
Resolution of brachioradial pruritus following anterior cervical discectomy and fusion: a case report
Highlight box
Key findings
• This patient underwent anterior cervical discectomy and fusion (ACDF) and later revision for cervical radiculopathy, manifesting as brachioradial pruritus. This was secondary to foraminal stenosis causing compression of the exiting cervical nerve root.
What is known and what is new?
• Brachioradial pruritus is localized pruritus of the dorsolateral arm and forearm most often affecting middle-aged women with lighter skin tones. Ultraviolet radiation and cervical radiculopathy are thought to be possible causes. Brachioradial pruritus is primarily managed conservatively.
• This case report offers evidence that cervical radiculopathy is a potential cause of brachioradial pruritis. The patient had initial relief of the pruritis after surgical decompression, followed by a brief period of symptom recurrence two months post-operation. Radiographs showed hardware displacement and restenosis of the cervical neuroforamen. The patient then underwent hardware removal and revision ACDF, which were curative.
What is the implication, and what should change now?
• ACDF is a relatively safe and viable treatment option for refractory brachioradial pruritus when there is corelative cervical nerve root compression.
Introduction
Brachioradial pruritus (BRP) is a condition characterized by localized pruritus of the dorsolateral arm and forearm. While the etiology of BRP remains somewhat controversial, patients with BRP often present similarly. Patients typically are middle-aged fair-skinned females who complain of itching and burning localized to sun-exposed areas including the neck, shoulders, arms, and forearms. Because of the involvement of sun-exposed areas, BRP was initially believed to be solely caused by ultraviolet (UV) radiation. However, the literature reveals numerous cases associated with cervical neuropathy (1-8). Pruritus as a symptom presents an interesting challenge, as it is non-specific. Consequently, patients suffering from BRP are frequently seen by different specialists and forming the diagnosis is often delayed. Here we present a case of BRP that was partially obscured for years by a significant dermatologic history. The patient presented to an orthopedic surgeon after numerous failed dermatologic interventions. The patient subsequently underwent anterior cervical discectomy and fusion (ACDF) with resolution of symptoms that later returned due to migration of surgical implants. The patient’s recurrent symptoms again resolved after ACDF revision. We present this case in accordance with the CARE reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-22-90/rc).
Case presentation
A 72-year-old Caucasian female with previous dermatologic history presented to the clinic with neck pain and right arm and forearm pruritus, which had been ongoing for several years without a known cause. She also complained of difficulty walking and balancing, numbness and weakness of the hands, hand clumsiness, and frequently dropping things. The patient was being followed by dermatology for skin cancer, eczematous dermatitis, lichen simplex chronicus, and underwent frequent skin exams. Her pruritus was isolated to the C6 dermatome. She had been treated by dermatologic providers with multiple topical agents, oral agents, and injections that have been shown to have success with neuropathic itching but without significant or long-term relief. She was then referred to our orthopedic practice for evaluation for possible BRP.
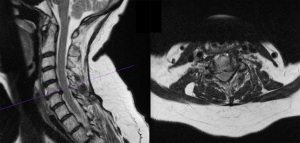
Radiographs and computed tomographic scans of the cervical spine showed severe disc degeneration at C5-C6 and collapse of the disc space (Figure 1). Magnetic resonance imaging (MRI) of the cervical spine showed disc herniation at C5-C6 causing mild cord compression with bilateral foraminal stenosis (Figure 2).

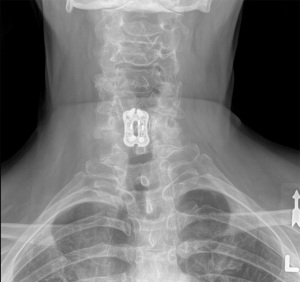
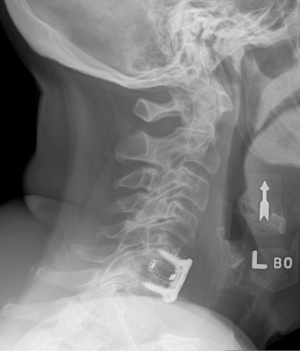
The patient subsequently underwent ACDF without any intraoperative complications. The patient was seen in the hospital on post-operative day one and reported complete resolution of her pre-operative symptoms. Initial postoperative recovery was without incident. At her 6- and 12-week post-operative appointments, radiographs demonstrated migration of the cage, and the patient reported a return of mild symptoms that gradually worsened (Figures 3,4). She was taken back to surgery 4 months after the initial operation for ACDF revision. Again, the patient reported resolution of symptoms while in the hospital on post-operative day one. The patient recovered well from the revision and X-rays did not demonstrate any migration (Figures 5,6). The symptoms had completely resolved at 6-, 12-, and 24-month follow-up appointments (Figures 7,8).




