
Prospective 5-year follow-up of L5–S1 versus L4–5 midline decompression and interspinous-interlaminar fixation as a stand-alone treatment for spinal stenosis compared with laminectomies
Highlight box
Key findings
• Spinal stenosis patients treated with InSpan IFD, used as a stand-alone treatment for interspinous-interlaminar fixation, at L4–5 and L5–S1 showed improved outcome scores and low complication and revision rates and were comparable to historical open laminectomy data.
• All surgeries were completed in less than one hour.
What is known and what is new?
• Insufficient published data exists regarding interspinous fixation devices at the L5–S1 level.
• Patients treated at L5–S1 with InSpan had significant improvement in pain and functional scores.
• Reoperation rate at five to ten years varied up to 24% for laminectomies.
• There was a total of one L4–5 revision (1.8%) and two L5–S1 revisions (4.4%).
What is the implication, and what should change now?
• Midline decompression and maintenance of distraction with InSpan is a successful substitute for laminectomies in selected patients.
Introduction
It is common to see magnetic resonance imaging (MRI) evidence of lumbar degenerative disc disease (DDD) in asymptomatic patients, but when patients have protracted symptoms of back pain and or neurogenic symptoms with MRI evidence of DDD and spinal stenosis, they are often treated first with physical therapy and medications. If this first-line treatment fails patients progress in treatment to repeated injections by pain management. If this fails, there is published evidence to support surgical decompression alone or coupled with placement of an interspinous device to distract the foramen and act as an extension block to prevent dynamic stenosis (1). L5–S1 is atypical in having the immobile sacrum adjacent which puts more stresses on implants and the S1 spinous process is often relatively smaller than the L5 spinous process. Furthermore, the canal at L5–S1 is larger than at L4–5 therefore, patients with symptomatic DDD and spinal stenosis at L5–S1 may not have typical MRI findings showing severe stenosis due to ligamentum flavum hypertrophy more easily seen at L4–5 and thus might not be offered interspinous process (ISP) devices until much more advanced MRI findings at which point patients may need laminectomies for decompression of the underlying spinal stenosis and instrumented fusion for fixation. For patients not yet deemed candidates for laminectomies or fusion, an alternative treatment emerged to treat mild to moderate stenosis in the lumbar spine, except for L5–S1, using unfixed ISP devices that act as dynamic extension blocks, such as Vertiflex Superion Interspinous Spacer (Boston Scientific Inc., Marlborough, MA, USA). Vertiflex has been demonstrated in clinical IDE studies to treat lumbar spinal stenosis (LSS) dynamically above L5–S1 to distract the foramen and limit extension, acting as an interspinous spacer (2). Dynamic extension block interspinous devices like Vertiflex and others such as X-Stop Interspinous Process Decompression System (Medtronic, Minneapolis, MN, USA) (3) and Coflex Interlaminar Stabilization device (Xtant Medical, Belgrade, MT, USA) (4), are not fixated to the spinous processes and therefore often fail by dislodgement, spinous process erosion, and fractures or loosening leading to continued symptoms (5-7). Interspinous fixation devices (IFD) emerged to provide greater fixation and are placed between the spinous processes as well as the lamina with teeth that bite into the spinous processes while there is a central hub to maintain distraction during extension such as the InSpan (InSpan LLC, Malden, MA, USA) (1,8) and Aspen (ZimVie, Westminster, CO, USA) (9,10). However, there is a paucity of literature for interspinous fixation devices at L5–S1 for symptomatic spinal stenosis and to our knowledge this is the first study to evaluate a fixated nondynamic extension block IFD at L5–S1 in an Ambulatory Surgery Center (ASC) setting with the added comparison to IFD at L4–5 and published laminectomy data.
