
Prone position lateral interbody fusion—a narrative review
Introduction
Background
Degenerative disc disease, facet disease and lumbar stenosis are common causes of disability in an aging population. Symptoms can include axial back pain, radiculopathy and/or claudication leading to reduced mobility and subsequent poor quality of life (1). Surgical treatment options for these symptoms revolve around decompression of the compressed neural elements. Fusion would also be done if needed for any underlying or resultant instability (2). Interbody fusion is one such method that has the power to both indirectly decompress as well as fuse the pathologic levels undergoing instrumentation while also restoring regional lordosis and correcting deformity (1,2). Historically, interbody instrumentation has consisted of posterior lumbar interbody fusion and trans foraminal interbody fusion, but these procedures are challenging due to the need for thecal sac and nerve root retraction, limiting the size of the interbody device, as well as being associated with increased blood loss and disruption of the paraspinal musculature. Because of these limitations, multiple techniques for interbody fusion have been developed including anterior lumbar interbody fusion (3), oblique lateral interbody fusion (OLIF), and lateral lumbar interbody fusion (LLIF) (1,4). These techniques allow for improved access to the lumbar disc space which allows for the implantation of a larger interbody implant allowing for more powerful deformity correction and lower blood loss when compared to posterior procedures. Lateral access lumbar interbody fusion is an increasingly popular procedure that allows for anterior column support through discectomy, endplate preparation, and interbody insertion. As initially performed, the lateral approach required initial lateral decubitus position with the patient then repositioned to the prone position for placement of open or percutaneous pedicle screws (5). Recently, single position LLIF techniques have been described to decrease both operative and anesthesia time as well as decrease costs from time that is spent repositioning the patient in the operating room. The prone lateral interbody fusion technique is one such modification that allows the patient to be positioned prone while the LLIF is performed with posterior pedicle screw fixation without repositioning (4-6).
Rationale and knowledge gap
This new iteration of lateral access surgery comes with several advantages, disadvantages, and unique considerations. Beginning with open posterior procedures for lumbar discectomy and interbody fusion there has been progressive development of surgical techniques towards better anterior column access and muscle sparing less invasive surgery. Open posterior surgery progressed through minimally invasive tubular/endoscopic posterior surgery, then to open lateral access surgery, and minimally invasive lateral surgery. We now examine prone position LLIF and its comparison to other surgical techniques, in particular lateral decubitus position lateral lumbar interbody fusion.
Objective
This narrative review seeks to summarize and synthesize the recent developments in the literature on advantages, disadvantages, and unique features of the prone position lateral access lumbar interbody fusion. We present this article in accordance with the Narrative Review reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-23-34/rc).
Methods
We performed a narrative review of articles published up to 01 November 2022 through a PubMed search. The search terms “prone lateral spine surgery” and “lateral approach spine surgery” AND “prone position” were used, as summarized in Table 1. Articles not available in English were excluded. The search result abstracts were independently reviewed by 2 authors and 28 full text articles were reviewed. The PRISMA flow diagram is shown in Figure 1. Both reviewing authors were orthopedic surgery residents. The reviewed articles are listed in Table 2.
