
Spinopelvic sagittal realignment and incidence of adjacent segment disease after single-segment posterior lumbar inter-body fusion using 12° lordotic cages—a 2-year prospective cohort study
Highlight box
Key findings
• Posterior lumbar inter-body fusion (PLIF) with 12° lordotic cages improved segmental lordosis and global sagittal realignment, and achieved satisfactory clinical outcomes with a low incidence of adjacent segment disease (ASD).
What is known and what is new?
• In recent years, even with single-segment fusion, focusing attention on the fusion angle and an aim to achieve appropriate angled fusion have been reported as mandatory.
• The present study is the first prospective longitudinal study to examine realignment in spinopelvic segmental and global sagittal parameters and the incidence of ASD after PLIF with 12° lordotic cages. PLIF with 12° lordotic cages achieved spinopelvic segmental and global sagittal realignment, with satisfactory clinical outcomes and a low incidence of ASD during 2 years of follow-up.
What is the implication, and what should change now?
• These results suggest that achieving the correction of segmental lordosis and spinopelvic sagittal realignment using 12° lordotic cages in PLIF may prevent ASD and iatrogenic flat back.
Introduction
The importance of spinopelvic sagittal alignment and its implications for clinical outcomes after lumbar fusion surgery have recently been demonstrated (1,2). In addition, spinopelvic sagittal malalignment including segmental lordosis (SL) at the fused segment has been reported as one of the risk factors for adjacent segment disease (ASD) after posterior lumbar inter-body fusion (PLIF) (1,3-5). Moreover, particularly in the lower lumbar arc (L4–S1), SL at the fused segments was more important to prevent iatrogenic flat back after lumbar fusion surgery, because this arc forms a foundation of the lumbar spine and accounts for about 70% of lumbar lordosis (LL) (2,6-9). Therefore, some reports have noted the need to take into consideration acquisition of SL at the lower lumbar level even with single-segment PLIF (1,10).
However, previous studies have reported that PLIF with 0° rectangular cages cannot achieve the correction of SL (1,11-13). On the other hand, recent reports have suggested a relationship between cage angle and improvement of SL and spinopelvic global sagittal alignment after lumbar inter-body fusion (14-17). We therefore hypothesized that using lordotic cages in PLIF could acquire SL at the fused segment, which would improve spinopelvic global sagittal alignment and reduce the incidence of ASD. However, no longitudinal cohort studies appear to have determined the extent to which SL and spinopelvic global sagittal alignment could be acquired using lordotic cages in PLIF or the extent to which the development of ASD could be prevented. To exclude other factors in the present study, patients were limited to those with degenerative spondylolisthesis at L4/5 using the same fusion technique. The purpose of this study was to analyze changes in segmental and spinopelvic global sagittal alignment after single-segment PLIF with 12° lordotic cages for L4–5 degenerative spondylolisthesis, to clarify the relationship between changes in segmental and spinopelvic global sagittal alignment, and to report the clinical outcomes and incidence of ASD at 2 years postoperatively. We present this article in accordance with the STROBE reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-23-78/rc).
Methods
Subjects
This study was a 2-year prospective longitudinal cohort study. Subjects were patients who had undergone L4/5 PLIF using 12° lordotic polyetheretherketone cages for L4 degenerative spondylolisthesis. Twenty-eight consecutive patients (5 men, 23 women) were enrolled from 2014 to 2016. The exclusion criteria were the presence of scoliosis (Cobb angle >20°) or vertebral fractures. Mean age at the time of primary surgery was 66.9 years (range, 53–78 years). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was approved by the Institutional Review Board of Osaka Rosai Hospital (No. 27-2) and informed consent was taken from all the patients.
Surgical procedure
All procedures were performed using the same technique described elsewhere (18). Briefly, bilateral total facetectomy, subtotal discectomy, and local autologous bone graft with two cages were performed. The 12° lordotic cages were placed as far anterior of the disc space as possible. Finally, compression was applied with a rod system so that the cages and vertebral endplates could obtain close contact.