Our objective was to test our hypothesis that we can achieve long-term successful outcomes in spinal stenosis patients treated with midline decompression and placement of a fixated IFD at L5–S1 versus L4–5 in an ASC comparable to open laminectomies. We present this article in accordance with the STROBE reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-23-49/rc).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Institutional Review Board (IRB) approval was granted for this study through Western Institutional Review Board (WIRB®) now known as WIRB-Copernicus Group (WCG® IRB) (WIRB#20181251) and informed consent was obtained from all individual participants. Data was kept on a HIPAA secured computer database. Data was inputted by medical personnel dedicated to research. We prospectively studied 100 consecutive patients from a single surgeon in a private academic practice. The patients underwent direct midline open decompression and hemilaminectomies followed by additional indirect decompression achieved by distraction of the lamina and spinous processes to open to foramen and canal using InSpan IFD, in the outpatient setting by a single board-certified orthopedic spine surgeon, for treatment of symptomatic degenerative spinal stenosis between the timeframe of September 2011 to October 2016. The inferior aspect of the footprint of the InSpan IFD (Figure 1) is contoured to the lamina allowing it to be placed flush against the lamina at the base of the spinous process and extends interlaminar. This advantage allows it to overcome the challenges of placing interspinous devices in spinous processes that are small or atypical, typically seen at S1. Patients were only considered for surgery after they were symptomatic for greater than four months and failed conservative management for at least three months that included physical therapy, nonsteroidal anti-inflammatory drugs (NSAID), chiropractic treatment, and epidural steroids. We prospectively collected Visual Analog Scores (VAS) and Oswestry Disability Index (ODI) data preoperatively and postoperatively follow-up to 5 years. Plain radiographs were done at the first postoperative visit and at the latest follow-up. Failure was determined as the need for a revision. Out of the 100 consecutive patients, 45 patients had surgery with placement of the InSpan IFD at L5–S1 and 55 patients at L4–5.

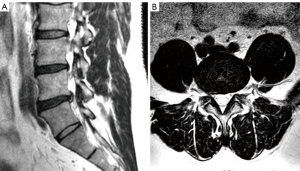
All patients had MRI evidence of mild to moderate central and/or foraminal spinal stenosis, disc desiccation, annular tear and confirmation of a spinous process height measuring at least 10 mm in order to fit the IFD’s smallest implant. Figure 2 is a preoperative MRI showing L5–S1 mild central and foraminal spinal stenosis, annular tear, anterior and posterior herniated disc, degenerative disc desiccation, degenerative facets plus facet tropism in a patient with low back pain and S1 radicular symptoms refractory to nonoperative treatment including steroid injections and medial branch blocks. Sagittal MRI view shows over 30% loss of disc height and mild grade 1 retrolisthesis. Figure 3 is a preoperative MRI with moderate right L4–5 foraminal spinal stenosis, annular tear and disc desiccation in a patient with right L4 radicular symptoms and back pain refractory to nonoperative treatment including steroid injections and medial branch blocks. Exclusion criteria for this study included acute severe trauma, fractures, malignancy, infection, unstable chronic medical illnesses, prior lumbar fusions, and a body mass index (BMI) >42 kg/m2 (11). All patients were assessed preoperatively, and narcotics were discontinued (12). Patients with chronic but stable medical conditions, including hypertension, diabetes mellitus, asthma, hypercholesterolemia, and heart disease were medically cleared by their family practitioner and/or cardiologist where applicable.

Summary of operative technique
The patient was placed in the prone position on the Wilson frame and underwent general endotracheal anesthesia. The Wilson frame was elevated to open the spinous processes. The operative level was confirmed using a 22-G spinal needle placed at the level of the transverse process (13) under AP and lateral intraoperative fluoroscopy. The spinous processes and laminas were exposed from a midline incision. Bilateral hemilaminectomies were performed with Kerrison Ronguers in the standard fashion to decompress the central canal and lateral recesses. The Wilson frame was returned to its natural position. The sizer was placed between the spinous processes and distracted to measure for an appropriate-sized IFD to open the foramen and spinal canal and unload the facets. The lumbar posterior ligamentous complex (PLC) was preserved. An intraoperative assessment for placement of IFD at the surgical level was made by fitting the footprint of the IFD against the spinous processes. Once confirmed, the appropriately sized InSpan device was placed deep to rest between the laminas and against the spinous processes with the teeth buried within the spinous processes (Figure 4). The set screws of the IFD implant were locked to ensure stability. Final AP and lateral fluoroscopy views were taken to confirm position and the wound was closed in layers. A standard outpatient postoperative protocol was followed to discharge patient after being deemed oriented and neurologically intact by the anesthesiologist, operating surgeon and nurse (14-16).