Table 1
| Items | Specification |
|---|---|
| Date of search | Nov 1, 2022 |
| Databases and other sources searched | PubMed |
| Search terms used | Lateral approach spine surgery, prone lateral spine surgery, prone position |
| Timeframe | All studies published up to Nov 1, 2022 |
| Inclusion criteria | English language, specific to prone lateral interbody fusion |
| Selection process | Selection process independently conducted by 2 orthopedic surgery chief residents |
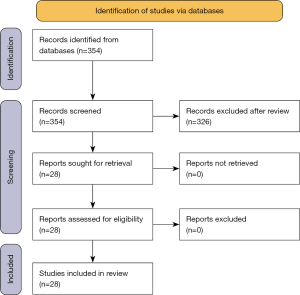
Table 2
| Authors | Title | Journal |
|---|---|---|
| Farber et al. (7) | Single-position prone lateral transpsoas approach: early experience and outcomes | J Neurosurg Spine |
| Guiroy et al. (8) | Single-Position Surgery versus Lateral-Then-Prone-Position Circumferential Lumbar Interbody Fusion: A Systematic Literature Review | World Neurosurg |
| Lamartina et al. (9) | Prone single-position extreme lateral interbody fusion (Pro-XLIF): preliminary results | Eur Spine J |
| Gandhi et al. (10) | Prone transpsoas lumbar corpectomy: simultaneous posterior and lateral lumbar access for difficult clinical senarios | J Neurosurg Spine |
| Hoffman et al. (11) | Three-dimensional Navigation-guided, Prone, Single-position, Lateral Lumbar Interbody Fusion Technique | J Vis Exp |
| Walker et al. (12) | Single-Position Prone Lateral Interbody Fusion Improves Segmental Lordosis in Lumbar Spondylolisthesis | World Neurosurg |
| Alluri et al. (13) | Location of the Femoral Nerve in the Lateral Decubitus Versus Prone Position | Global Spine J |
| Pimenta et al. (14) | Single-Position Prone Transpsoas Lateral Interbody Fusion Including L4L5: Early Postoperative Outcomes | World Neurosurg |
| Smith et al. (15) | Effects of Surgical Positioning on L4-L5 Accessibility and Lumbar Lordosis in Lateral Transpsoas Lumbar Interbody Fusion: A Comparison of Prone and Lateral Decubitus in Asymptomatic Adults | World Neurosurg |
| Soliman et al. (16) | Comparison of Prone Transpsoas and Standard Lateral Lumbar Interbody Fusion Surgery for Degenerative Lumbar Spine Disease: A Retrospective Radiographic Propensity Score-Matched Analysis | World Neurosurg |
| Stone et al. (17) | Prone-lateral access to the lumbar spine: single-level corpectomy with approach discussion | Neurosurg Focus Video |
| Godzik et al. (18) | Single-position prone lateral approach: cadaveric feasibility study and early clinical experience | Neurosurg Focus |
| North et al. (19) | Navigation and Robotic-Assisted Single-Position Prone Lateral Lumbar Interbody Fusion: Technique, Feasibility, Safety, and Case Series | World Neurosurg |
| Martirosyan et al. (5) | Prone Lateral Lumbar Interbody Fusion: Case Report and Technical Note | World Neurosurg |
| Amaral et al. (20) | The Effect of Patient Position on Psoas Morphology and in Lumbar Lordosis | World Neurosurg |
| Pimenta et al. (6) | Prone Transpsoas Technique for Simultaneous Single-Position Access to the Anterior and Posterior Lumbar Spine | Oper Neurosurg (Hagerstown) |
| Smith et al. (21) | Initial multi-centre clinical experience with prone transpsoas lateral interbody fusion: Feasibility, perioperative outcomes, and lessons learned | N Am Spine Soc J |
| Salmons et al. (22) | Prone Versus Lateral Decubitus Positioning for Direct Lateral Interbody Fusion | Clin Spine Surg |
| Gandhi et al. (23) | Anatomical positional changes in the lateral lumbar interbody fusion | Eur Spine J |
| Courville et al. (24) | Effects of thigh extension on the position of the femoral nerve: application to prone lateral transpsoas approaches to the lumbar spine | Neurosurg Rev |
| Soliman et al. (25) | Prone Transpsoas Lateral Lumbar Interbody Fusion for Degenerative Lumbar Spine Disease: Case Series With an Operative Video Using Fluoroscopy-Based Instrument Tracking Guidance | Oper Neurosurg (Hagerstown) |
| Pimenta et al. (26) | The prone transpsoas technique: preliminary radiographic results of a multicenter experience | Eur Spine J |
| Buckland et al. (27) | Single position circumferential fusion improves operative efficiency, reduces complications and length of stay compared with traditional circumferential fusion |
Spine J |
| Goldberg et al. (28) | Single-Position Fluoroscopy-Guided Lateral Lumbar Interbody Fusion With Intraoperative Computed Tomography-Navigated Posterior Pedicle Screw Fixation: Technical Report and Literature Review | Int J Spine Surg |
| Shahrestani et al. (29) | A case report of robotic-guided prone transpsoas lumbar fusion in a patient with lumbar pseudarthrosis, adjacent segment disease, and degenerative scoliosis | Int J Surg Case Rep |
| Hiyama et al. (30) | Facet joint violation after single-position versus dual-position lateral interbody fusion and percutaneous pedicle screw fixation: A comparison of two techniques | J Clin Neurosci |
| Wang et al. (31) | Single-position prone transpsoas fusion for the treatment of lumbar adjacent segment disease: early experience of twenty-four cases across three tertiary medical centers | Eur Spine J |
