
Salvage of failed direct lateral sacroiliac joint fixation using a new percutaneous lateral-oblique transfixation technique with two variable-threaded screws: a multicenter case report of three cases
Highlight box
Key findings
• First article demonstrating a new salvage technique for sacroiliac joint (SIJ) pseudoarthrosis after direct lateral fixation.
• A new percutaneous lateral-oblique transfixation technique.
What is known and what is new?
• Revision of a failed direct lateral SIJ implant requires an open incision through the gluteal muscles.
• New technique for salvage of SIJ pseudoarthrosis after direct lateral fixation without implant removal.
What is the implication, and what should change now?
• Revise SIJ failure without implant removal.
• Patients discharged home the same day.
• 89% pain improvement, short procedure time, approximate 1 inch incision, and less than five cc blood loss.
Introduction
Background
Lower back pain caused by the sacroiliac joint (SIJ) is frequently overlooked (1-3). The SIJ is estimated to be a cause of chronic low back pain in 15–30% (4) of patients presenting for evaluation and in about 40% of patients with low back pain who had a prior lumbar instrumented fusion (5). The SIJ is complex in nature and is the largest axial joint in the body, which allows for mobility of the spine with the pelvis (6). The biomechanics of the joint does not allow for much stability against the shear loads which causes instability of the joint (6,7). Secondary surgery rates are especially higher with L5–S1 fusion which is increases with long-segment fusion and extended instrumentation to the pelvis (8).
With the popularization of the triangular titanium implant (TTI) wedges (iFuse Implant System, SI-Bone, Inc., Santa Clara, CA, USA) surgeons have utilized a percutaneous direct lateral approach to perform SIJ fusion. Randomized clinical trials have shown superior pain improvement and quality of life in patients who underwent direct lateral SIJ fusion versus non-operative treatment (9-11). The TTI is designed for SIJ fusion based on bone adherence to the surface and three devices are recommended for rotational stability. One or more may not achieve fusion and thus have the likelihood for pain. There is a reported up to 16.4% risk of adverse events using the direct lateral approach (12,13). The revision rate for SIJ using a direct lateral approach ranged from 5.7% to 30.8% (14). Faced with pseudoarthrosis, the differential diagnosis may include infection, although rare. Shamrock et al. evaluated fourteen studies, found a 2% incidence of wound infection and a 1.6% incidence of nerve root impingement (15). Postoperatively, patients were required to restrict weight bearing for up to six weeks.
Rationale and knowledge gap
The revision of failed direct lateral SIJ implant has traditionally required an open incision through the gluteal muscles and dissection through scar tissue within the area where the superior gluteal neurovascular structures reside. The exact percentage of patients who require revision of their iFuse implants is unknown, but published data in one study reported 3.6% at 4 years (16). Given the potential morbidity from revising failed direct lateral SIJ implants, Sacrix® Limited Liability Company (LLC) (Malden, MA, USA) developed a new cannulated variable-threaded device called SacroFuse® (Figure 1) and a new percutaneous lateral-oblique transfixation technique to fixate the SIJ around the failed direct lateral SIJ implants percutaneously without removing them.
Objective
We hypothesized that a lateral-oblique technique to place two variable-threaded screws could be used to fixate the SIJ without the need to remove the failed implants. Our objective was to describe the technique and used three illustrative cases performed by two surgeons in separate facilities who were trained by the surgeon (primary author). We present this case report in accordance with the CARE reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-23-43/rc).
Case presentation
Three patients were enrolled in this study with failed direct lateral SIJ fusions with three implants. An independent radiologist and the operating orthopedic spine surgeon evaluated the preoperative and postoperative plain radiographs. All three revision surgeries were performed through a new posterior incision over the lateral border of the iliac crest without removing the existing implants. The inclusion criteria for surgery included a history of lower back and buttock pain, painful physical examination, unassisted ambulation, positive diagnostic intra-articular SIJ injections, positive imaging for pseudoarthrosis, and failed conservative management (such as medication and activity modification) for at least 6 months. On plain radiographs and/or computed tomography (CT) scans, signs of halo and implant migration were suggestive of probable loosening. Clinical patients had at least three out of five provocative positive SIJ pain tests: distraction, thigh thrust, compression, Gaenslen’s and flexion, abduction, and external rotation (FABER). All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Prior to surgery, all patients signed an informed consent form that explained the procedure, risks, and benefits and were informed of data collection for research purposes. Data regarding these groups were collected from medical records and operative notes. Western Institutional Review Board approval was granted through protocol # 20181251.