Statistical analysis
SPSS statistical software version 22 (IBM Corp, Armonk, New York, USA) was used to conduct statistical analysis. Intragroup comparisons of normally distributed variables were made using a paired t-test. For intergroup comparisons of non-normally distributed variables, the Mann-Whitney U test was used. The level of significance was set at P<0.05 for all assessed variables.
Results
A total of 100 consecutive patients having one level InSpan IFD instrumentation at L5–S1 or L4–5 was prospectively collected. At L5–S1, there was a total of 45 consecutive patients with a male and female population of 31 (68.89%) and 14 (31.11%). The mean patient age was 46.73 [standard deviation (SD) 8.99; 95% confidence interval (CI): 44.11, 49.36] and a median age of 45 years. The mean BMI was 30.19 (SD 5.41) kg/m2. The mean VAS preoperative and postoperative scores improved from 8.64 (SD 1.31) to 2.2 (SD 1.21), P<0.001. The mean ODI preoperative and postoperative scores improved from 39.36 (SD 10.86) to 14.73 (SD 4.61), P<0.001. The mean estimated blood loss (EBL) and surgeon time were 64 mL (SD 35) and 58 minutes (SD 17), respectively. We found 0% radiographic evidence of device-related failures. There were no instances of aborting the placement of the IFD at S1 due to atypical anatomy or a small spinous process (less than 10 mm). There were 2 (4.4%) revisions, one was an implant removal and revision hemilaminectomy decompression thought to be due to inadequate decompression and/or painful hardware. The second was converted to removal and fusion with pedicle screws (PS) and interbody polyetheretherketone (PEEK) cages.
There was a total of 55 InSpan IFD at L4–5 with a male and female population of 28 (50.91%) and 27 (49.09%). The mean age for the patients was 51.24 (SD 10.67; 95% CI: 48.42, 54.06) and a median age of 50. The mean BMI was 29.19 (SD 5.38) kg/m2. The mean VAS preoperative and postoperative scores improved from 8.9 (SD 1.55) to 1.74 (SD 1.46), P<0.001. The mean ODI preoperative and postoperative scores improved from 41.97 (SD 14.44) to 14.2 (SD 4.37), P<0.001. The mean EBL and surgical time were 40 mL (SD 15) and 45 minutes (SD 15) for L4–5. There was a total of 1 revision case (1.8%) with removal of the IFD and a revision open hemilaminectomy decompression.
There were no significant differences in the preoperative and postoperative ODI and preoperative VAS scores between the L5–S1 and L4–5 groups (P=0.501, P=0.637 and P=3.16), however, the VAS scores at 5-year postoperative at L4–5 was significantly less than at L5–S1 (P<0.01). There were no complications, no spinous process fractures, no spinous process erosion, no implant dislodgement, nor need for blood transfusions up to five-year follow-up. Figure 5 and Figure 6 show postoperative radiographs with the InSpan IFD in a stable position at L5–S1 and L4–5.


Mobbs et al. (17) reported improved preoperative and postoperative VAS and ODI scores with laminectomies (open and minimally invasive approach). Patients who underwent open laminectomy reported statistically significant improvement (P<0.05) in VAS and ODI scores of (7.9±1.4 to 3.9±2.9) and (46.6±18.9 to 17.8±15.4) respectively with a mean EBL of 110 mL (17). Long-term published laminectomy data for LSS showed reoperation rate at five to ten years varied up to 24% (18).
Discussion
Key findings
Our study aimed to demonstrate the safety and efficacy of InSpan IFD, used as a stand-alone treatment for interspinous-interlaminar fixation, after lumbar decompression without fusion at the L5–S1 level as we look at clinical outcomes, complications, and revision rates at five-year follow-up in patients with symptomatic degenerative spinal stenosis and compared the outcomes to L4–5 and historical open laminectomy data. The S1 spinous process is often small and can be quite challenging for placement of interspinous devices at L5–S1. We were able to demonstrate improved pain scores with decreasing clinical disability. There were no complications and no aborted surgeries due to small spinous process, no revision due to spinous process fracture or dislodgement. The InSpan IFD distracts deep to the base of the spinous processes and against the lamina thus increasing disc height as well as foraminal height without segmental kyphosis. Unlike unfixed interspinous spacers limited to blocking extension, decompression and stabilization using the InSpan IFD proved to be effective in avoiding full laminectomies and being able to block flexion and extension without loosening or spinal fractures thus treating symptoms due to foraminal stenosis on extension as well as decreasing the stresses on the facets and intervertebral discs due to painful motion. InSpan has not experienced any incidence of spinal fractures, device failures or dislodgement. Given the rigid sacrum, there might be concern with a higher incidence at L5–S1 of device or clinical failure where only the L5 lamina distracts while at L4–5 both the L4 and L5 laminas distract to open the foramen and spinal canal. We had no device-related failure in our study, but two patients required revisions at L5–S1 and one at L4–5 due to recurrent neurogenic symptoms. This was suggestive of inadequate decompression.
