
Sagittal alignment in operative degenerative lumbar spondylolisthesis: a scoping review
Highlight box
Key findings
• There is limited analysis of global sagittal spinal alignment in degenerative lumbar spondylolisthesis (DLS). Although, there is an increasing prevalence of studies investigating sagittal spinal alignment in DLS surgery the quality of the currently available literature is of overall low evidence and largely retrospective in nature.
What is known and what is new?
• The benefit of surgical intervention for DLS patients with neurologic symptoms is well-established; however, the optimal treatment for this population remains unclear. There has been an increased interest in the literature on understanding the role of surgery for DLS on functional outcomes with respect to focal and global sagittal spinal alignment. However, a number of conflicting results in the literature muddy the signal of alignment effect and importance from DLS surgery.
What is the implication, and what should change now?
• Future investigational emphasis on longitudinally followed large prospective cohort or multi-centre randomized controlled trials should be prioritized.
Introduction
Degenerative lumbar spondylolisthesis (DLS) is a frequently encountered clinical pathology for adult spine surgeons (1). While the mechanism of this unique degenerative process is not fully understood, DLS primarily leads to central stenosis with an anterolisthesis of the affected vertebral body on the immediately caudal vertebrae (2). As a result of this process, patients commonly experience neurogenic claudication and may also suffer from increased back pain and radiculopathy (3,4). The benefit of surgical intervention over conservative treatment for DLS patients with neurologic symptoms is well-established (1,3,5). Treatment options centre on the goal of achieving neurologic decompression; however, the optimal treatment for this patient population remains unclear. Frequently interventions are coupled with instrumented fusions, most typically with interbody device use despite a lack of demonstrated efficacy over decompression alone (4,6,7).
Patients with DLS tend to prefer a forward flexed posture to increase intracanal space and minimize claudication symptoms while ambulating (8). The result of this postural accommodation leads to an energy-inefficient posture, which can lead to worsened health related quality of life (HRQOL) (9). To compensate for sagittal spinal imbalance, individuals with DLS tend to have increased pelvic tilt (PT), sacral slope (SS) and lumbar lordosis (LL) compared to healthy individuals in addition to patients with lumbar spinal stenosis without anterolisthesis (10-12). The inherent increased retroversion of the pelvis is the protective mechanism for maintaining sagittal balance in DLS (13). Unfortunately, PT has a finite accommodation that can occur before segmental and global sagittal spinal imbalance occurs. When sagittal imbalance occurs in DLS patients, there is a corresponding increase in the sagittal vertical axis (SVA) and a reduction in LL (14).
Appropriately addressing and correcting spinal sagittal imbalance at the time of surgery has been shown to improve HRQOLs and degree of disability in the adult spinal deformity literature (15). Patients with DLS who have a worse sagittal spinal alignment postoperatively also report greater disability and poorer HRQOL (3). Unsurprisingly, there has been an increased interest in the literature on understanding the role of surgery for DLS on functional outcomes with respect to focal and global sagittal spinal alignment (16).
It is currently unclear what breadth of available evidence exists on regional and global sagittal alignment in DLS surgery. Thus, our objective was to conduct a scoping review to map and synthesize the DLS surgical literature regarding the current radiographic assessment of alignment both pre and postoperatively. We sought to identify critical gaps in current knowledge and to provide insight about directions for future research. We present this article in accordance with the PRISMA-ScR reporting checklist (17) (available at https://jss.amegroups.com/article/view/10.21037/jss-23-26/rc).
Methods
Eligibility criteria
To be eligible for inclusion in this scoping review, investigations had to be peer-reviewed, primary studies, with English-language full text available from January 1971 to January 2023. Studies needed to examine radiographic parameters related to patients undergoing surgery of any type or indication for DLS and involve human subjects only, with greater than five patients included. Included studies did not have to primarily assess radiographic parameters nor sagittal spinal balance. However, in such instances, secondary outcomes had to include at least one time-point analysis of a radiographic parameter either preoperatively or postoperatively related to DLS surgery. Studies reporting outcomes of lumbar spinal stenosis without spondylolisthesis, low-grade spondylolisthesis without a breakdown of isthmic or DLS patient data were excluded. Any study examining functional outcomes only or fusion rates of a specific surgical technique without any measured radiographic alignment parameter were excluded.