| Hiyama et al. (32) | Comparison of radiological changes after single-position versus dual-position for lateral interbody fusion and pedicle screw fixation | BMC Musculoskelet Disord |
| Dodo et al. (33) | The anatomical positioning change of retroperitoneal organs in prone and lateral position: an assessment for single-prone position lateral lumbar surgery | Eur Spine J |
| Farber et al. (34) | Complications associated with single-position prone lateral lumbar interbody fusion: a systematic review and pooled analysis | J Neurosurg Spine |
Results and discussion
Lateral interbody fusion has several advantages relative to anterior and posterior approaches for interbody placement for the appropriate indications. The anterior approach for interbody placement in the thoracolumbar spine provides outstanding access for discectomy, endplate preparation and interbody placement, but typically requires an access surgeon and puts the abdominal great vessels at risk during access to the lumbar spine. There are several advantages of lateral interbody fusion surgery relative to anterior interbody fusion; including shorter operative time, lack of a need for an approach surgeon, and decreased manipulation and risk of injury to the great vessels (9,32,35). Posterior approach or translaminar interbody fusion is limited to a small surgical field to access the intervertebral disc resulting in limited interbody cage size and relatively less ability to restore regional lordosis. An interbody device placed through posterior approach typically rests on cancellous end plate, instead of the cortical rim, leading to subsequent subsidence and loss of regional correction (16,36,37). This technique also requires retraction of the thecal sac and nerve roots with accompanying greater risk of dural tear and CSF leak (1,4). Lateral interbody fusion also provides the unique ability to insert a long interbody device which rests on the cortical rim of both the endplate above and below the disk space. This helps to prevent subsidence and maintain the regional lordosis achieved during surgery (16,36,37). When lateral lumbar interbody fusion is performed with the anterior longitudinal ligament release, it provides the opportunity to correct sagittal plane deformity with hyper lordotic interbody device, without the direct access to the great vessels at front (38). It should be noted that lateral interbody fusion does still retain the risk of neurovascular injury, particularly to the lumbar plexus or femoral nerve and the great vessels largely from retraction of these structures to obtain access to the lateral aspect of the spine (39). There has been evolution in lateral surgery from “direct look” visual evaluation of the lumbar plexus to the use of directional nerve stimulation. Proper utilization of the directional nerve stimulation with trigger electromyography (EMG) helps to find a safe corridor to the disk, protecting the lumbar plexus. More recently, somatosensory evoked potential monitoring is also utilized during LLIF which provides warning of nerve injury from prolonged retraction (40,41).
There are many advantages of lateral interbody fusion performed in the prone position in comparison to the same procedure performed in the lateral decubitus position. These advantages include ease of placing pedicle screws in the prone position, increased ability to obtain segmental lordosis in the prone position, as well as relative position of the psoas muscle belly, lumbar plexus, peritoneal contents, and great vessels. There are additional advantages that have been suggested or anecdotally alluded to in the literature, but for which empirical evidence is currently lacking.
Advantages
Ease of placing pedicle screws
Lateral interbody fusion is typically augmented with posterior pedicle screw instrumentation to stabilize the fusion construct. Other options for supplementary stabilization include lateral plate placement or a stand alone cage with integrated screw fixation, however, the literature suggests that most surgeons performing lateral interbody fusions utilize a minimally invasive technique coupled with open or percutaneous pedicle screw fixation (42). There are multiple studies describing the placement of pedicle screws in the lateral position (43,44). While technically feasible, most surgeons have far more experience with placing pedicle screws in the prone position and prone lateral interbody fusion affords the ability to easily place pedicle screws in the prone position (18). The placement of pedicle screws in the lateral position can increase the risk of contamination to the sterile field particularly while placing the down side pedicle screws due to the unergonomic angle. In a study by Ziino et al., comparing single position LLIF in the lateral position with pedicle screw placement with dual position LLIF—LLIF in the lateral position followed by prone pedicle screw placement, two patients in the single position lateral group had to return to the operating room for removal of symptomatic pedicle screws. No patients in the group with pedicle screws placed in the prone position had to return to the OR (44).