Strengths and limitations
The authors of this study recognize that there are limitations to the study design. Foremost, the results included in this analysis are comprised of the procedures and outcomes of a single surgeon. The patients were all symptomatic and failed nonoperative treatment, but the cohort studied was limited to mild to moderate radiographic spinal stenosis. It is the authors experience that spinal stenosis at L5–S1 where there is wider canal space does not present with severe stenosis on MRI images typically seen at higher levels such as L4–5 where you see classic hypertrophic ligamentum flavum and facets. However, a strength is that this is the first study to evaluate an IFD used as a stand-alone treatment for interspinous or interlaminar fixation at L5–S1 to treat L5–S1 degenerative spinal stenosis and could be a pilot for a multicenter study to add more patients to broaden the pool. The historically published open laminectomy data was not divided into L4–5 and L5–S1 groups for a more accurate comparison.
Comparison with similar research
ISP fixation for LSS has been shown to reduce the direct and indirect costs associated with LSS compared with extended periods of conservative treatment or laminectomies (19). Previous studies have also concluded that ISP devices have minimal operative risk of dura and nerve injuries, shortened operative time, and decreased intraoperative blood loss (20-22). Zhu et al. performed a systemic clinical and biomedical review of interspinous fusion devices and found that they can provide excellent biomechanical efficiency and promising clinical success (23). Kim et al. compared clinical outcome between the interspinous fusion devices and PS fixation and found significant evidence of a higher incidence of adjacent segmental degeneration (ASD) in the PS group than the interspinous devices (24). Lee et al. studied a group of 26 patients (1:1 ratio of interspinous fusion devices and PS) and demonstrated that interspinous fusion devices can be used as an alternative to PS fixation (25). Concerns that ISP might lead to kyphosis by spine surgeons have also limited the adoption. A study by Schulte et al. reviewed postoperative radiographs and concluded that interspinous distraction does not seem to be detrimental to sagittal balance, and may improve it (26). This study evaluated the X-Stop device (Medtronic) which is a nonfixation ISP that acts as an extension block. These nonfixation devices are prone to revisions approximating 19% in two years in one study by Borg et al. (27). In patients with degenerative spondylolisthesis treated with X-Stop the failure rate defined as reintervention for surgery was 54% and so nonfixed ISP is not recommended for degenerative spondylolisthesis (28). Bowers et al. reported X-Stop complication rate of 38% and 85% ultimate failure rate requiring additional spinal surgery (29). In another study of a nonfixed ISP, BacJac (Surgalign, Deerfield, IL, USA) interspinous device, the authors demonstrated favorable early outcome measures however, long-term results showed only 41% of patients with a satisfactory result (30). Cumulative data have proven, nonfixed ISP devices have the potential for early effectiveness in treating spinal stenosis but long-term outcomes remain uncertain, primarily due to the recurring symptoms observed by two years (31). The X-Stop device was withdrawn from the market for Orthopedics and Neurosurgeons by Medtronic, while Vertiflex failed to gain traction among spine surgeons so targeted Interventional Pain Management specialists eager to treat spinal stenosis with a seemingly minimally invasive and low-risk device.