Clinical evaluations
The Japanese Orthopaedic Association (JOA) score was used to evaluate clinical outcomes. The JOA score consists of 4 categories and has a maximum score of 29. The low back pain (LBP) score of the JOA score ranges from 0 to 3 points (none, 0; occasionally mild, 1; usually mild and occasionally severe, 2; always severe, 3). The recovery rate (%) of the JOA score was calculated as: (postoperative JOA score − preoperative JOA score)/(29 − preoperative JOA score) × 100 (19). The JOA score was determined preoperatively and at 1 year and 2 years postoperatively. Operative ASD (O-ASD) was defined as a symptomatic condition in which additional operation was required to treat neurological deterioration at the adjacent degenerative segment (20).
Radiological evaluations
All patients had standing radiographs of the whole spine with inclusion of the femoral heads. Radiological measurements were examined preoperatively and at 3 months, 1 year and 2 years postoperatively. The following radiographic spinopelvic parameters were measured: SL at L4/5; sagittal vertical axis (SVA); T1 pelvic angle (TPA); thoracic kyphosis (TK); LL; sacral slope (SS); pelvic tilt (PT); and pelvic incidence (PI) in sagittal view. SL was measured from the upper endplate of L4 to the lower endplate of L5. SVA was measured as the distance between the C-7 plumb line and the superior posterior corner of the S1 vertebral body in the lateral radiograph. TPA was measured as the angle subtended by lines drawn from the center of the femoral head axis to the center of the T1 vertebral body and to the middle of the S1 endplate. TK was measured from the upper endplate of T5 to the lower endplate of T12. LL was measured from the upper endplate of L1 to the upper endplate of S1. SS was measured as the angle between the endplate of S1 and a horizontal line. PT was measured as the angle between the vertical line and the line connecting the midpoint of the sacral plate to the femoral head axis. PI was measured as the angle between the line perpendicular to the sacral plate at its midpoint and the line connecting this point to the femoral head axis (21-24). Realignment after PLIF was calculated by the change between 3 months postoperatively and the preoperative value (ΔSL, ΔLL, ΔSVA, ΔTPA, ΔTK, ΔSS, ΔPT), defined as the value at 3 months postoperatively minus the preoperative value. Cage subsidence was evaluated using lateral radiographs at 3 months and 2 years postoperatively, and was defined as present if a cage was observed to sink into an adjacent vertebral body by 2 mm (25). Radiological ASD (R-ASD) at 2 years postoperatively was defined as a condition in which a narrowing of disc height by >3 mm on lateral radiograph, posterior opening angle >5°, progression of anterior slippage by >3 mm on lateral flexion radiograph, or progression of posterior slippage by >3 mm on lateral extension radiograph was seen in comparison with preoperative radiographs at the adjacent segment level (L3/4 or L5/S) (20).
Statistical analysis
Radiological parameters were compared between preoperatively and 3 months, 1 year and 2 years postoperatively using the paired t-test for continuous variables and the chi-squared test for categorical variables. The Spearman correlation test was used to identify correlations between change in SL (ΔSL) and changes in other spinopelvic sagittal parameters (ΔSVA, ΔTPA, ΔTK, ΔLL, ΔSS, ΔPT, ΔPI-LL) between preoperatively and 3 months postoperatively. All statistical analyses were performed using IBM SPSS Statistics for Windows, version 21 (IBM Corp., New York, United States). Values of P<0.05 were considered significant.
Results
The follow-up rate was 100% (n=28) at 1 year postoperatively and 96.4% (n=27) at 2 years postoperatively.
Clinical outcomes
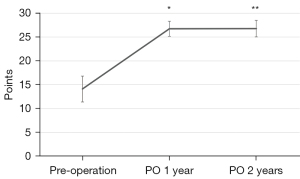
Mean JOA scores preoperatively and at 1 year and 2 years postoperatively were 14.1±2.7 (range, 7–18), 26.8±1.6 (range, 24–29), and 26.8±1.7 (range, 24–29), respectively. Recovery rates at 1 year and 2 years postoperatively were 85%±10% and 84.9%±11.7%, respectively. JOA scores and recovery rates improved significantly after primary surgery (P<0.01) (Figure 1). No cases of O-ASD were seen during the 2 years of follow-up.