Information sources and search
To identify relevant studies to our review, we performed a comprehensive search in the MEDLINE, EMBASE and Cochrane databases from January 1971 to January 2023. MeSH and EMTREE headings and subheadings were used to query the databases for appropriate studies for inclusion after agreement upon the highest yield search strategy by the review team. The search terms used were: “spondylolisthesis or degenerative spondylolisthesis or lumbar degenerative spondylolisthesis or spondylolistheses AND surgery or surgical procedure or surgical procedures or decompression or fusion or posterolateral fusion or interbody fusion or interbody device or interbody cage AND radiograph or radiographic parameter or spinopelvic balance or spinopelvic alignment or sagittal balance or sagittal alignment or foraminal height or disc angle or lordosis or segmental lordosis or global lordosis or segmental lumbar lordosis or global lumbar lordosis.”
Selection of sources of evidence
Title and abstract screening was performed in duplicate for the first 50 studies with review by three screeners (PT, MM, CO) to standardize and amend the screening process. Discrepancies and disagreements in the screening process were resolved via discussion and consensus upon inclusion and exclusion. Inter-observer agreement for assessment by the reviewers was calculated via Cohen’s kappa coefficient of agreement (17). Full text screening was performed through an agreed upon data extraction method that was determined ad hoc by the review team to assess the salient features of our included studies.
Data charting process, data items and synthesis of results
A data charting form was developed prior to beginning data extraction, with agreed upon variables to extract from included studies. We abstracted data on study characteristics such as date of publication, origin of investigation, type of study and the level of evidence. Level of evidence hierarchy determination of study bias was performed according to Burns et al. to stratify included studies from level one to level four (higher risk of bias) (18). Additionally, we assessed the primary objective of the investigation, surgical procedure type(s), the number of patients, average age and follow-up length. We also extracted the type of radiographic parameter(s) measured and if these were compared preoperatively to postoperative values and/or to a comparative group. Furthermore, we assessed any functional and/or health related quality of life outcomes examined among the studies. We grouped the studies by their primary investigational objective (radiographic alignment; functional outcome/radiographic alignment secondary; adjacent segment disease; new device/technique; adequacy of surgery; classification development).
Results
Literature search results and selection
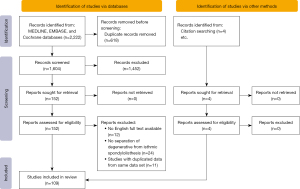
From our initial search, 2,222 studies were returned for review (Figure 1). After removal of 618 duplicate studies, 1,604 titles and abstracts were available for screening. Substantial agreement was found between the two screeners who conducted duplicate screening of the first 50 studies (Cohen’s Kappa coefficient, 0.7). Ultimately, full text screening of 152 studies identified 105 studies for inclusion with an additional four studies identified via included full text study reference lists, for a total of 109 included studies.
Study characteristics
The included studies contained 10,730 patients with an average age of 63.0 years old at the time of surgery. Average follow-up was performed 35.1 months postoperatively. Analysis of the included studies by year of publication demonstrated a strong increasing prevalence of recent investigations examining radiographic alignment with surgery in DLS (Figure 2) (19-22). The last decade [2013–2023] represented 93 (85%) of all included studies.
Included studies were largely retrospective cohorts 70 (64%) or case series 22 (20%) (Figure 3). Overall, the level of evidence among the included studies was low, with 74 (68%) of studies graded level three evidence and an additional 25 (23%) of included studies comprising level four evidence. Only two investigations (1.8%) provided level one evidence (23,24). There was a predominance of publications from Asia 65 (60%), North America 21 (19%) and Europe 20 (18%) (Figure 4).