Surgical technique
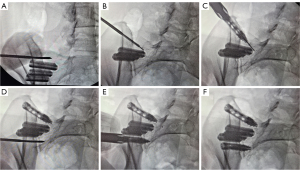
Each surgeon underwent training on a cadaver with the board-certified orthopedic spine surgeon who was the inventor of the new technique and the variable-threaded screws. The patient was placed prone after general anesthesia and sterile preparation was performed. The fluoroscope was tilted to 20–30 degrees cephalad (pelvic outlet view) to flatten the S1 endplate then rotated 20–30 degrees contralateral oblique to visualize the SIJ and the posterior lateral border of the iliac crest and medial teardrop illustrating the top of the iliac crest (17) (Figure 2). Marcaine with epinephrine was injected approximately 2 cm lateral to the line and caudal to the S1 endplate line within the alar skin markings. A Jamshidi needle was placed through the skin under direct hand control. The S1 screw trajectory was aimed towards the tip of the S1 sacral promontory and below the L5–S1 disc space. A direct lateral fluoroscopic view was used to ensure that the Jamshidi needle was docked high on the lateral border of the iliac crest above the posterior margin of the sacrum. Using a percutaneous technique, the Jamshidi needle was inserted across the SIJ into the sacral alar above the laterally placed implants. A smooth, blunted tip Nitinol guidewire was inserted through the Jamshidi needle into the alar. The Jamshidi was removed and an approximate 1-inch incision was made around the guidewire. A dilator was inserted over the guidewire and a working cannula was inserted and docked on the iliac crest. The position was confirmed using fluoroscopy, and the dilator was removed to leave the working cannula. A 12 mm × 60 mm screw was prepacked with NanoFuse Biologics Putty (NanoFuse Biologics LLC, Malden, MA, USA) and inserted over the guidewire at the S1 level under a pelvic inlet view to confirm that the screw would not breach the anterior border of the sacral alar. The procedure was repeated for the placement of a second screw measuring 12 mm × 50 mm at the S2 level below the laterally placed implants. The screws were placed along the outer border of the iliac crest posteriorly and advanced obliquely and anteriorly across the SI joint into the sacral alar at the S1 and S2 levels, allowing for cancellous bone self-harvest and purchase. Screw placement was confirmed with intraoperative fluoroscopy using multiple views. Figure 3 shows fluoroscopic images of the surgical technique steps in a failed direct lateral case with three TTI wedges. After irrigation and hemostasis, the wound was closed in layers and a dry sterile dressing was applied.

Case 1
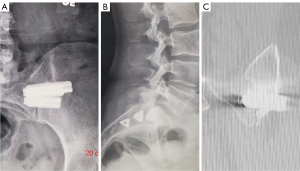
The first case was a 47-year-old female with recurrent but worse left SIJ pain radiating towards the hip and groin after SIJ fusion using three TTI wedges. The pain was exacerbated with standing, walking and physical activities. The patient had localized tenderness over the sacral sulcus, SIJ provocative tests and radiographic evidence of loosening of the implants suggesting pseudoarthrosis, as shown in Figure 4A. At 20 months post op, a revision of the left SIJ fusion was performed and two variable-threaded screws were placed, one cephalad and one caudal to the three TTI wedges, under fluoroscopic guidance. At 22-month follow-up, postoperative anteroposterior (AP) and lateral radiographs showed satisfactory placement of the two screws (Figure 4B,4C).

Case 2
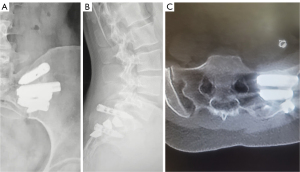
The second case was a 40-year-old female with left buttock pain and diagnosed with instability of the left SIJ after pregnancy. She underwent left SIJ fixation with three TTI but within a year, she was found to have recurrent left buttock pain and intermittent radiation to the left groin with prolonged sitting, standing and activities. The patient reported tenderness over the left SIJ and a positive response to provocative tests on physical examination. There was radiographic suspicion of lucency around two of the three TTI (Figure 5A,5B). A coronal CT scan confirmed implant migration and lucency around the tip of the TTI (Figure 5C) suggestive of pseudoarthrosis. The patient underwent a revision left SIJ fixation at 26 months and in this case, the first screw was placed cephalad to the TTI wedges while the second screw was placed between the remaining two wedges. Postoperative AP and lateral radiographs showed fusion (Figure 6A,6B), confirmed on axial CT scan at 10-month follow-up (Figure 6C).