Simultaneous posterior access
Prone position for the placement of lateral interbody cages allows for access to the posterior elements of the spine. This facilitates the completion of additional procedures while performing a lateral interbody fusion such as direct posterior decompression, osteotomy of the posterior elements, and posterior instrumentation or revision/removal of prior posterior instrumentation (21). This ability to simultaneously access the posterior elements allows for significant versatility of the lateral interbody procedure while maintaining the benefits of lateral interbody versus posterior interbody techniques such as transforaminal lumbar interbody fusion (45). An example case demonstrating the advantages of simultaneous lateral and posterior access is a 55-year-old patient with a history of back pain and neurogenic claudication with grade 2 degenerative spondylolisthesis at L4–L5. Anteroposterior and lateral radiographs of this patient are seen in Figure 2. This patient underwent prone lateral indirect decompression with lateral lumbar interbody cage placement with an open facetectomy and pedicle screw placement L4–L5. Post operative radiographs of this case are seen in Figure 3. It is possible to place pedicle screws while the patient is placed in lateral position for the lumbar interbody fusion, however it is technically difficult to perform facetectomies in the lateral position. Simultaneous posterior access also decreases the operative time of the procedure by allowing for placement of posterior pedicle screws without having to re-position and re-drape the patient. Guiroy et al. determined through a literature review that prone position LLIF had a significantly shorter operative time than dual position LLIF at 103 vs. 306 minutes, P=0.001 (8). A potential complication of lateral interbody fusion is the inability to place a lateral interbody cage because of the lack of a safe corridor through the lumbar plexus or technical challenges accessing the disk space due to a high iliac crest. In this situation, to complete the procedure, a posterior decompression and fusion with a transforaminal or posterior interbody cage is often performed as a salvage option. Prone positioning for lateral interbody placement allows for this reserve option without patient repositioning.


Regional lumbar lordosis and global sagittal alignment
In achieving segmental lordosis, lateral interbody fusion in the prone position has the advantage of achieving increased segmental lordosis relative to posterior interbody fusion, which is also done in the prone position (16,36,46). In comparison to lateral interbody fusion in the lateral decubitus position, prone position allows for significantly more segmental lordosis than lateral decubitus position. Smith et al., studied the effect of different positions including prone hip flexed, prone hips neutral, prone in a coronal bend positioner with hips neutral, and prone in a coronal bend positioner with hips extended, for lateral interbody fusion in healthy adult volunteers on segmental lordosis. They found that all prone positions had a significantly greater degree of segmental lordosis than lateral decubitus P<0.001. The average segmental lordosis in the lateral decubitus position was 11.2 degrees at L4–L5 and 53.5 degrees through L1–S1. The greatest average segmental lordosis in the prone position was prone extended with 12 degrees at L4–L5 and 62.5 degrees through L1–S1 (15). MRI studies showed up to a 3 times greater increase in lumbar lordosis in patients voluntarily undergoing MRI in the prone position relative to the same patients in the lateral decubitus position (20,23). A study by Amaral et al., examined patients by MRI to evaluate lumbar lordosis in the prone and lateral decubitus position. This study found that there was a significantly greater degree of lumbar lordosis in the prone position than the lateral decubitus position in overall lumbar lordosis, 57.6 vs. 46.5 degrees, P<0.001, as well as in distal lumbar lordosis defined as L4–S1, 40.4 vs. 36.9 degrees, P<0.01 (20).
A study examining pre-operative vs. post-operative change in segmental lordosis in patients who underwent lateral position lateral interbody fusion followed by either pedicle screw fixation in the prone position or the lateral decubitus position showed no significant difference in overall segmental lordosis (32,44). When this viewed along with the MRI studies showing significant increases in lumbar lordosis in the prone position vs. lateral decubitus position suggest that prone position for placement of the interbody cage may be integral to obtaining increased segmental lumbar lordosis.
A study by Walker et al. (12), comparing segmental lordosis between patients undergoing prone lateral interbody fusion and lateral position lateral interbody fusion followed by prone pedicle screw fixation showed a significant increase in segmental lordosis for the prone lateral group. This study showed that the prone lateral group had an increase in segmental lordosis of 5.1 vs. 2.5 degrees for the dual position lateral then prone group, P=0.02. However, this study did not show as significant difference in overall segmental lordosis at 6.3 vs. 3.1 degrees, P=0.14. There was a significantly more anterior placement of the interbody cage in the prone position vs. the lateral decubitus position, however cage position was not correlated with segmental lordosis. So, this alone cannot account for the increased segmental lordosis in the prone position group (20). Soliman et al. (16) conducted a study comparing propensity score matched patients that underwent prone position LLIF with those that underwent LLIF in the lateral decubitus position. They found that the prone group had a significant average increase in lumbar lordosis vs the lateral position group at 9.9 vs. 0.5 degrees, P=0.047. They also found that the prone group had a change in PI-LL that approached statistical significance versus the lateral position group at 15.6 vs. 3.7, P=0.05. It is important to note that the preoperative PI-LL was significantly higher for the prone group: 19.1 vs. 8.5, P=0.02, which may reveal some initial patient selection bias. Available literature suggests that the prone position lateral interbody fusion affords for greater increase in segmental lordosis and more ease in doing so relative to lateral decubitus lateral interbody fusion (21).