Primary objective of included investigations
There was wide variability among included studies with respect to primary objectives of investigation (Figure 5). Forty (37%) studies primarily assessed sagittal spinal alignment in patients undergoing DLS surgery. A similar proportion, 41 (38%) studies, primarily sought to assess the functional outcomes of DLS surgery with a secondary objective of sagittal spinal alignment outcomes and/or correlation to functional outcomes. There were also 15 (14%) studies that examined either new surgical techniques or new devices in DLS surgery and their role in sagittal alignment changes.
Primary procedure types and comparative analysis among included studies
The most frequently investigated primary procedure types were posterior lumbar interbody fusion (PLIF) and transforaminal lumbar interbody fusion (TLIF), with 71 (65%) of studies reporting results of PLIF/TLIF. Fourteen studies (13%) assessed lateral lumbar interbody fusion (LLIF), extreme LIF (XLIF) or oblique LIF (OLIF), with 12 (11%) of studies assessing posterolateral fusion (PLF). Only 5 (4.6%) studies primarily assessed decompression alone with 3 (2.8%) reporting on tension band device use, 2 (1.8%) studies examining anterior lumbar interbody fusion (ALIF). Finally, 1 (0.9%) investigation assessed lumbar disc replacement, with an additional investigation combining reports of ALIF/PLIF/PLF without stratification by procedure type. Of all studies included, 29 (27%) reported on the use of minimally invasive techniques to include endoscopic/microendoscopic techniques, percutaneous pedicle screw fixation, and minimally invasive interbody fusions from a variety of approaches.
A minority of investigations [47 (43%) studies] did not report a comparative arm of either differing patient types compared to each other with the same surgical techniques, nor a comparison of two different surgical techniques and their corresponding radiographic and/or functional results. Of the studies that did report a comparative arm [62 (57%) studies], the greatest number of investigations [29/62 (47%) studies] compared PLIF/TLIF to PLIF/TLIF (Figure 6). There was an additionally higher emphasis in the included investigations on comparing PLIF/TLIF to PLF, [13/62 (21%) studies] and PLIF/TLIF to LLIF [9/62 (15%) studies].

Radiographic measures reported
There was a marked degree of variation among the studies with regards to which radiographic parameters were reported (Figure 7). One hundred (92%) studies compared the same preoperative to postoperative measurements of their patient cohorts. Of the 52 studies which did not report a comparative arm, 48/52 (92%) assessed the radiographic parameters preoperatively and postoperatively between groups. A common theme among the reporting of radiographic parameters in the included investigations was the assessment of the magnitude and/or maintenance of a radiographic change postoperatively, with 92 (84.4%) studies reporting these findings.
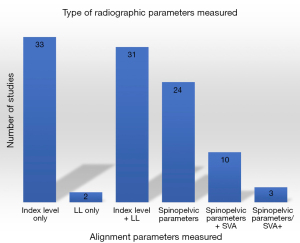
The majority of studies focused on index DLS level [33 (30%) studies] or lumbar spine radiographic imaging [33 (30%) studies] only. Thirty-seven (34%) studies reported spinopelvic parameters inclusive of PI, PT and SS, with only 13 (12%) of all included studies assessing 36-inch standing lateral radiographs and associated overall alignment.
Patient rated functional outcomes reported
A total of 87 (80%) studies reported at least one functional outcome in addition to radiographic measurements (Figure 8). The most frequent patient-reported outcome measure (PROM) was the Oswestry Disability Index (ODI), with 62 (71%) of all investigations reporting PROMs utilizing the ODI. Similarly, the Visual Analog Scale [VAS, 48 (55%) studies] and the Japanese Orthopaedic Association (JOA) back pain score [17 (20%) studies] were heavily emphasized in the PROMs reported. Notably, of the 87 studies reporting patient reported functional outcomes, only 18 analyzed these in the context of overall sagittal spinal alignment.