Explanations of findings
Interspinous fixation devices have been studied to show advantages over transpedicular screw fixation such as reduced postoperative back pain from less lateral muscle dissection, short operative time, and reduced cephalad ASD (20). ISP devices placed between the spinous process can increase the central canal area up to 18%, the foraminal area by 25% and the foraminal width by 43% in cadaveric spine studies (32). ISPs were approved for patient use for over a century (32) and the evolution to new designs have resulted in IFD devices that are contoured to be lamina and provide extension block in addition to fixation of the spinous processes and stabilization of the facets. These novel IFD devices such as InSpan in this study are designed to provide relief for patients suffering from LSS worse on extension but also who have back pain from degenerative disc and facets and who may have facet tropism due to difference in angulation of the facets on either side (33). Nonfixed ISP devices, when evaluated on routine biplanar radiographic evaluation, have reported 1–5.8% fractures due to relative structural weakness of the spinous process (5). Spinous process fractures and erosions have been shown to occur with dynamic fixation with X-Stop and interspinous fixation with Aspen due to degenerative spondylolisthesis and with weak evidence due to osteoporosis (34). In our study there were no spinous process erosions or fractures. InSpan has a unique design different from X-Stop and Aspen which allows for deep positioning of the device between the interlaminar space and has a relatively large footplate with tall, staggered spikes or teeth that interdigitates to provide strong fixation within the spinous processes to result in excellent stability (Figure 1B). Nonfixed ISP devices such as X-Stop and Vertiflex were designed with a central hub and “wing” projections to limit lateral expulsion but were not designed to prevent posterior expulsion. This design also posed risks for spinous process erosions and fractures due to their lack of fixation as they are 100% load bearing. In contrast, IFD devices like InSpan were designed with spiked or teethed plates for load sharing by dissipating the forces through the teeth and plates rather than solely relying on the central hub. The teethed plates are held securely together by two top loading set screws that are embedded in the plate and can tightened or loosened. When tightened and locked, they create a strong fixation with the principle that a greater force would be required to separate the plates. This secure fixation aided in preventing expulsion in all six planes of motion, spinous process erosions and fractures. To revise InSpan, the two set screws are loosened to disengage the teethed plates. The ZIP (Aurora Spine, Carlsbad, CA, USA) and Minuteman (Spinal Simplicity, Overland Park, KS, USA) are two IFD designs that lack top loading set screws, making revision more difficult.
Implications and actions needed
According to a study conducted by Lurie et al. (35) in 2016, lumbar stenosis affects more than 200,000 adults in the USA alone, with this number rising each year (11). The increasingly aging population in the USA has resulted in a greater proportion of elderly patients, coinciding with a rise in lumbar stenosis. The 2010 U.S. Census Bureau has reported that the fastest growing age groups are 45 to 64 (31.5%) and 62 and older (21.1%) (36). As life expectancy increases and the “baby boomer” generation reaches late adulthood, associated comorbidities rise, as well. DDD in the spine along with degeneration of other major joints are the common offenders of chronic musculoskeletal conditions (37). Increasingly, patients over 60 are continuing to work, travel, and remain physically active, but are often plagued by lower back pain and sciatica due to degenerative spine diseases such as stenosis and disc and facet degeneration. The high prevalence of LSS seen in this age group results in massive numbers of patient visits to healthcare facilities, as individuals seek available treatment options for their pain—both surgical and nonsurgical (38). Lumbar stenosis has been identified as the most common reason for spinal surgery in patients over 65 (11).
Traditionally, once a patient has failed conservative measures, they may consider a surgical approach. This may be in the form of lumbar decompression alone or in combination with instrumentation for spinal fusion consisting of removal of the intervertebral disc, placement of interbody cages and posterior PS and rods. There are known complications of these traditional lumbar surgeries using PS and interbodies such as dural tears, spinal cord injury depending on level, malposition, and pedicle fracture (39,40). There is a growing movement towards less invasive spinal surgeries that can be safely done in an outpatient setting with greater efficiency, faster recovery, less blood loss, less risk, and less cost. The IFD satisfies the above criteria if performed in the appropriately selected patient. IFD is used for less exposure spine surgery (LESS) resulting in less exposure of the spine, less muscle dissection, less radiation, less blood loss, less time, less complication, less radiation, less postoperative recovery time and pain and thus less need for hospitalization. Abbas et al. published their study showing that patients with facet tropism (L3 to S1) have approximately a 2.9 times increased risk of developing LSS (41). However, there is lack of evidence to show efficacy of IFD at L5–S1 and there is doubt in its application due to the unusual anatomy such as the immobile sacrum which provides greater stresses on the L5–S1 disc and the usually shorter S1 spinous process in some patients providing less space to fix an IFD implant.