Position of the psoas muscle and lumbar plexus
The position and morphology of the psoas muscle can change with patient position between the prone position and the lateral decubitus position. A study by Gandhi et al. examined the MRI scans of 10 healthy volunteers in various surgical positions to evaluate the position and morphology of the psoas muscle. This study found that the psoas muscle was most anteriorly elongated in the lateral decubitus position with hips flexed at 5.82 mm, more anterior P<0.001 followed by lateral decubitus position with hips extended at 2.23 mm, P<0.001. The psoas did anteriorly elongate slightly relative to supine in the prone hips flexed position at 0.21 mm, P=0.014. There was not a statistically significant difference between the anterior elongation of the psoas in the prone hip extended position compared to the supine position (23). This suggests that the lumbar plexus contained in the psoas muscle remains relatively more posterior in the prone position relative to the lateral decubitus position, decreasing the risk of lumbar plexus injury for prone LLIF relative to LLIF in the lateral decubitus position. Most preoperative MRI are done in the supine position with pre-operative planning also being done based on anatomical structures as they appear in these images. Prone position more closely approximates the position of anatomical structures seen on supine preoperative MRI (23). If desired, an MRI for pre-operative planning could also be obtained in the prone position. A change in position of the lumbar plexus is also a potential variation of concern when performing a lateral interbody fusion, however, MRI studies in the prone and lateral decubitus position have shown that the position of the lumbar plexus remains largely unchanged relative to the vertebral body between the prone and lateral decubitus position (20).
Position of great vessels
The position of the great vessels is another consideration when considering the lateral approach in the prone position. An MRI study shows that when comparing the left lateral flexed position to the prone extended position the IVC moves medially to the left and the aorta moves laterally to the left. This study also showed that the venous structures appear to be more full and open in the lateral decubitus position than in the prone position (23). This could be a concern for increase blood loss in the prone position, though other studies have shown less blood loss or equivalent blood loss in prone lateral interbody fusion when compared to the lateral decubitus position followed by percutaneous pedicle screw fixation in the prone position (8).
Other potential advantages
There are many other advantages to prone lateral surgery suggested in the literature by surgeons performing and publishing on this topic that at this time lack empirical evidence. One of these potential advantages is that patient positioning in the prone position allows gravity to assist in the peritoneal contents falling anteriorly away from the surgical field, potentially decreasing the risk of injury to these and retroperitoneal structures such as the ascending or descending colon. A study by Dodo et al. evaluating position of retroperitoneal organs did show that these structures moved away from the operative field in the prone position, though remained close enough to be at risk of injury (33). The overall rate of retroperitoneal or peritoneal injury is low making it difficult to show the prone position to have an overall lower rate of such injury (8,34). The increased stability and thus accuracy of navigation in the prone position relative to lateral decubitus position is also suggested. It is thought that in the prone position there is less ability for rotatory and other motions that may reduce the reliability and accuracy of navigation systems (18). However, other surgeons have also suggested that there is actually less stability of the spine in the torso or patient on prone positioning frame relative to the lateral decubitus position.
Disadvantages
Exposure and retraction
There are several disadvantages to performing a lateral access interbody fusion in the lateral position relative to the lateral decubitus position. Prone positioning can make adequate exposure and retraction more challenging in obese patients with a large abdominal girth. In the lateral decubitus position gravity can assist in allowing excess soft tissue to fall away from the operative site and reduce the depth of the field (18,21). This is not the case in prone position and the resulting increase depth of the field can make this procedure more challenging. Furthermore, commercially available retractor blades are limited in the depth of retractor available (5). Longer retractor blades also can tend to flex at the deep extent of the exposure causing a smaller working field, which can further complicate the procedure (21).