Discussion
In this scoping review, we identified 109 primary studies addressing sagittal radiographic parameters in DLS surgery. All studies were published between 1990 and January 2023 and the number of publications increased with time demonstrating an increasing trend of interest in the importance of sagittal spinal balance among patients undergoing DLS surgery. The majority of investigations are of level three or four evidence, primarily being published from Asia. Predominantly, retrospective cohort studies and case series dominate the literature included in this scoping review. Among our included studies, we were able to map the primary objective of each investigation in addition to the types of radiographic parameters most frequently being reported. From this synthesis, we have identified significant heterogeneity among the sagittal spinal alignment parameters being reported in these investigations. Largely our included studies focused on segmental and regional sagittal alignment parameters, with fewer studies pursuing whole spine sagittal alignment measurements. The current variability of reporting among our included studies limit the ability to meaningfully synthesize and amplify the potential effect of these smaller investigations.
While the demonstrated functional benefits of surgery for DLS have been definitively established, it has not been established what radiographic alignment parameters both preoperatively and postoperatively are most important for DLS patients. The important sagittal spinal alignment parameters demonstrated in the adult spinal deformity literature have widely permeated to degenerative lumbar spine and DLS investigations. It is unclear which surgical intervention in DLS can most affect regional and global sagittal alignment. Furthermore, different investigations outline differing effects of decompression, posterolateral fusion and interbody fusion based techniques (23,25).
Varied reports exist in the literature surrounding the regional and global sagittal alignment changes that can occur with single-level DLS surgery and importantly how this relates to functional outcomes. It has been shown that patients with greater SVA postoperatively suffer worsened functional outcome improvements than individuals with an SVA under five centimetres (3). Similarly, a PI-LL mismatch after TLIF for DLS is associated with worsened functional outcomes (26). While not borne out in the postoperative literature, there does appear to be unique patients within the DLS population who suffer from sagittal imbalance versus those who have DLS but no radiographic imbalance and these patients likely need to be treated differently (27). Kobayashi et al. have attempted to demonstrate that distinct presenting sagittal spinal alignment patterns exist among DLS patients, normal SVA <40 mm, high SVA >95 mm and associated differences in PI (28).
Unfortunately, as demonstrated, small cohort studies, largely dominate the available literature on this topic. Small scale cohort studies have been shown to exaggerate or mislead with results (28). There are a corresponding number of conflicting results which muddy the signal of alignment effect and importance from DLS surgery. Attempts at systematic reviews and meta-analyses in the DLS population with respect to radiographic alignment outcomes have struggled to achieve meaningful effect given heterogeneity within the available literature and have focused on only a limited number of DLS surgical techniques (16,29). As such, it is currently unclear what degree of sagittal balance restoration if any, correlates to improved functional outcomes in patients undergoing DLS surgery. Furthermore, Rhee et al. have demonstrated that both those patients deemed to be conventionally sagitally balanced and those determined to be imbalanced postoperatively have not been shown to have meaningful clinical functional differences in outcome (16). With existing clinical equipoise surrounding the most efficacious surgical treatment option for the DLS population it is important to identify which patients will most benefit from more invasive, expensive and higher risk surgical interventions.
Limitations
Our scoping review has several limitations. Firstly, it is subject to limitations associated with this specific study methodology in which the goal is to map the current body of literature. Secondly, we were unable to retrieve 12 non-English studies to assess in full text. This potentially limits some of the mapping of the available evidence on our topic and may have produced an underestimation of the contributions of investigations from Europe and Asia (30). However, large scale investigations such as multi-centre randomized controlled trials and high-impact prospective cohorts most commonly achieve publication in high-impact English language journals, which should help to minimize this limitation (30). Additionally, we intentionally excluded some studies which reported including patients with DLS when their results sections did not stratify the DLS patient outcomes from the isthmic or “low grade spondylolisthesis” or lumbar stenosis populations.