Decompressive hemilaminectomies or full laminectomies can provide relief from opening of the neural canal both the central canal and the foramen by removal of the ligamentum flavum, obstructive facet osteophytes and herniated discs. This approach is limited in only removing static compression as many patients also have dynamic compression in extension with radicular symptoms described as a positive Kemp sign (42) mostly due to foraminal stenosis. Full laminectomies risk hematoma formation, dural tears and massive dural scaring leading to symptomatic tethering of the dura and nerves. Full laminectomies also lead to hypermobility of the segment leading to facet and disc degeneration and risks symptomatic post laminectomy kyphosis. Some previous studies on the lasting effects of lumbar decompression for patients that present with spinal stenosis demonstrate deterioration of the neural space (21,22). This deterioration leads to instability, which will often require a future surgical procedure with instrumented fusion to provide stability. A 2016 study on laminectomy plus fusion versus laminectomy alone for lumbar spondylolisthesis stated that within 4 years, approximately one-third of all patients in their study that had undergone a laminectomy required reoperation. The reoperation rate was 34% in the cohort of patients who received laminectomy, and this was based on clinical instability (43).
Conclusions
Our study demonstrates long-term successful outcomes of the InSpan IFD, used as a stand-alone treatment for interspinous-interlaminar fixation, at L5–S1 for symptomatic degenerative spinal stenosis similar to at L4–5 and published data for open laminectomies. InSpan demonstrated revision rates of 4.4% at L5–S1 and 1.8% at L4–5 compared to nonfixed ISP devices, such as X-Stop, which exhibited an 85% ultimate failure rate requiring additional spinal surgery. There were no device-related failures in our study, but two patients required revisions at L5–S1 and one at L4–5 due to recurrent neurogenic symptoms suggestive of inadequate decompression. To reduce the risks of needing revision surgery, we recommend adequate distraction decompression of the foramen with a large enough sized IFD to show an opened foramen greater than seen on preoperative lateral radiographs and comparable to adjacent foramen sizes. All InSpan surgeries at L4–5 and L5–S1 were completed in less than one hour. There were no complications, spinous process fractures, spinous process erosion, implant dislodgement or the need for blood transfusions.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-23-49/rc
Data Sharing Statement: Available at https://jss.amegroups.com/article/view/10.21037/jss-23-49/dss
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-23-49/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-23-49/coif). K.R.C. reports that he is the cofounder and CEO of KIC (Kingsley Investment Company) Ventures and has ownership shares in the company. J.A.S. and K.R.C. are members of Less Exposure Surgery Specialists (LESS) Institute, a for-profit single surgeon private clinical practice. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Western Institutional Review Board (WIRB®) now known as WIRB-Copernicus Group (WCG® IRB) (WIRB#20181251) and informed consent was obtained from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chin KR, Pencle FJR, Benny A, et al. Greater than 5-year follow-up of outpatient L4-L5 lumbar interspinous fixation for degenerative spinal stenosis using the INSPAN device. J Spine Surg 2020;6:549-54. [Crossref] [PubMed]
- Nunley PD, Patel VV, Orndorff DG, et al. Five-year durability of stand-alone interspinous process decompression for lumbar spinal stenosis. Clin Interv Aging 2017;12:1409-17. [Crossref] [PubMed]
- Nielsen M. X-STOP surgical implant for the treatment of lumbar spinal stenosis: clinical practice recommendations for neurosurgical nurse practitioners. J Neurosci Nurs 2013;45:44-51. [Crossref] [PubMed]