Positioning
Lateral interbody fusion in the lateral position has the advantage of breaking the table to allow better lateral access to the desired intervertebral disk space. This is not easily done in the standard prone position; however, some specialized table attachments are commercially available that allow a similar feature to breaking the table in the prone position. In the standard prone position, a bolster placed against the patient may allow for a similar effect to breaking the table, however, this is not as effective as breaking the table in the lateral decubitus position. This may limit access in levels near the iliac crest or rib cage for prone lateral interbody fusion (5). Patient stability in the prone position, at least without a procedure specific table or stabilizers, is another concern. A large multi-center study reported that one of the disadvantages of the prone position relative to the lateral position was movement of the patient during the procedure with the forces applied, movement of the spine within the torso, and retractor creep with gravity. The table mounted retractor would sometimes pull away from the spine, during malleting in the procedure, allowing from soft tissue encroachment (21).
Limitations of this review
This review is limited in its scope as a narrative review of prone position lateral lumbar interbody fusion. The nature of this paper as a narrative review is a limitation as it is not as methodologically rigorous as a systematic review. Furthermore, this does not provide a rigorous statistical comparison to other surgical techniques is limited to a summary observation of the available literature.
Summary and conclusions
Prone position lateral interbody fusion is an increasingly prevalent and useful surgical technique with several advantages and disadvantages when compared to lateral interbody fusion in the lateral decubitus position. The prone lateral interbody fusion may provide the benefits of improved sagittal alignment, decreased operative times, different risk profile, and more familiar and ergonomic positioning relative to other methods for lateral interbody fusion. Disadvantages such as exposure, retraction, and visualization exist and should be further explored. There are several surgical indications and goals for which prone lateral interbody fusion may provide significant benefit when compared to other interbody fusion techniques.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Cameron Kia) for the series “Minimally Invasive Techniques in Spine Surgery and Trend Toward Ambulatory Surgery” published in Journal of Spine Surgery. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-23-34/rc
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-23-34/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-23-34/coif). The series “Minimally Invasive Techniques in Spine Surgery and Trend Toward Ambulatory Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mobbs RJ, Phan K, Malham G, et al. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg 2015;1:2-18. [Crossref] [PubMed]
- Nomura H, Yamashita A, Watanabe T, et al. Quantitative analysis of indirect decompression in extreme lateral interbody fusion and posterior spinal fusion with a percutaneous pedicle screw system for lumbar spinal stenosis. J Spine Surg 2019;5:266-72. [Crossref] [PubMed]
- Jawish R, Ghorayeb J, Khalife R. Quadruple and juxta-articular pelvic osteotomy in children using anterior approach: technique and results. J Pediatr Orthop B 2007;16:10-5. [Crossref] [PubMed]
- Mills ES, Treloar J, Idowu O, et al. Single position lumbar fusion: a systematic review and meta-analysis. Spine J 2022;22:429-43. [Crossref] [PubMed]
- Martirosyan NL, Uribe JS, Randolph BM, et al. Prone Lateral Lumbar Interbody Fusion: Case Report and Technical Note. World Neurosurg 2020;144:170-7. [Crossref] [PubMed]
- Pimenta L, Taylor WR, Stone LE, et al. Prone Transpsoas Technique for Simultaneous Single-Position Access to the Anterior and Posterior Lumbar Spine. Oper Neurosurg (Hagerstown) 2020;20:E5-E12. [Crossref] [PubMed]
- Farber SH, Naeem K, Bhargava M, et al. Single-position prone lateral transpsoas approach: early experience and outcomes. J Neurosurg Spine 2022;36:358-65. [Crossref] [PubMed]
- Guiroy A, Carazzo C, Camino-Willhuber G, et al. Single-Position Surgery versus Lateral-Then-Prone-Position Circumferential Lumbar Interbody Fusion: A Systematic Literature Review. World Neurosurg 2021;151:e379-86.
- Lamartina C, Berjano P. Prone single-position extreme lateral interbody fusion (Pro-XLIF): preliminary results. Eur Spine J 2020;29:6-13. [Crossref] [PubMed]
- Gandhi SD, Liu DS, Sheha ED, et al. Prone transpsoas lumbar corpectomy: simultaneous posterior and lateral lumbar access for difficult clinical scenarios. J Neurosurg Spine 2021;35:284-91. [Crossref] [PubMed]
- Hoffman SE, Gupta S, Huang K, et al. Three-dimensional Navigation-guided, Prone, Single-position, Lateral Lumbar Interbody Fusion Technique. J Vis Exp 2021;
- Walker CT, Farber SH, Gandhi S, et al. Single-Position Prone Lateral Interbody Fusion Improves Segmental Lordosis in Lumbar Spondylolisthesis. World Neurosurg 2021;151:e786-92.