Radiological outcomes
The bone union rate was 82.1% (n=23) at 1 year postoperatively and 96.3% (n=26) at 2 years postoperatively. The rate of cage subsidence was 18.5% (n=5) at 2 years postoperatively.
Comparison of pre- and postoperative radiographic parameters
Radiological parameters at preoperatively and 3 months, 1 year, and 2 years postoperatively and P values of pre- and postoperative comparisons are shown in Table 1. Postoperative SL was significantly corrected and maintained throughout the 2 years of follow-up. Similarly, spinopelvic sagittal parameters such as SVA, TPA, LL, PT and PI-LL were significantly corrected, and the effects of postoperative realignment were maintained throughout the 2-year follow-up period. PI-LL mismatch preoperatively and at 3 months, 1 year, and 2 years postoperatively were observed in 17, 12 patients (P=0.18), 11 patients (P=0.10) and 10 patients (P=0.07), respectively.
Table 1
| Radiographic parameters | Timing of radiographic evaluations | |||
|---|---|---|---|---|
| Preoperatively (n=28) | 3 months postoperatively (n=28) | 1 year postoperatively (n=28) | 2 years postoperatively (n=27) | |
| SL at L4/5 (°) | 14.4 (4.1) | 18.0 (5.2)** | 18.3 (5.6)†† | 18.5 (5.5)‡‡ |
| SVA (mm) | 52.7 (53.7) | 29.1 (25.3)* | 30.5 (34.1)† | 36.2 (29.0) |
| TPA (°) | 22.1 (8.0) | 18.3 (7.4)** | 17.4 (7.3)†† | 18.2 (6.4)‡‡ |
| TK (°) | 29.1 (8.4) | 30.0 (7.0) | 32.0 (7.9)†† | 32.3 (7.2)‡ |
| LL (°) | 41.9 (11.4) | 44.9 (9.9)* | 46.1 (9.1)†† | 46.0 (9.5)‡‡ |
| SS (°) | 31.5 (7.3) | 31.8 (7.4) | 33.3 (6.2)† | 33.3 (6.4)‡ |
| PT (°) | 23.8 (8.0) | 22.3 (6.8)* | 20.9 (6.8)†† | 21.1 (6.6)‡‡ |
| PI (°) | 55.3 (11.1) | 54.3 (10.0) | 54.1 (9.3) | 54.5 (9.5) |
| PI-LL (°) | 13.4 (10.4) | 9.5 (7.9)** | 8.0 (8.5)†† | 8.5 (7.9)‡‡ |
Data are expressed as mean (SD). *, P<0.05; **, P<0.01 (preoperatively vs. 3 months postoperatively); †, P<0.05; ††, P<0.01 (preoperatively vs. 1 year postoperatively); ‡, P<0.05; ‡‡, P<0.01 (preoperatively vs. 2 years postoperatively). SL, segmental lordosis; SVA, sagittal vertical axis; TPA, T1 pelvic angle; TK, thoracic kyphosis; LL, lumbar lordosis; SS, sacral slope; PT, pelvic tilt; PI, pelvic incidence; SD, standard deviation.
Correlations of change in segmental lordosis (ΔSL) and changes in spinopelvic sagittal alignment (ΔSVA, ΔTPA, ΔTK, ΔLL, ΔSS, ΔPT, ΔPI-LL)
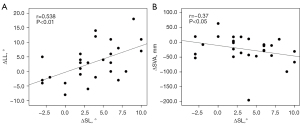
At 3 months postoperatively, ΔSL was 3.6°. With respect to spinopelvic global parameters, ΔSVA was −23.6 mm, ΔTPA was −3.8°, ΔTK was 0.8°, ΔLL was 3°, ΔSS was 0.3°, ΔPT was −1.5° and ΔPI-LL was −3.9°. Regarding the correlation between ΔSL and spinopelvic global parameters, significant correlations were detected in ΔSVA (r=−0.37, P<0.05) and ΔLL (r=0.538, P<0.01) (Figure 2). No correlations were seen with other parameters.