Conclusions
There is an increasing prevalence of studies investigating sagittal spinal alignment parameters in DLS surgery. The quality of the currently available literature on this topic is of overall low evidence and largely retrospective in nature. There is limited analysis of global sagittal spinal alignment in DLS. Future investigational emphasis on longitudinally followed large prospective cohort or multi-centre randomized controlled trials should be prioritized. Attempts at standardizing the radiographic and functional outcome reporting techniques across multi-centre investigations and prospective cohorts will allow for more robust, reproducible analyses of significance to be conducted on DLS patients.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA-ScR reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-23-26/rc
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-23-26/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-23-26/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Urquhart JC, Alnaghmoosh N, Gurr KR, et al. Posterolateral Versus Posterior Interbody Fusion in Lumbar Degenerative Spondylolisthesis. Clin Spine Surg 2018;31:E446-52.
- Cushnie D, Johnstone R, Urquhart JC, et al. Quality of Life and Slip Progression in Degenerative Spondylolisthesis Treated Nonoperatively. Spine (Phila Pa 1976) 2018;43:E574-9.
- Radovanovic I, Urquhart JC, Ganapathy V, et al. Influence of postoperative sagittal balance and spinopelvic parameters on the outcome of patients surgically treated for degenerative lumbar spondylolisthesis. J Neurosurg Spine 2017;26:448-53. [Crossref] [PubMed]
- Schneider N, Fisher C, Glennie A, et al. Lumbar degenerative spondylolisthesis: factors associated with the decision to fuse. Spine J 2021;21:821-8. [Crossref] [PubMed]
- Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical Compared with Nonoperative Treatment for Lumbar Degenerative Spondylolisthesis: Four-Year Results in the Spine Patient Outcomes Research Trial (SPORT) Randomized and Observational Cohorts. The Journal of Bone & Joint Surgery 2009;91:1295-304. [Crossref] [PubMed]
- Maher A. Understanding surgeon decision-making and current surgical practice regarding the DSIC scheme and DLS treatment: a CSORN study. Spine J 2019;19:S14-5.
- Kepler CK, Vaccaro AR, Hilibrand AS, et al. National trends in the use of fusion techniques to treat degenerative spondylolisthesis. Spine (Phila Pa 1976) 2014;39:1584-9. [Crossref] [PubMed]
- Buckland AJ, Vira S, Oren JH, et al. When is compensation for lumbar spinal stenosis a clinical sagittal plane deformity? Spine J 2016;16:971-81.
- Mehta VA, Amin A, Omeis I, et al. Implications of spinopelvic alignment for the spine surgeon. Neurosurgery 2015;76:S42-56; discussion S56. [Crossref] [PubMed]
- Nakamae T, Nakanishi K, Kamei N, et al. The correlation between sagittal spinopelvic alignment and degree of lumbar degenerative spondylolisthesis. J Orthop Sci 2019;24:969-73. [Crossref] [PubMed]
- Yijian Z, Hao L, Huilin Y, et al. Comparison of posterolateral fusion and posterior lumbar interbody fusion for treatment of degenerative spondylolisthesis: Analysis of spino-pelvic sagittal balance and postoperative chronic low back pain. Clin Neurol Neurosurg 2018;171:1-5. [Crossref] [PubMed]
- Funao H, Tsuji T, Hosogane N, et al. Comparative study of spinopelvic sagittal alignment between patients with and without degenerative spondylolisthesis. Eur Spine J 2012;21:2181-7. [Crossref] [PubMed]
- Liu H, Li S, Zheng Z, et al. Pelvic retroversion is the key protective mechanism of L4-5 degenerative spondylolisthesis. Eur Spine J 2015;24:1204-11. [Crossref] [PubMed]
- Lim JK, Kim SM. Comparison of Sagittal Spinopelvic Alignment between Lumbar Degenerative Spondylolisthesis and Degenerative Spinal Stenosis. J Korean Neurosurg Soc 2014;55:331-6. [Crossref] [PubMed]
- Sheikh Alshabab B, Gupta MC, Lafage R, et al. Does Achieving Global Spinal Alignment Lead to Higher Patient Satisfaction and Lower Disability in Adult Spinal Deformity? Spine (Phila Pa 1976) 2021;46:1105-10. [Crossref] [PubMed]
- Rhee C, Visintini S, Dunning CE, et al. Does restoration of focal lumbar lordosis for single level degenerative spondylolisthesis result in better patient-reported clinical outcomes? A systematic literature review. J Clin Neurosci 2017;44:95-100. [Crossref] [PubMed]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-74.