- Alluri R, Clark N, Sheha E, et al. Location of the Femoral Nerve in the Lateral Decubitus Versus Prone Position. Global Spine J 2023;13:1765-70. [Crossref] [PubMed]
- Pimenta L, Pokorny G, Amaral R, et al. Single-Position Prone Transpsoas Lateral Interbody Fusion Including L4L5 Early Postoperative Outcomes. World Neurosurg 2021;149:e664-8.
- Smith TG, Pollina J, Joseph SA Jr, et al. Effects of Surgical Positioning on L4-L5 Accessibility and Lumbar Lordosis in Lateral Transpsoas Lumbar Interbody Fusion: A Comparison of Prone and Lateral Decubitus in Asymptomatic Adults. World Neurosurg 2021;149:e705-13.
- Soliman MAR, Aguirre AO, Ruggiero N, et al. Comparison of prone transpsoas lateral lumbar interbody fusion and transforaminal lumbar interbody fusion for degenerative lumbar spine disease: A retrospective radiographic propensity score-matched analysis. Clin Neurol Neurosurg 2022;213:107105. [Crossref] [PubMed]
- Stone LE, Diaz-Aguilar LD, Santiago-Dieppa DR, et al. Prone-lateral access to the lumbar spine: single-level corpectomy with approach discussion. Neurosurg Focus Video 2022;7:V9. [Crossref] [PubMed]
- Godzik J, Ohiorhenuan IE, Xu DS, et al. Single-position prone lateral approach: cadaveric feasibility study and early clinical experience. Neurosurg Focus 2020;49:E15. [Crossref] [PubMed]
- North RY, Strong MJ, Yee TJ, et al. Navigation and Robotic-Assisted Single-Position Prone Lateral Lumbar Interbody Fusion: Technique, Feasibility, Safety, and Case Series. World Neurosurg 2021;152:221-230.e1. [Crossref] [PubMed]
- Amaral R, Daher MT, Pratali R, et al. The Effect of Patient Position on Psoas Morphology and in Lumbar Lordosis. World Neurosurg 2021;153:e131-40.
- Smith TG, Joseph SA Jr, Ditty B, et al. Initial multi-centre clinical experience with prone transpsoas lateral interbody fusion: Feasibility, perioperative outcomes, and lessons learned. N Am Spine Soc J 2021;6:100056. [Crossref] [PubMed]
- Salmons HI, Baird MD, Dearden ME, et al. Prone Versus Lateral Decubitus Positioning for Direct Lateral Interbody Fusion. Clin Spine Surg 2022;35:351-3. [Crossref] [PubMed]
- Gandhi SV, Dugan R, Farber SH, et al. Anatomical positional changes in the lateral lumbar interbody fusion. Eur Spine J 2022;31:2220-6. [Crossref] [PubMed]
- Courville E, Ditty BJ, Maulucci CM, et al. Effects of thigh extension on the position of the femoral nerve: application to prone lateral transpsoas approaches to the lumbar spine. Neurosurg Rev 2022;45:2441-7. [Crossref] [PubMed]
- Soliman MAR, Ruggiero N, Aguirre AO, et al. Prone Transpsoas Lateral Lumbar Interbody Fusion for Degenerative Lumbar Spine Disease: Case Series With an Operative Video Using Fluoroscopy-Based Instrument Tracking Guidance. Oper Neurosurg (Hagerstown) 2022;23:382-8. [Crossref] [PubMed]
- Pimenta L, Amaral R, Taylor W, et al. The prone transpsoas technique: preliminary radiographic results of a multicenter experience. Eur Spine J 2021;30:108-13. [Crossref] [PubMed]
- Buckland AJ, Ashayeri K, Leon C, et al. Single position circumferential fusion improves operative efficiency, reduces complications and length of stay compared with traditional circumferential fusion. Spine J 2021;21:810-20. [Crossref] [PubMed]
- Goldberg JL, McGrath LB Jr, Kirnaz S, et al. Single-Position Fluoroscopy-Guided Lateral Lumbar Interbody Fusion With Intraoperative Computed Tomography-Navigated Posterior Pedicle Screw Fixation: Technical Report and Literature Review. Int J Spine Surg 2022;16:S9-S16. [Crossref] [PubMed]
- Shahrestani S, Brown NJ, Acharya N, et al. A case report of robotic-guided prone transpsoas lumbar fusion in a patient with lumbar pseudarthrosis, adjacent segment disease, and degenerative scoliosis. Int J Surg Case Rep 2022;94:106999. [Crossref] [PubMed]
