvis in a 60-year-old female. Both pedicle screws from T9 (the highest instrumented vertebral level) were involved due to pathologic fracture of T9. The patient was admitted for a revision, and the fusion extended to T4. Osteoporosis, excessive strain on the implant, sagittal imbalance, screw hole preparation techniques, insertional torque, and direction of screw placement may affect screw pullout strength (13-19). Kim et al. (20) reported rod breakage in 6.7% of primary and 33.3% of revision surgeries for adult spinal deformities. There were 6 cases (2%) of rod breakage in the current series. Five of those cases occurred in patients treated for spinal deformity (2 revisions and 3 primaries in 65 patients with deformity). All of these cases had long constructs (8–14 levels) and the breakage occurred in the lower lumbar and lumbosacral area, where stress is higher in a long construct (19).
There were certain limitations with this study. Although the average follow-up period was 17 months, and more than two-thirds of patients were followed more than one year, there were a subgroup of patients with much shorter follow-up, for whom, the authors were not able to report the potential long-term complications.
Conclusions
Based on this single-institution experience, the use of modular head pedicle screws for posterior thoracolumbar instrumentation is not associated with an increased complication rate. The modular screw system provides a safe method to stabilize the spine posteriorly without obstructing the view for the surgeon during a critical part of the operation. Future longer-term and multi-center studies could address its potential benefits in specific radiographic measures and/or specific patient populations.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-22-99/rc
Data Sharing Statement: Available at https://jss.amegroups.com/article/view/10.21037/jss-22-99/dss
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-22-99/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-22-99/coif). AJP is a paid consultant to Medtronic, Globus Medical Inc. and United Healthcare; has received research support from Globus Medical Inc., Medtronic, Lumbar Spine Research Society, and Cervical Spine Research Society, Trustees of Dartmouth College, and RDB Bioinformatics. BB and NT are salaried employees and have stock option of Globus Medical Inc. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Institutional Review Board of The University of Iowa (No. 201912277). IRB approval was obtained before initiation of this study. Informed consents were not obtained as it was a retrospective review of de-identified cases and the requirement was waived by the IRB.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Boos N, Webb JK. Pedicle screw fixation in spinal disorders: a European view. Eur Spine J 1997;6:2-18. [Crossref] [PubMed]
- Faraj AA, Webb JK. Early complications of spinal pedicle screw. Eur Spine J 1997;6:324-6. [Crossref] [PubMed]
- Esses SI, Sachs BL, Dreyzin V. Complications associated with the technique of pedicle screw fixation. A selected survey of ABS members. Spine (Phila Pa 1976) 1993;18:2231-8; discussion 2238-9. [Crossref] [PubMed]
- Roy-Camille R, Saillant G, Berteaux D, et al. Osteosynthesis of thoraco-lumbar spine fractures with metal plates screwed through the vertebral pedicles. Reconstr Surg Traumatol 1976;15:2-16. [PubMed]
- Gulbrandsen TR, Muffly SA, Shamrock A, et al. Total Hip Arthroplasty: Direct Anterior Approach Versus Posterior Approach in the First Year of Practice. Iowa Orthop J 2022;42:127-36. [PubMed]
- Crawford MJ, Esses SI. Indications for pedicle fixation. Results of NASS/SRS faculty questionnaire. North American Spine Society and Scoliosis Research Society. Spine (Phila Pa 1976) 1994;19:2584-9. [Crossref] [PubMed]
- Katonis P, Christoforakis J, Kontakis G, et al. Complications and problems related to pedicle screw fixation of the spine. Clin Orthop Relat Res 2003;86-94. [Crossref] [PubMed]
- West JL 3rd, Ogilvie JW, Bradford DS. Complications of the variable screw plate pedicle screw fixation. Spine (Phila Pa 1976) 1991;16:576-9. [Crossref] [PubMed]
- Yuan HA, Garfin SR, Dickman CA, et al. A Historical Cohort Study of Pedicle Screw Fixation in Thoracic, Lumbar, and Sacral Spinal Fusions. Spine (Phila Pa 1976) 1994;19:2279S-96S. [Crossref] [PubMed]
- Di Silvestre M, Parisini P, Lolli F, et al. Complications of thoracic pedicle screws in scoliosis treatment. Spine (Phila Pa 1976) 2007;32:1655-61. [Crossref] [PubMed]
- El Saman A, Meier S, Sander A, et al. Reduced loosening rate and loss of correction following posterior stabilization with or without PMMA augmentation of pedicle screws in vertebral fractures in the elderly. Eur J Trauma Emerg Surg 2013;39:455-60. [Crossref] [PubMed]
- Zhao Q, Zhang H, Hao D, et al. Complications of percutaneous pedicle screw fixation in treating thoracolumbar and lumbar fracture. Medicine (Baltimore) 2018;97:e11560. [Crossref] [PubMed]
- Bianco RJ, Arnoux PJ, Wagnac E, et al. Minimizing Pedicle Screw Pullout Risks: A Detailed Biomechanical Analysis of Screw Design and Placement. Clin Spine Surg 2017;30:E226-32. [Crossref] [PubMed]
- Lee SJ, Lee JH, Lee HJ, et al. Pullout strength of pedicle screws using cadaveric vertebrae with or without artificial demineralization. Spine J 2021;21:1580-6. [Crossref] [PubMed]
- Gautschi OP, Schatlo B, Schaller K, et al. Clinically relevant complications related to pedicle screw placement in thoracolumbar surgery and their management: a literature review of 35,630 pedicle screws. Neurosurg Focus 2011;31:E8. [Crossref] [PubMed]
- Varghese V, Saravana Kumar G, Krishnan V. Effect of various factors on pull out strength of pedicle screw in normal and osteoporotic cancellous bone models. Med Eng Phys 2017;40:28-38. [Crossref] [PubMed]
- Ye YX, Huang DG, Hao DJ, et al. Screw Pull-out Strength After Pedicle Screw Reposition: a Finite Element Analysis. Spine (Phila Pa 1976) 2022; Epub ahead of print. [Crossref] [PubMed]
- Zaidi Q, MacNeille R, Ramos O, et al. Predicting Pedicle Screw Pullout and Fatigue Performance: Comparing Lateral Dual-Energy X-Ray Absorptiometry, Anterior to Posterior Dual-Energy X-Ray Absorptiometry, and Computed Tomography Hounsfield Units. Int J Spine Surg 2023;17:43-50. [Crossref] [PubMed]
- Zdeblick TA, Kunz DN, Cooke ME, et al. Pedicle screw pullout strength. Correlation with insertional torque. Spine (Phila Pa 1976) 1993;18:1673-6. [Crossref] [PubMed]
- Kim WJ, Shin HM, Song DG, et al. Comparison of Clinical Outcomes and Complications of Primary and Revision Surgery Using a Combined Anterior and Posterior Approach in Patients with Adult Spinal Deformity and Sagittal Imbalance. Clin Orthop Surg 2021;13:196-206. [Crossref] [PubMed]



