
Differences in evaluation and management coding of outpatient clinic visits for patients undergoing elective spine surgery with use of a standardized template
Highlight box
Key findings
• After the implementation of the 2021 E&M billing changes, there was a statistically significant increased level of billing for templated notes for lumbar microdiscectomy (P=0.013) but not for clinic visits where patients underwent an anterior cervical discectomy and fusion (ACDF) in 2021.
What is known and what is new?
• Providers often do not have a standardized method for including information in their clinic notes.
• This study compares templated and non-templated documentation in terms of reimbursement.
What is the implication, and what should change now?
• Standardization of template use should be considered for all tertiary care facilities to ensure proper documentation, appropriate reimbursements, and reduces variability of billing among surgeons.
Introduction
Studies have shown that lack of physician involvement in coding for both hospital and clinic visits can result in up to 25% decreased reimbursement in the US (1). One specific study reported an estimated revenue loss of over $80,000 in a 1-year period at a university outpatient clinic due to fewer level 4 visits when compared to Medicare normative data (2). These discrepancies result from incomplete clinical documentation which results in inadequate medical reimbursements (3). Previous studies have demonstrated that electronic medical record template use improves accuracy and completeness of both operative and clinical notes in orthopedic surgery, contributing to ease in interdisciplinary communication (4-6). Discrepancies in documentation of outpatient clinic visits could potentially result in inappropriate reimbursement.
One method to address accuracy of medical record and billing is the use of standardized templates. Incorporating standardized templates may result in a noticeable difference in tertiary care settings, where physicians with different backgrounds practice, and at teaching institutions where rotating residents of all levels of training often author clinic notes. In our study, we chose to analyze two common procedures performed at our institution, one in the cervical and one in the lumbar spine for generalizability. The purpose of this study is to (I) assess differences in re-imbursement between templated and non-templated outpatient documentation for patients who eventually underwent single level lumbar microdiscectomy and anterior cervical discectomy and fusion (ACDF) both before US Centers for Medicare and Medicaid Services (CMS) and after the E&M billing changes were implemented in 2021; and (II) determine if standardized templates are preferred for both medical coders and resident physicians. We present this article in accordance with the STROBE reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-22-91/rc).
Methods
Outpatient clinic documentation
This was a single institution retrospective review from data collected at a tertiary care center between 2018 and 2019 as well as 2021. Patients ranging from 18–65 years old who underwent either a lumbar microdiscectomy or single-level ACDF were included in the study. Up to four different spine surgeons who were responsible for these outpatient clinic visits that resulted in subsequent surgery were included in each time period. These spine surgeons had disparate backgrounds, with one surgeon having military and academic experience of over 20 years, a second with private practice and academic experience of over 20 years, a third being in an academic practice for over 10 years, and a fourth being academic practice for less than 5 years. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional review board of University of Missouri-Columbia (No. 2013104) and informed consent was taken from all individual participants.
From 2018 to 2019, the average age of the patients was 40 years old. Ninety percent of patients were Caucasian with an average of 1.43 comorbidities. Current or prior smokers comprised 46% of patients included in this study. Other comorbidities included hypertension, major depression, chronic pain syndrome, fibromyalgia, chronic obstructive lung disease, cancer, and chronic renal failure. The coding level of each office visit in which operative management was collected. IRB approval was obtained for the study. The total number of visits for lumbar discectomies was 46 and ACDFs was 41. The average number of visits in the year per surgeon were 15.3. Given the new E&M billing change, additional data was collected for 35 patients were seen by four spine surgeons for lumbar microdiscectomy and 30 patients for ACDF between January and December of 2021.
The standard template utilized in the study included information regarding the patient’s symptoms (onset, location, duration, characterization, aggravating factors, relieving factors) as, screening for myelopathy (dexterity, gait), bowel and bladder concerns, previous back surgery, as well as prior treatments for their current chief complaint. There was also a set physical exam template to include muscle strength, sensation exam, reflexes and other upper motor neuron signs.
Billing levels for all office visits prior to the surgery were collected. Outpatient clinic visit E&M codes were collected, with the most common being 99203, 99204, 99213, and 99214. The higher level visit was used for data analysis regardless of when advanced imaging results were obtained or if it was an initial versus follow-up appointment. Surgical intervention was recommended in the included clinic visit.
Resident physician response to template use
Nine residents completed a five-item multiple choice online survey assessing their preference in using a template and the value of using templates for clinical documentation during their spine rotation. Additionally, they were asked if they planned to use templates outside of their spine rotation.
Coders response to template use
Coders completed a two-item questionnaire to assess whether they found templates helpful when evaluating clinical documentation for billing purposes, and whether they preferred the utilization of templates by resident physicians.
Statistical methods
Continuous variables were reported with means and standard deviations. Categorical analysis was performed with percentages. Analysis of variance was utilized when comparing data among three or more surgeons and significance was determined when P<0.05.