Radiological ASD at 2 years
R-ASD was observed in 3 patients (11.1%). Two patients showed narrowing of disc height by >3 mm at the L5/S level and one patient showed progression of posterior slippage by >3 mm at the L3/4 level. No patients displayed posterior opening >5° or progression of anterior slippage by >3 mm (Table 2).
Table 2
| Type of radiological change | Level, n (%) | |
|---|---|---|
| L3/4 | L5/S | |
| Disc height narrowing >3 mm | 0 (0.0) | 2 (7.4) |
| Posterior opening angle >5° | 0 (0.0) | 0 (0.0) |
| Progression of slippage >3 mm | 1 (3.7) | 0 (0.0) |
Representative case
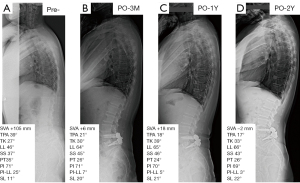
A 55-year-old woman achieved and maintained spinopelvic segmental and global sagittal realignment after PLIF using 12° lordotic cages (Figure 3). No R-ASD was encountered. JOA score improved significantly from 10 preoperatively to 28 at 2 years postoperatively.
Discussion
Spinopelvic alignment after lumbar fusion is a very important factor that affects the long-term outcomes. In recent years, even with single-segment fusion, focusing attention on the fusion angle and an aim to achieve appropriate angled fusion have been reported as mandatory (1,10,15,16). To the best of our knowledge, the present study is the first prospective longitudinal study to examine realignment in spinopelvic segmental and global sagittal parameters and the incidence of ASD after PLIF with 12° lordotic cages, limited to the same fusion segment and number of fusions using standing radiographs of the whole spine. PLIF with 12° lordotic cages for L4-5 degenerative spondylolisthesis achieved spinopelvic segmental and global sagittal realignment, with satisfactory clinical outcomes and a low incidence of ASD during 2 years of follow-up.
Causes of realignment after lumbar fusion surgery can be mainly divided into effects of decompression and correction of segmental alignment at the fused segment. In terms of the effects of decompression, some authors have reported reactive lumbar and global sagittal realignment after decompression without fusion (26-28). As the mechanisms of realignment, decreased epidural pressure and the release of neurological symptoms after decompression have been speculated to lead to spinopelvic global realignment, because in patients with degenerative lumbar stenosis, anterior displacement of the C-7 plumb line and the loss of lordosis occur as protective mechanisms to avoid neurological symptoms (26,28,29). The effect of decompression was also considered to be involved in the results of spinopelvic global realignment in the present study. However, acquiring the correction of segmental alignment by decompression alone was difficult. In terms of the effects of correcting segmental alignment after lumbar fusion, a relationship between cage angle and spinopelvic sagittal alignment has been reported (11,14-16,30). Gödde et al. noted that cage geometry has a significant impact on alignment of the lumbar spine after PLIF (11). They concluded that SL and LL decreased with 0° rectangular cages, but significantly increased with various wedge-shaped cages. In fact, we have previously reported that SL decreased slightly in PLIF with 0° rectangular cages (1). Moreover, Hong et al. reported that in transforaminal lumbar inter-body fusion, cages with a 15° lordotic angle achieved higher restoration of SL and LL than 4° or 8° cages (16). They concluded that the lordotic angle of the cages determined the degree of restoration of LL. Similarly, in the present study, SL and various spinopelvic global parameters (SVA, TPA, LL, PT, PI-LL) were significantly improved after PLIF with 12° lordotic cages. Spinopelvic global sagittal realignment in the present study was attributed to the effects of decompression and the corrected SL in the lower lumbar arc, which provides the foundation of the lumbar spine. Actually, in the present study, ΔSL and ΔLL showed a significant positive correlation, and ΔSL and ΔSVA showed a significant negative correlation, suggesting that the acquisition of SL using 12° lordotic cages was key to spinopelvic sagittal realignment in PLIF. However, these correlations were weak with low r values, because the effect of PLIF between single-segments alone on global alignment is limited.