- Li AM, Li X, Yang Z. Decompression and coflex interlaminar stabilisation compared with conventional surgical procedures for lumbar spinal stenosis: A systematic review and meta-analysis. Int J Surg 2017;40:60-7. [Crossref] [PubMed]
- Kim DH, Tantorski M, Shaw J, et al. Occult spinous process fractures associated with interspinous process spacers. Spine (Phila Pa 1976) 2011;36:E1080-5. [Crossref] [PubMed]
- Gazzeri R, Galarza M, Neroni M, et al. Failure rates and complications of interspinous process decompression devices: a European multicenter study. Neurosurg Focus 2015;39:E14. [Crossref] [PubMed]
- Zhong J, O'Connell B, Balouch E, et al. Patient Outcomes After Single-level Coflex Interspinous Implants Versus Single-level Laminectomy. Spine (Phila Pa 1976) 2021;46:893-900. [Crossref] [PubMed]
- Raikar SV, Patil AA, Pandey DK, et al. Inter Spinal Fixation and Stabilization Device for Lumbar Radiculopathy and Back Pain. Cureus 2021;13:e19956. [Crossref] [PubMed]
- Karahalios DG, Kaibara T, Porter RW, et al. Biomechanics of a lumbar interspinous anchor with anterior lumbar interbody fusion. J Neurosurg Spine 2010;12:372-80. [Crossref] [PubMed]
- Postacchini F, Postacchini R, Menchetti PP, et al. Lumbar Interspinous Process Fixation and Fusion with Stand-Alone Interlaminar Lumbar Instrumented Fusion Implant in Patients with Degenerative Spondylolisthesis Undergoing Decompression for Spinal Stenosis. Asian Spine J 2016;10:27-37. [Crossref] [PubMed]
- Chin KR, Coombs AV, Seale JA. Feasibility and patient-reported outcomes after outpatient single-level instrumented posterior lumbar interbody fusion in a surgery center: preliminary results in 16 patients. Spine (Phila Pa 1976) 2015;40:E36-42. [Crossref] [PubMed]
- Lawrence JT, London N, Bohlman HH, et al. Preoperative narcotic use as a predictor of clinical outcome: results following anterior cervical arthrodesis. Spine (Phila Pa 1976) 2008;33:2074-8. [Crossref] [PubMed]
- Chin KR, Pencle FJR, Kubik J, et al. Avoidance of Wrong Level Surgery in the Lumbar Spine: A Technical Report. J Spine 2015;4:257.
- Chin KR, Pencle FJ, Coombs AV, et al. Lateral Lumbar Interbody Fusion in Ambulatory Surgery Centers: Patient Selection and Outcome Measures Compared With an Inhospital Cohort. Spine (Phila Pa 1976) 2016;41:686-92. [Crossref] [PubMed]
- Chin KR, Pencle FJR, Coombs AV, et al. Clinical Outcomes With Midline Cortical Bone Trajectory Pedicle Screws Versus Traditional Pedicle Screws in Moving Lumbar Fusions From Hospitals to Outpatient Surgery Centers. Clin Spine Surg 2017;30:E791-7. [Crossref] [PubMed]
- Chin KR, Pencle FJR, Coombs AV, et al. Eligibility of Outpatient Spine Surgery Candidates in a Single Private Practice. Clin Spine Surg 2017;30:E1352-8. [Crossref] [PubMed]
- Mobbs RJ, Li J, Sivabalan P, et al. Outcomes after decompressive laminectomy for lumbar spinal stenosis: comparison between minimally invasive unilateral laminectomy for bilateral decompression and open laminectomy: clinical article. J Neurosurg Spine 2014;21:179-86. [Crossref] [PubMed]
- Sajadi K, Azarhomayoun A, Jazayeri SB, et al. Long-Term Outcomes of Laminectomy in Lumbar Spinal Stenosis: A Systematic Review and Meta-Analysis. Asian J Neurosurg 2022;17:141-55. [Crossref] [PubMed]
- Cairns K, Deer T, Sayed D, et al. Cost-effectiveness and Safety of Interspinous Process Decompression (Superion). Pain Med 2019;20:S2-8. [Crossref] [PubMed]
- Chen MH, Chen JY. A Novel Nonpedicular Screw-Based Fixation in Lumbar Spondylolisthesis. Biomed Res Int 2017;2017:5619350. [Crossref] [PubMed]
- Genevay S, Atlas SJ. Lumbar spinal stenosis. Best Pract Res Clin Rheumatol 2010;24:253-65. [Crossref] [PubMed]
- Munakomi S, Foris LA, Varacallo M. Spinal Stenosis and Neurogenic Claudication. Treasure Island (FL): StatPearls Publishing; 2023.