Results
Outpatient clinic documentation
According to Figure 1, between 2018 and 2019 for lumbar microdiscectomy patients, the average level of billing was 3.2±0.4 for surgeon 1, 3.5±0.6 for surgeon 2, and 2.9±0.8 for surgeon 3. This results in an estimated reimbursement of $1,693 for surgeon 1, $1,954 for surgeon 2, and $1,401 for surgeon 3 for 14 visits. Our institution performs approximately 10,000 surgeries per year and if these billing levels were extrapolated across all procedures for each surgeon’s documentation patterns, this would translate to $713,664 vs. $820,695 vs. $590,357, with an increase of $107,032–$230,338 when comparing templated versus non-templated notes.
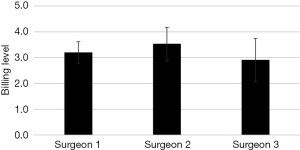
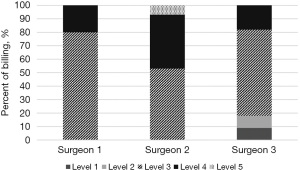
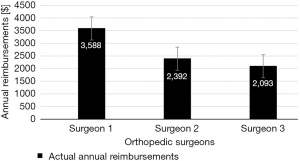
Only surgeon 3 billed a level 1 (1/11 patients) and level 2 (1/11 patients) clinic visit, and only surgeon 2 billed a level 5 clinic visit (1/15 patients). Variability was represented in Figure 2, where surgeon 1 demonstrated mostly level 3 clinic visits (80%) and surgeon 2 with a mix of level 3 (53%), level 4 (40%), and level 5 (7%) clinic visits. Surgeon 3 had 64% of level 3 clinic visits, but remaining clinic visits had billing levels spread across level 1 (9%), level 2 (9%), and level 4 (18%). Based on the RVU schedule generated by the RUC committee, this equates to re-imbursement rates of $3,588 for surgeon 1, $2,392 for surgeon 2, and $2,093 for surgeon 3 when accounting for only level 3 clinic visits (Figure 3).
Interestingly, even after the implementation of the 2021 E&M billing changes, there was a statistically significant increased level of billing for templated notes for lumbar microdiscectomy (P=0.013). Table 1 shows the mean levels of coding for 35 lumbar microdiscectomy patients seen by four different surgeons, which ranges from 3.25 to 4.
Table 1
| Surgeon | N | Mean level of coding | Standard deviation |
|---|---|---|---|
| Surgeon 1 | 4 | 3.25 | 0.500 |
| Surgeon 2 | 9 | 3.56 | 0.527 |
| Surgeon 3 | 17 | 3.88 | 0.332 |
| Surgeon 4 | 5 | 4.00 | 0.00 |
| Total | 35 | 3.74 | 0.433 |
There was also a statistically significant higher level of billing for clinic visits from 2018–2019 for ACDF patients (P<0.001). A total of 52 patients were seen by 3 surgeons with mean levels of coding ranging from 3.09 to 3.84 (Table 2). However, this did not translate to the clinic visits for patients who underwent ACDF in 2021. When data was aggregated for all the patients from 2021 who either underwent lumbar microdiscectomy or ACDF, using a template still resulted in a statistically significant higher level of billing (P<0.05).
Table 2
| Surgeon | N | Mean level of coding | Standard deviation |
|---|---|---|---|
| Surgeon 1 | 11 | 3.09 | 0.302 |
| Surgeon 2 | 22 | 3.32 | 0.477 |
| Surgeon 3 | 19 | 3.84 | 0.688 |
| Total | 52 | 3.46 | 0.609 |
ACDF, anterior cervical discectomy and fusion.
Residents physician response to template use
On the spine surgery rotation, only one attending physician encouraged the use of a standardized template for each clinic visit. Of the 17 residents who were eligible to respond, nine completed the survey, which was a 52.9% response rate (Figure 4). Over half of respondents indicated that template use during their spine rotation was somewhat helpful (55.6%). A third of the residents were undecided about template use outside of their spine rotation. Not surprisingly, 33.3% of residents thought templates made patient presentations easier. Over 40% of residents thought that the benefit of proper documentation with a standardized template was justified.
Coders response to template use
All the coders working with these same spine surgeons at the time were surveyed and preferred a template for coding and billing purposes due to improved accuracy and ease of clinical documentation on review.
Discussion
Standardized templates to reduce variability in medical billing for the same surgery is a key issue for orthopedic surgeons because reimbursement in Orthopaedic surgery is downtrending (7). Walker et al. documented a 29% decrease in inflation-adjusted Medicare reimbursement for work relative value units (RVUs) in 2016 across all subspecialties, except oncology when compared to rates in 2000 (7). The same study also demonstrated the need for active involvement of orthopedic attending physicians and residents in coding documentation and fee-schedule representation (7). In this study, a substantial degree of variability for billing levels were observed between three orthopedic surgeons managing lumbar disc herniations with microdiscectomies. If all 3 surgeons had level 3 clinic visits 80% of the time whenever a patient is seen for a microdiscectomy preoperatively for 52 patient visits annually, as per this study from 2018–2019 by surgeon 1, the total annual reimbursement of all 3 surgeons, based on level 3 billing code 99203, would be $9,867. However, with surgeon 2 and surgeon 3 having only 53% ($2,392 annual) and 64% ($2,093 annual) of clinic visits billed at level 3, respectively, the net annual re-imbursement in this specific tertiary care center for lumbar microdiscectomy level 3 clinic visits is $8,073. This equates to a net loss of $1,803 annually when only considering level 3 clinic visits for microdiscectomy. However, when comparing all levels of billing for clinic visits, surgeon 2 was the only attending who consistently utilized a standardized template, resulting in improved overall annual reimbursement, with a higher percentage of both level 4 and level 5 clinic visits.