Several studies have reported on relationships between spinopelvic sagittal alignment and ASD. Kumar et al. reported that patients who had an abnormal C7 plumb line position and/or SS experienced a significantly higher rate of ASD (31). With respect to LL and PI-LL, lower LL and PI-LL mismatch have been suggested as risk factors for ASD after lumbar fusion (4,32,33). Rothenfluh et al. reported that patients with PI-LL mismatch had a 10-fold greater risk of developing ASD than controls (4). We have also reported that preoperative higher SVA, higher PT, lower LL and PI-LL mismatch were associated with ASD after PLIF using 0° rectangular cages at the L4/5 segment (1). Furthermore, regarding SL, Umehara et al. reported in a biomechanical study that hypolordosis in the fused segments caused increased loading of the posterior column in the adjacent segments (3). Moreover, Kim et al. suggested that maintaining the L4/5 SL at >20° was important for preventing clinical ASD (34). Okuda et al. reported that decreased ΔSL after PLIF represented a risk factor for early-onset ASD within 2 years (35). They also reported the difficulty of acquiring the SL after PLIF with 0° rectangular cages and the incidences of early-onset ASD were 19% for R-ASD and 5% for O-ASD at 2 years postoperatively (1,20). In the present study, the incidences of ASD were 11.1% for R-ASD and 0% for O-ASD at 2 years postoperatively; there was a low incidence of ASD. Therefore, these results also suggested that appropriate SL after L4/5 PLIF with 12° lordotic cages leads to the realignment of spinopelvic global parameters and prevention of ASD. Particularly in lower lumbar fusion surgery, we should consider various options such as using lordotic cages to acquire SL at the fused segment and thus avoid creating an iatrogenic flat back.
The present study has several limitations. First was the small number of patients. Second, the follow-up period was short. Third, cages with other lordotic angles were not evaluated as a control group. Further long-term follow-up is needed to identify the long-term radiological alignment and incidence of ASD.
Conclusions
In conclusion, realignment in segmental and spinopelvic global parameters and the incidence of ASD after PLIF using 12° lordotic cages for L4–5 degenerative spondylolisthesis were investigated. PLIF with 12° lordotic cages allowed the acquisition and maintenance of segmental correction and spinopelvic global realignment, and the incidence of R-ASD was 11.1% and O-ASD was 0% within 2 years. These results suggest that achieving the correction of SL and spinopelvic sagittal realignment using 12° lordotic cages in PLIF may prevent ASD and iatrogenic flat back.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-23-78/rc
Data Sharing Statement: Available at https://jss.amegroups.com/article/view/10.21037/jss-23-78/dss
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-23-78/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-23-78/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was approved by the Institutional Review Board of Osaka Rosai Hospital (No. 27-2) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Matsumoto T, Okuda S, Maeno T, et al. Spinopelvic sagittal imbalance as a risk factor for adjacent-segment disease after single-segment posterior lumbar interbody fusion. J Neurosurg Spine 2017;26:435-40. [Crossref] [PubMed]