All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
BRP, a chronic form of localized neurocutaneous dysesthesia in the dorsolateral upper extremities, shoulders, or neck, has an unclear etiology. UV radiation and cervical radiculopathy/neuropathy are hypothesized as the main etiologic factors (1-8). While its origin is uncertain, forming the diagnosis is relatively simple and is made clinically, often in a dermatologic setting; further testing is rarely utilized in establishing the diagnosis (9). BRP most commonly affects middle-aged women with lighter skin tones. Symptoms include itching, tingling, and burning in the C5-C6 dermatomes that present bilaterally and worsen in the summer months. A physical exam may reveal excoriations, prurigo nodules, or lichenification as a result of repetitive scratching.
Treatment options include decreasing sun exposure, ice application, topical medications, systemic medications, and in very rare circumstances, surgery. Itching relieved from ice, known as the ice-pack sign, is considered pathognomonic for BRP (10). Commonly reported topical medications include steroids, antihistamines, anesthetics, and capsaicin. Commonly reported oral medications include gabapentin, amitriptyline, and antipsychotics (9). Many of these medications have shown efficacy towards other neuropathic pain syndromes (7,11). Our literature search revealed only two reports where surgical decompression was used to treat BRP, which lends to the overall success of conversative treatment (7,12). Like those reports, ACDF was also used for this case report. However, this case report is unique because the patient had a brief period of symptom recurrence two months post-operation as supported by displacement of the cage on imaging. The patient then underwent implant removal and revision with the use of an anterior plate. She has been symptom free since the most recent 2-year post-operative evaluation.
BRP is a rare disease and the number of case reports where surgery was used for treatment is significantly limited. The purpose of this case study is to expound on surgical intervention as a relatively safe and viable treatment option for certain patients with refractory BRP that have failed conservative management. We hope to better familiarize the orthopedic community with BRP.
Conclusions
BRP is a rare disease that is often treated conservatively with oral and/or topical medications. In situations where conservative measures are not successful, surgical management has demonstrated to be low-risk and curative.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-22-90/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-22-90/coif). JT is a current employee of Steward Medical Group. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Waisman M. Solar pruritus of the elbows (brachioradial summer pruritus). Arch Dermatol 1968;98:481-5. [Crossref] [PubMed]
- Fisher DA. Brachioradial pruritus: a recurrent solar dermopathy. J Am Acad Dermatol 1999;41:656-8. [Crossref] [PubMed]
- Wallengren J. Brachioradial pruritus: A recurrent solar dermopathy. J Am Acad Dermatol 1999;41:657-8. [Crossref] [PubMed]
- Heyl T. Brachioradial pruritus. Arch Dermatol 1983;119:115-6. [Crossref] [PubMed]
- Goodkin R, Wingard E, Bernhard JD. Brachioradial pruritus: cervical spine disease and neurogenic/neuropathic [corrected] pruritus. J Am Acad Dermatol 2003;48:521-4. [Crossref] [PubMed]
- Marziniak M, Phan NQ, Raap U, et al. Brachioradial pruritus as a result of cervical spine pathology: the results of a magnetic resonance tomography study. J Am Acad Dermatol 2011;65:756-62. [Crossref] [PubMed]
- Binder A, Fölster-Holst R, Sahan G, et al. A case of neuropathic brachioradial pruritus caused by cervical disc herniation. Nat Clin Pract Neurol 2008;4:338-42. [Crossref] [PubMed]
- Pinto AC, Wachholz PA, Masuda PY, et al. Clinical, epidemiological and therapeutic profile of patients with brachioradial pruritus in a reference service in dermatology. An Bras Dermatol 2016;91:549-51. [Crossref] [PubMed]
- Mirzoyev SA, Davis MD. Brachioradial pruritus: Mayo Clinic experience over the past decade. Br J Dermatol 2013;169:1007-15. [Crossref] [PubMed]
- Bernhard JD, Bordeaux JS. Medical pearl: the ice-pack sign in brachioradial pruritus. J Am Acad Dermatol 2005;52:1073. [Crossref] [PubMed]
- Baron R. Mechanisms of disease: neuropathic pain--a clinical perspective. Nat Clin Pract Neurol 2006;2:95-106. [Crossref] [PubMed]
- Salzmann SN, Okano I, Shue J, et al. Disabling Pruritus in a Patient With Cervical Stenosis. J Am Acad Orthop Surg Glob Res Rev 2020;4:e19.00178.