Notably, with novel E&M changes in 2021, a standardized template also resulted in statistically significant higher levels of coding for lumbar microdiscectomy patients, but not for ACDF patients. This may be due to the inherent high acuity of patient care and documentation provided in ACDF versus microdiscectomy patients. However, when ACDF and lumbar microdiscectomy patients from 2021 were combined, there was a statistically significant increase in level of billing with a standardized template. This could be due to a limitation of sample size both for the total number of patients included and number of patients for each surgery. Generalizability of this study is also difficult to determine as this study was only regarding select spine cases in an outpatient/23-hrs stay setting and each surgeon has a unique background. However, each institution could perform small quality improvement studies after implementation of a standardized template to help maximize re-imbursement and improve accuracy of documentation. Spine surgeons, however, may choose not to utilize templates for several reasons including ease of dictation, amount of time spent filling out a template, and personal preference.
The majority of residents (55.6%) reported usefulness of a standardized template during their spine rotation. Coders also indicated their preference for standardized templates as a means for improving clinical documentation completeness and enhancing documentation that supports medical necessity. The data in this study only considers patients managed with lumbar microdiscectomy or ACDF. Therefore, the aggregate financial impact that includes all preoperative billed clinical visits could be substantially greater. Standardization is crucial as previous studies have emphasized the need for improving resident instruction in coding in effort to enhance the accuracy of claims data (8). The use of a template for clinical documentation can also serve as a means for improving resident instruction in coding. Other studies have shown that coding errors and omissions in patients resulted in cumulative loss of revenue of £46,750 ($60,130.08) over the course of one year (3). One study by Murphy et al. has shown low levels of concordance between resident and attending surgeons in CPT coding, possibly due to a lack of training (9). The use of a standardized template could also potentially alleviate discrepancies in CPT coding through accurate documentation and should be utilized whenever feasible.
Conclusions
When a standardized template was utilized for clinical documentation, billing trended toward higher levels both prior to and after the 2021 CMS E&M changes for lumbar microdiscectomy patients, resulting in higher clinical visit reimbursement for the same diagnosis. Further studies with a larger sample size and other diagnoses could be explored for application to all Orthopaedic subspecialities. In a large volume academic clinical practice with multiple providers, the financial impact could prove to be substantial for preoperative documentation alone when a templated documentation is used.
Acknowledgments
Funding: Funding was obtained from within the Department of Orthopaedic Surgery at the University of Missouri-Columbia.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-22-91/rc
Data Sharing Statement: Available at https://jss.amegroups.com/article/view/10.21037/jss-22-91/dss
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-22-91/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-22-91/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional review board of University of Missouri-Columbia institutional review board (No. 2013104) and informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Filler BC. Coding basics for orthopaedic surgeons. Clin Orthop Relat Res 2007;105-13. [Crossref] [PubMed]
- Dezfuli B, Smith JL. Level of billing as a function of resident documentation and orthopedic subspecialty at an academic multispecialty orthopedic surgery practice. Orthopedics 2012;35:e1655-8. [Crossref] [PubMed]
- Harshavardhana NS, Sahu A, Maret S, et al. Payment by results (PbR) in orthopaedic trauma: Where are we losing? Abstracts Injury Extra 2009;40:183-235. [Crossref]
- Al-Dadah K, Evans O, Ali F. Optimizing knee arthroscopy documentation using a new template. Br J Hosp Med (Lond) 2014;75:227-30. [Crossref] [PubMed]
- Cao J, Farmer R, Carry PM, et al. Standardized Note Templates Improve Electronic Medical Record Documentation of Neurovascular Examinations for Pediatric Supracondylar Humeral Fractures. JB JS Open Access 2017;2:e0027.
- Urchek RJ, Morscher MA, Steiner RP, et al. Orthopaedic Resident Use of an Electronic Medical Record Template Does Not Improve Documentation for Pediatric Supracondylar Humerus Fractures. J Am Acad Orthop Surg 2019;27:e395-e400. [Crossref] [PubMed]
- Walker R, Morrison Z, Campbell M. Trends in Orthopedic Surgery Reimbursement From 2000 to 2015. Orthopedics 2020;43:187-90. [Crossref] [PubMed]
- Jones K, Lebron RA, Mangram A, et al. Practice management education during surgical residency. Am J Surg 2008;196:878-81; discussion 881-2. [Crossref] [PubMed]
- Murphy RF, Littleton TW, Throckmorton TW, et al. Discordance in current procedural terminology coding for foot and ankle procedures between residents and attending surgeons. J Surg Educ 2014;71:182-5. [Crossref] [PubMed]