- Le Huec JC, Faundez A, Dominguez D, et al. Evidence showing the relationship between sagittal balance and clinical outcomes in surgical treatment of degenerative spinal diseases: a literature review. Int Orthop 2015;39:87-95. [Crossref] [PubMed]
- Umehara S, Zindrick MR, Patwardhan AG, et al. The biomechanical effect of postoperative hypolordosis in instrumented lumbar fusion on instrumented and adjacent spinal segments. Spine (Phila Pa 1976) 2000;25:1617-24. [Crossref] [PubMed]
- Rothenfluh DA, Mueller DA, Rothenfluh E, et al. Pelvic incidence-lumbar lordosis mismatch predisposes to adjacent segment disease after lumbar spinal fusion. Eur Spine J 2015;24:1251-8. [Crossref] [PubMed]
- Tartara F, Garbossa D, Armocida D, et al. Relationship between lumbar lordosis, pelvic parameters, PI-LL mismatch and outcome after short fusion surgery for lumbar degenerative disease. Literature review, rational and presentation of public study protocol: RELApSE study (registry for evaluation of lumbar artrodesis sagittal alignEment). World Neurosurg X 2023;18:100162. [Crossref] [PubMed]
- Janik TJ, Harrison DD, Cailliet R, et al. Can the sagittal lumbar curvature be closely approximated by an ellipse? J Orthop Res 1998;16:766-70. [Crossref] [PubMed]
- Barrey C, Darnis A. Current strategies for the restoration of adequate lordosis during lumbar fusion. World J Orthop 2015;6:117-26. [Crossref] [PubMed]
- Nagamoto Y, Okuda S, Matsumoto T, et al. Multiple-Repeated Adjacent Segment Disease After Posterior Lumbar Interbody Fusion. World Neurosurg 2019;121:e808-16.
- Takahashi Y, Okuda S, Nagamoto Y, et al. Effect of segmental lordosis on the clinical outcomes of 2-level posterior lumbar interbody fusion for 2-level degenerative lumbar spondylolisthesis. J Neurosurg Spine 2019; Epub ahead of print. [Crossref]
- Kong LD, Zhang YZ, Wang F, et al. Radiographic Restoration of Sagittal Spinopelvic Alignment After Posterior Lumbar Interbody Fusion in Degenerative Spondylolisthesis. Clin Spine Surg 2016;29:E87-92. [Crossref] [PubMed]
- Gödde S, Fritsch E, Dienst M, et al. Influence of cage geometry on sagittal alignment in instrumented posterior lumbar interbody fusion. Spine (Phila Pa 1976) 2003;28:1693-9. [Crossref] [PubMed]
- Rice JW, Sedney CL, Daffner SD, et al. Improvement of Segmental Lordosis in Transforaminal Lumbar Interbody Fusion: A Comparison of Two Techniques. Global Spine J 2016;6:229-33. [Crossref] [PubMed]
- Lee CW, Yoon KJ, Ha SS. Which Approach Is Advantageous to Preventing Development of Adjacent Segment Disease? Comparative Analysis of 3 Different Lumbar Interbody Fusion Techniques (ALIF, LLIF, and PLIF) in L4-5 Spondylolisthesis. World Neurosurg 2017;105:612-22. [Crossref] [PubMed]
- Sembrano JN, Horazdovsky RD, Sharma AK, et al. Do Lordotic Cages Provide Better Segmental Lordosis Versus Nonlordotic Cages in Lateral Lumbar Interbody Fusion (LLIF)? Clin Spine Surg 2017;30:E338-43.
- Kim CH, Chung CK, Park SB, et al. A Change in Lumbar Sagittal Alignment After Single-level Anterior Lumbar Interbody Fusion for Lumbar Degenerative Spondylolisthesis With Normal Sagittal Balance. Clin Spine Surg 2017;30:291-6. [Crossref] [PubMed]
- Hong TH, Cho KJ, Kim YT, et al. Does Lordotic Angle of Cage Determine Lumbar Lordosis in Lumbar Interbody Fusion? Spine (Phila Pa 1976) 2017;42:E775-80.