- Zhu L, Yin J. Interspinous fusion device: A systematic review of clinical and biomechanical evidence. Advances in Mechanical Engineering 2016; [Crossref]
- Kim HJ, Bak KH, Chun HJ, et al. Posterior interspinous fusion device for one-level fusion in degenerative lumbar spine disease: comparison with pedicle screw fixation - preliminary report of at least one year follow up. J Korean Neurosurg Soc 2012;52:359-64. [Crossref] [PubMed]
- Lee CH, Hyun SJ, Kim KJ, et al. Can the Interspinous Device, SPIRE(TM), be an Alternative Fixation Modality in Posterior Lumbar Fusion Instead of Pedicle Screw? Turk Neurosurg 2017;27:408-13. [Crossref] [PubMed]
- Schulte LM, O'Brien JR, Matteini LE, et al. Change in sagittal balance with placement of an interspinous spacer. Spine (Phila Pa 1976) 2011;36:E1302-5. [Crossref] [PubMed]
- Borg A, Hill CS, Nurboja B, et al. A randomized controlled trial of the X-Stop interspinous distractor device versus laminectomy for lumbar spinal stenosis with 2-year quality-of-life and cost-effectiveness outcomes. J Neurosurg Spine 2021;34:544-52. [Crossref] [PubMed]
- Verhoof OJ, Bron JL, Wapstra FH, et al. High failure rate of the interspinous distraction device (X-Stop) for the treatment of lumbar spinal stenosis caused by degenerative spondylolisthesis. Eur Spine J 2008;17:188-92. [Crossref] [PubMed]
- Bowers C, Amini A, Dailey AT, et al. Dynamic interspinous process stabilization: review of complications associated with the X-Stop device. Neurosurg Focus 2010;28:E8. [Crossref] [PubMed]
- Spallone A, Lavorato L, Belvisi D. Long-term Results for the BacJac Interspinous Device in Lumbar Spine Degenerative Disease. J Neurol Surg A Cent Eur Neurosurg 2019;80:3-7. [Crossref] [PubMed]
- Pintauro M, Duffy A, Vahedi P, et al. Interspinous implants: are the new implants better than the last generation? A review. Curr Rev Musculoskelet Med 2017;10:189-98. [Crossref] [PubMed]
- Richards JC, Majumdar S, Lindsey DP, et al. The treatment mechanism of an interspinous process implant for lumbar neurogenic intermittent claudication. Spine (Phila Pa 1976) 2005;30:744-9. [Crossref] [PubMed]
- Boden SD, Riew KD, Yamaguchi K, et al. Orientation of the lumbar facet joints: association with degenerative disc disease. J Bone Joint Surg Am 1996;78:403-11. [Crossref] [PubMed]
- Kim DH, Shanti N, Tantorski ME, et al. Association between degenerative spondylolisthesis and spinous process fracture after interspinous process spacer surgery. Spine J 2012;12:466-72. [Crossref] [PubMed]
- Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ 2016;352:h6234. [Crossref] [PubMed]
- Jackson RP, McManus AC, Moore J. Lumbar spinal stenosis: treatment options for an aging population. Mo Med 2012;109:466-9.
- Rustenburg CME, Emanuel KS, Peeters M, et al. Osteoarthritis and intervertebral disc degeneration: Quite different, quite similar. JOR Spine 2018;1:e1033. [Crossref] [PubMed]
- Suri P, Rainville J, Kalichman L, et al. Does this older adult with lower extremity pain have the clinical syndrome of lumbar spinal stenosis? JAMA 2010;304:2628-36. [Crossref] [PubMed]
- Lonstein JE, Denis F, Perra JH, et al. Complications associated with pedicle screws. J Bone Joint Surg Am 1999;81:1519-28. [Crossref] [PubMed]
- Nottmeier EW, Seemer W, Young PM. Placement of thoracolumbar pedicle screws using three-dimensional image guidance: experience in a large patient cohort. J Neurosurg Spine 2009;10:33-9. [Crossref] [PubMed]
- Abbas J, Peled N, Hershkovitz I, et al. Facet Tropism and Orientation: Risk Factors for Degenerative Lumbar Spinal Stenosis. Biomed Res Int 2020;2020:2453503. [Crossref] [PubMed]
- Orita S, Inage K, Eguchi Y, et al. Lumbar foraminal stenosis, the hidden stenosis including at L5/S1. Eur J Orthop Surg Traumatol 2016;26:685-93. [Crossref] [PubMed]
- Ghogawala Z, Dziura J, Butler WE, et al. Laminectomy plus Fusion versus Laminectomy Alone for Lumbar Spondylolisthesis. N Engl J Med 2016;374:1424-34. [Crossref] [PubMed]