- Hiyama A, Katoh H, Sakai D, et al. Facet joint violation after single-position versus dual-position lateral interbody fusion and percutaneous pedicle screw fixation: A comparison of two techniques. J Clin Neurosci 2020;78:47-52. [Crossref] [PubMed]
- Wang TY, Mehta VA, Sankey EW, et al. Single-position prone transpsoas fusion for the treatment of lumbar adjacent segment disease: early experience of twenty-four cases across three tertiary medical centers. Eur Spine J 2022;31:2255-61. [Crossref] [PubMed]
- Hiyama A, Katoh H, Sakai D, et al. Comparison of radiological changes after single- position versus dual- position for lateral interbody fusion and pedicle screw fixation. BMC Musculoskelet Disord 2019;20:601. [Crossref] [PubMed]
- Dodo Y, Okano I, Kelly NA, et al. The anatomical positioning change of retroperitoneal organs in prone and lateral position: an assessment for single-prone position lateral lumbar surgery. Eur Spine J 2023;32:2003-11. [Crossref] [PubMed]
- Farber SH, Valenzuela Cecchi B, O'Neill LK, et al. Complications associated with single-position prone lateral lumbar interbody fusion: a systematic review and pooled analysis. J Neurosurg Spine 2023;39:380-6. [Crossref] [PubMed]
- Ozgur BM, Aryan HE, Pimenta L, et al. Extreme Lateral Interbody Fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J 2006;6:435-43. [Crossref] [PubMed]
- Saadeh YS, Joseph JR, Smith BW, et al. Comparison of Segmental Lordosis and Global Spinopelvic Alignment After Single-Level Lateral Lumbar Interbody Fusion or Transforaminal Lumbar Interbody Fusion. World Neurosurg 2019;126:e1374-8.
- Briski DC, Goel VK, Waddell BS, et al. Does Spanning a Lateral Lumbar Interbody Cage Across the Vertebral Ring Apophysis Increase Loads Required for Failure and Mitigate Endplate Violation. Spine (Phila Pa 1976) 2017;42:E1158-64. [Crossref] [PubMed]
- Godzik J, Pereira BA, Hemphill C, et al. Minimally Invasive Anterior Longitudinal Ligament Release for Anterior Column Realignment. Global Spine J 2020;10:101S-10S.
- Kepler CK, Bogner EA, Herzog RJ, et al. Anatomy of the psoas muscle and lumbar plexus with respect to the surgical approach for lateral transpsoas interbody fusion. Eur Spine J 2011;20:550-6. [Crossref] [PubMed]
- Alluri RK, Vaishnav AS, Sivaganesan A, et al. Multimodality Intraoperative Neuromonitoring in Lateral Lumbar Interbody Fusion: A Review of Alerts in 628 Patients. Global Spine J 2023;13:466-71. [Crossref] [PubMed]
- Alluri R, Mok JK, Vaishnav A, et al. Intraoperative Neuromonitoring During Lateral Lumbar Interbody Fusion. Neurospine 2021;18:430-6. [Crossref] [PubMed]
- Manzur MK, Steinhaus ME, Virk SS, et al. Fusion rate for stand-alone lateral lumbar interbody fusion: a systematic review. Spine J 2020;20:1816-25. [Crossref] [PubMed]
- Yson SC, Sembrano JN, Santos ER, et al. Does prone repositioning before posterior fixation produce greater lordosis in lateral lumbar interbody fusion (LLIF)? J Spinal Disord Tech 2014;27:364-9. [Crossref] [PubMed]
- Ziino C, Konopka JA, Ajiboye RM, et al. Single position versus lateral-then-prone positioning for lateral interbody fusion and pedicle screw fixation. J Spine Surg 2018;4:717-24. [Crossref] [PubMed]
- Pawar AY, Hughes AP, Sama AA, et al. A Comparative Study of Lateral Lumbar Interbody Fusion and Posterior Lumbar Interbody Fusion in Degenerative Lumbar Spondylolisthesis. Asian Spine J 2015;9:668-74. [Crossref] [PubMed]
- Nakashima H, Kanemura T, Satake K, et al. Comparative Radiographic Outcomes of Lateral and Posterior Lumbar Interbody Fusion in the Treatment of Degenerative Lumbar Kyphosis. Asian Spine J 2019;13:395-402. [Crossref] [PubMed]