- Toop N, Viljoen S, Baum J, et al. Radiographic and clinical outcomes in one- and two-level transforaminal lumbar interbody fusions: a comparison of bullet versus banana cages. J Neurosurg Spine 2022;36:918-27. [Crossref] [PubMed]
- Okuda S, Oda T, Miyauchi A, et al. Surgical outcomes of posterior lumbar interbody fusion in elderly patients. Surgical technique. J Bone Joint Surg Am 2007;89:310-20. [Crossref] [PubMed]
- Matsumoto T, Okuda S, Nagamoto Y, et al. Effects of Concomitant Decompression Adjacent to a Posterior Lumbar Interbody Fusion Segment on Clinical and Radiologic Outcomes: Comparative Analysis 5 Years After Surgery. Global Spine J 2019;9:505-11. [Crossref] [PubMed]
- Okuda S, Nagamoto Y, Matsumoto T, et al. Adjacent Segment Disease After Single Segment Posterior Lumbar Interbody Fusion for Degenerative Spondylolisthesis: Minimum 10 Years Follow-up. Spine (Phila Pa 1976) 2018;43:E1384-8. [Crossref] [PubMed]
- Schwab FJ, Blondel B, Bess S, et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976) 2013;38:E803-12. [Crossref] [PubMed]
- Rose PS, Bridwell KH, Lenke LG, et al. Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine (Phila Pa 1976) 2009;34:785-91. [Crossref] [PubMed]
- Baghdadi YM, Larson AN, Dekutoski MB, et al. Sagittal balance and spinopelvic parameters after lateral lumbar interbody fusion for degenerative scoliosis: a case-control study. Spine (Phila Pa 1976) 2014;39:E166-73. [Crossref] [PubMed]
- Protopsaltis T, Schwab F, Bronsard N, et al. The T1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. J Bone Joint Surg Am 2014;96:1631-40. [Crossref] [PubMed]
- Kim MC, Chung HT, Cho JL, et al. Subsidence of polyetheretherketone cage after minimally invasive transforaminal lumbar interbody fusion. J Spinal Disord Tech 2013;26:87-92. [Crossref] [PubMed]
- Suzuki H, Endo K, Kobayashi H, et al. Total sagittal spinal alignment in patients with lumbar canal stenosis accompanied by intermittent claudication. Spine (Phila Pa 1976) 2010;35:E344-6. [Crossref] [PubMed]
- Fujii K, Kawamura N, Ikegami M, et al. Radiological improvements in global sagittal alignment after lumbar decompression without fusion. Spine (Phila Pa 1976) 2015;40:703-9. [Crossref] [PubMed]
- Dohzono S, Toyoda H, Takahashi S, et al. Factors associated with improvement in sagittal spinal alignment after microendoscopic laminotomy in patients with lumbar spinal canal stenosis. J Neurosurg Spine 2016;25:39-45. [Crossref] [PubMed]
- Barrey C, Jund J, Noseda O, et al. Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J 2007;16:1459-67. [Crossref] [PubMed]
- Youn YH, Cho KJ, Na Y, et al. Global Sagittal Alignment and Clinical Outcomes after 1-3 Short-Segment Lumbar Fusion in Degenerative Spinal Diseases. Asian Spine J 2022;16:551-9. [Crossref] [PubMed]
- Kumar MN, Baklanov A, Chopin D. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J 2001;10:314-9. [Crossref] [PubMed]
- Senteler M, Weisse B, Snedeker JG, et al. Pelvic incidence-lumbar lordosis mismatch results in increased segmental joint loads in the unfused and fused lumbar spine. Eur Spine J 2014;23:1384-93. [Crossref] [PubMed]
- Djurasovic MO, Carreon LY, Glassman SD, et al. Sagittal alignment as a risk factor for adjacent level degeneration: a case-control study. Orthopedics 2008;31:546.
- Kim KH, Lee SH, Shim CS, et al. Adjacent segment disease after interbody fusion and pedicle screw fixations for isolated L4-L5 spondylolisthesis: a minimum five-year follow-up. Spine (Phila Pa 1976) 2010;35:625-34. [Crossref] [PubMed]
- Okuda S, Nagamoto Y, Takenaka S, et al. Effect of segmental lordosis on early-onset adjacent-segment disease after posterior lumbar interbody fusion. J Neurosurg Spine 2021;35:454-9. [Crossref] [PubMed]