- Burns PB, Rohrich RJ, Chung KC. The levels of evidence and their role in evidence-based medicine. Plast Reconstr Surg 2011;128:305-10. [Crossref] [PubMed]
- Fujiya M, Saita M, Kaneda K, et al. Clinical study on stability of combined distraction and compression rod instrumentation with posterolateral fusion for unstable degenerative spondylolisthesis. Spine (Phila Pa 1976) 1990;15:1216-22. [Crossref] [PubMed]
- Kimura I, Shingu H, Murata M, et al. Lumbar posterolateral fusion alone or with transpedicular instrumentation in L4--L5 degenerative spondylolisthesis. J Spinal Disord 2001;14:301-10. [Crossref] [PubMed]
- Moher D, Pham B, Lawson ML, et al. The inclusion of reports of randomised trials published in languages other than English in systematic reviews. Health Technol Assess 2003;7:1-90. [Crossref] [PubMed]
- Mohanty S, Barchick S, Kadiyala M, et al. Should patients with lumbar stenosis and grade I spondylolisthesis be treated differently based on spinopelvic alignment? A retrospective, two-year, propensity matched, comparison of patient-reported outcome measures and clinical outcomes from multiple sites within a single health system. Spine J 2023;23:92-104. [Crossref] [PubMed]
- Kawakami M, Tamaki T, Ando M, et al. Lumbar sagittal balance influences the clinical outcome after decompression and posterolateral spinal fusion for degenerative lumbar spondylolisthesis. Spine (Phila Pa 1976) 2002;27:59-64. [Crossref] [PubMed]
- Challier V, Boissiere L, Obeid I, et al. One-Level Lumbar Degenerative Spondylolisthesis and Posterior Approach: Is Transforaminal Lateral Interbody Fusion Mandatory?: A Randomized Controlled Trial With 2-Year Follow-Up. Spine (Phila Pa 1976) 2017;42:531-9. [Crossref] [PubMed]
- Lian XF, Hou TS, Xu JG, et al. Posterior lumbar interbody fusion for aged patients with degenerative spondylolisthesis: is intentional surgical reduction essential? Spine J 2013;13:1183-9.
- Gille O, Challier V, Parent H, et al. Degenerative lumbar spondylolisthesis: cohort of 670 patients, and proposal of a new classification. Orthop Traumatol Surg Res 2014;100:S311-5. [Crossref] [PubMed]
- Aoki Y, Nakajima A, Takahashi H, et al. Influence of pelvic incidence-lumbar lordosis mismatch on surgical outcomes of short-segment transforaminal lumbar interbody fusion. BMC Musculoskelet Disord 2015;16:213. [Crossref] [PubMed]
- Kobayashi H, Endo K, Sawaji Y, et al. Global sagittal spinal alignment in patients with degenerative low-grade lumbar spondylolisthesis. J Orthop Surg (Hong Kong) 2019;27:2309499019885190. [Crossref] [PubMed]
- Bhandari M, Morshed S, Tornetta P, et al. Design, Conduct, and Interpretation of Nonrandomized Orthopaedic Studies: A Practical Approach: (All) Evidence Matters. J Bone Joint Surg 2009;91:1. [Crossref] [PubMed]
- Cho JY, Goh TS, Son SM, et al. Comparison of Anterior Approach and Posterior Approach to Instrumented Interbody Fusion for Spondylolisthesis: A Meta-analysis. World Neurosurg 2019;129:e286-93.