Case 3
The third case involved a 61-year-old male with a lumbar fusion with recurrent right buttock pain and intermittent radiating pain to the groin following a prior right SIJ fixation using three CoreLink Entasis screws (CoreLink, St. Louis, MO, USA). There was pain focused around the right SIJ and positive provocative SIJ compression tests on physical examination. At 36 months post op, two SacroFuse® variable-threaded screws were successfully placed cephalad and caudal to the lateral implants seen on postoperative AP and lateral radiographs (Figure 7A,7B), Fusion was confirmed on axial CT scan at 6 months (Figure 7C). The patient latest follow up was at 26 months.
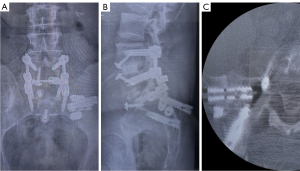
All the patients were discharged home the same day. The time between the initial SIJ fixation surgery and the salvage procedure ranged from 20, 26 and 36 months. The mean procedure time was 20 minutes, with blood loss of less than five cc. The incision size was approximately 1 inch. The prior SIJ fixation implants were left untouched. We found CT scan evidence of solid fusion as early as 6 months (Figure 7C). The patients reported immediate reduction in their preoperative pain after the revision surgery with the Sacrix technique, but all patients still had some residual pain at baseline at the latest follow-up. There was an 89% decrease in pain from the mean preoperative Visual Analog Score (VAS) score of 9.5 to the mean postoperative VAS score of 1 at the latest follow-up. There were no complications or implant failures.
Discussion
Key findings
The Sacrix® percutaneous lateral-oblique transfixation approach with two variable-threaded screws allows for oblique screw placement across the SIJ for favorable biomechanical strength and direct compression of the joint increasing the possibility of fusion while avoiding the failed direct laterally placed implants. This technique avoids gluteal muscle disruption, as observed with the direct lateral approach. The entry point was the posterior superior iliac spine and was performed percutaneously without any tissue dissection. This entry point was relatively superficial in all patients. The trajectory also avoided all neurovascular structures which are at risk with the direct lateral approach. The devices are placed diagonally across the SI joint, which transfixes the joint from the instantaneous axis of rotation (IAR), and limits rotations (18). Furthermore, the technique described in this report was shown to be effective with just using two screws (17). To our knowledge, these are the first three cases to illustrate the salvage of a failed laterally placed SIJ fixation using a percutaneous lateral-oblique transfixation technique with two variable-threaded screws.
Strengths and limitations
Given that there are only three illustrative cases, we may not be capturing the full scope of the possible clinical, radiographic, and technical experience in all patients. Therefore, there is prospect for limited surveillance of possible adverse events. However, the technique is reproducible as it uses the iliac crest as a landmark to place the screws, which is anatomically consistent among patients and the oblique inlet radiographic view to avoid the previous implants which allows for direct visualization of the screw trajectory and length.
Comparison with similar research
Transfixing the SI joint to stop painful micromotion forms a foundation for the rationale of the direct lateral approach used to treat the three patients described. While this is the first article to detail a lateral-oblique approach with variable-threaded screws, Sayed et al. reported the utilization of a posteriorly placed cortical allograft within the SIJ to salvage a failed direct lateral SIJ fusion at a mean interval time of 19.7 months (19). Whang et al. reported evidence of bony fusion at the SIJ for three TTI increased from 45% at 12 months to 71% at 24 months (20). Chin et al. confirmed fused SIJ following the Sacrix technique at 24 months using two screws (17). In our study, the time interval between the initial SIJ fixation surgery and the salvage procedure ranged between 20 to 36 months.
Explanations of findings
The percutaneous approach in this study aimed to salvage a difficult problem when a SIJ fixation device fails using the direct lateral approach and placement of three implants. This leaves little room for additional direct lateral implants, and it is highly morbid to remove the failed implants. The surgeons felt that they needed a strong trans-articular fixation technique that would fixate the SIJ with the direct lateral implants still in place. Procedures such as the direct lateral approach are aimed at stabilizing the large SIJ directly at or in close proximity to the IAR are likely to face a mechanical disadvantage compared to techniques that block motion further away from the IAR such as the lateral-oblique approach (18). The rate of revision for direct lateral SIJ ranged from 5.7% to 30.8% (14). The primary treatment goals of achieving immediate stability and long-term fusion were successfully accomplished. While the patients experienced a reduction in pain, they still reported some residual baseline pain. We suspected that the prolonged duration of symptoms in these patients may have led to the development of chronic pain, which persisted even after the treatment goal of stabilization and radiographic SIJ fusion with Sacrix was reached.
Implications and actions needed
The SI joint has a large surface area and, when healthy, has very little movement, that causes pain. It is thought that ligamentous laxity, such as after childbirth, can lead to painful micromotion. Other conditions, such as arthritis, trauma, infection, and stressors from adjacent lumbar fusion, may also contribute to painful micromotion. With an increase in recognition that over 22% of patients who present with back pain have SIJ pain rather than back pain (4) and the over 43% of lumbar instrumented fusions have adjacent segment breakdown of their SI joint (5), we see increasing publications on SIJ fusions (9,10,21,22). In this report, there was a delay in surgical intervention between failed conservative treatment and the salvage SIJ surgery because the surgeons did not have a revision option, other than an open surgery, to remove the laterally placed TTIs and screws, which carries significant risks. We expect to see higher incidences of failed diret lateral SIJ fixation being revised with the Sacrix technique as more surgeons become aware of this new salvage technique. Patients can also benefit from earlier intervention.
Conclusions
The percutaneous lateral-oblique transfixation technique can be used for salvaging failed direct lateral SIJ fusion without the removal of the prior implants. It utilizes an approximate 1-inch incision. Using this technique, two variable-threaded screws can be safely placed along the outer border of the iliac crest posteriorly and advanced obliquely and anteriorly across the SI joint into the sacral alar at the S1 and S2 levels, allowing for cancellous bone self-harvest and purchase. This trajectory has a favorable mechanical advantage when considering the anterior location of the IAR within the synovial portion of the joint. This less invasive technique avoids gluteal muscle disruption and neurovascular injuries. All three patients had improved clinical symptoms and achieved SIJ fusion despite not moving the original implants. The Sacrix technique is simple and reproducible and thus could be taught to a broad cohort of physicians who treat patients with SIJ pain. A larger case series would be needed to confirm this conclusion. With the Sacrix technique, we observed CT scan confirmation of SIJ bony fusion as early as 6 months. In conclusion, the Sacrix technique may be considered as an early intervention in patients who present with persistent and recurrent pain after 6 months post SIJ fixation with radiographic evidence of pseudoarthrosis.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-23-43/rc
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-23-43/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-23-43/coif). KRC is the co-founder and CEO of Kingsley Investment Company (KIC) Ventures and has ownership shares in the company. WMC and ES have shares in Kingsley Investment Company (KIC) Ventures. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Prior to surgery, all patients signed an informed consent form that explained the procedure, risks, and benefits and were informed of data collection for research purposes. Data regarding these groups were collected from medical records and operative notes. Western Institutional Review Board approval was granted through protocol # 20181251.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ebraheim NA, Elgafy H, Semaan HB. Computed tomographic findings in patients with persistent sacroiliac pain after posterior iliac graft harvesting. Spine (Phila Pa 1976) 2000;25:2047-51. [Crossref] [PubMed]
- Frymoyer JW, Howe J, Kuhlmann D. The long-term effects of spinal fusion on the sacroiliac joints and ilium. Clin Orthop Relat Res 1978;196-201.
- Maigne JY, Planchon CA. Sacroiliac joint pain after lumbar fusion. A study with anesthetic blocks. Eur Spine J 2005;14:654-8. [Crossref] [PubMed]
- Barros G, McGrath L, Gelfenbeyn M. Sacroiliac Joint Dysfunction in Patients With Low Back Pain. Fed Pract 2019;36:370-5.
- Cross WW, Tavanaiepour K, Paschel EE, et al. Percutaneous Sacroiliac Joint Fusion: Indications and Technique. Operative Techniques in Orthopaedics 2017;27:236-41.
- Kiapour A, Joukar A, Elgafy H, et al. Biomechanics of the Sacroiliac Joint: Anatomy, Function, Biomechanics, Sexual Dimorphism, and Causes of Pain. Int J Spine Surg 2020;14:3-13. [Crossref] [PubMed]
- Lee YC, Lee R, Harman C. The incidence of new onset sacroiliac joint pain following lumbar fusion. J Spine Surg 2019;5:310-4. [Crossref] [PubMed]
- Turel MK, Kerolus M, Deutsch H. Minimally Invasive Sacroiliac Fixation for Extension of Fusion in Cases of Failed Lumbosacral Fusion. J Neurosci Rural Pract 2018;9:574-7. [Crossref] [PubMed]
- Polly DW, Swofford J, Whang PG, et al. Two-Year Outcomes from a Randomized Controlled Trial of Minimally Invasive Sacroiliac Joint Fusion vs. Non-Surgical Management for Sacroiliac Joint Dysfunction. Int J Spine Surg 2016;10:28. [Crossref] [PubMed]
- Dengler J, Kools D, Pflugmacher R, et al. Randomized Trial of Sacroiliac Joint Arthrodesis Compared with Conservative Management for Chronic Low Back Pain Attributed to the Sacroiliac Joint. J Bone Joint Surg Am 2019;101:400-11. [Crossref] [PubMed]
- Sturesson B, Kools D, Pflugmacher R, et al. Six-month outcomes from a randomized controlled trial of minimally invasive SI joint fusion with triangular titanium implants vs conservative management. Eur Spine J 2017;26:708-19. [Crossref] [PubMed]
- Lee DW, Patterson DG, Sayed D. Review of Current Evidence for Minimally Invasive Posterior Sacroiliac Joint Fusion. Int J Spine Surg 2021;15:514-24. [Crossref] [PubMed]
- Schoell K, Buser Z, Jakoi A, et al. Postoperative complications in patients undergoing minimally invasive sacroiliac fusion. Spine J 2016;16:1324-32. [Crossref] [PubMed]
- Spain K, Holt T. Surgical Revision after Sacroiliac Joint Fixation or Fusion. Int J Spine Surg 2017;11:5.
- Shamrock AG, Patel A, Alam M, et al. The Safety Profile of Percutaneous Minimally Invasive Sacroiliac Joint Fusion. Global Spine J 2019;9:874-80. [Crossref] [PubMed]
- Cher DJ, Reckling WC, Capobianco RA. Implant survivorship analysis after minimally invasive sacroiliac joint fusion using the iFuse Implant System Med Devices (Auckl) 2015;8:485-92. [Crossref] [PubMed]
- Chin KR, Pencle FJ, Seale JA, et al. CT Scan and Clinical Outcomes of Novel Lateral-Oblique Percutaneous Sacroiliac Joint (SIJ) Fixation: Technique and Literature Review. Cureus 2021;13:e16408. [Crossref] [PubMed]
- Beck CE, Jacobson S, Thomasson E. A Retrospective Outcomes Study of 20 Sacroiliac Joint Fusion Patients. Cureus 2015;7:e260. [Crossref] [PubMed]
- Sayed D, Khatri N, Rupp A, et al. Salvage of Failed Lateral Sacroiliac Joint Fusion with a Novel Posterior Sacroiliac Fusion Device: Diagnostic Approach, Surgical Technique, and Multicenter Case Series. J Pain Res 2022;15:1411-20. [Crossref] [PubMed]
- Whang PG, Darr E, Meyer SC, et al. Long-Term Prospective Clinical And Radiographic Outcomes After Minimally Invasive Lateral Transiliac Sacroiliac Joint Fusion Using Triangular Titanium Implants. Med Devices (Auckl) 2019;12:411-22. [Crossref] [PubMed]
- Sachs D, Capobianco R, Cher D, et al. One-year outcomes after minimally invasive sacroiliac joint fusion with a series of triangular implants: a multicenter, patient-level analysis. Med Devices (Auckl) 2014;7:299-304. [Crossref] [PubMed]
- Smith AG, Capobianco R, Cher D, et al. Open versus minimally invasive sacroiliac joint fusion: a multi-center comparison of perioperative measures and clinical outcomes. Ann Surg Innov Res 2013;7:14. [Crossref] [PubMed]



