
Successful non-operative treatment of traumatic atlanto-occipital dislocation: a case report
Highlight box
Key findings
• Non-operative treatment of atlanto-occipital dislocation (AOD) was done with a successful radiographic and neurological recovery.
What is known and what is new?
• We know the standard of care for these injuries is operative cranio-cervical stabilization. This report suggests, however, that non-operative care may be possible for some patients.
What is the implication, and what should change now?
• Non-operative treatment of AOD is possible. However, we still advocate for operative stabilization as the standard of care for these injuries.
Introduction
Traumatic atlanto-occipital dislocation (AOD) is a rare but life-threatening injury, usually caused by high energy injury mechanisms. The range of neurologic injury can be from neurologically intact to instant fatality. Typically, these injuries are managed operatively in the form of fusion from the skull to upper cervical spine. If internal fixation is unable to be performed then a halo device is usually a secondary option to stabilize the upper cervical spine. We present a unique case of a patient who sustained an AOD and atlanto-axial dissociation (AAD) that was treated non-operatively in a hard collar alone. Reports of successful non-operative treatment of this injury pattern are rare and may fill in current voids in the literature regarding the treatment of this injury. We present this case in accordance with the CARE reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-23-60/rc).
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Verbal informed consent was obtained from the patient for publication of this case report and accompanying images. Every effort was made to contact the patient in person for written consent, but the patient lives several hundred miles away from our institution.
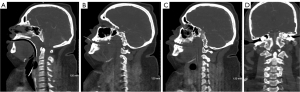
An 18-year-old male was involved in a high-speed motor vehicle accident. The patient had a Glasgow coma scale (GCS) score of 3 and was intubated by first responders. He initially presented to an outside community hospital, and trauma evaluation revealed an AOD with associated bilateral occipital condyle fractures, AAD, subarachnoid hemorrhage, subdural hemorrhage of the cervical spine, a right-sided scalp laceration and hematoma, an open right lower extremity wound, and a coccyx fracture. His physical exam at that time revealed an American Spinal cord Injury Association (ASIA) B spinal cord injury with no sensation on the right side of the body but some sensation on the left side and intact cranial nerves II–XII. Imaging with computed tomography (CT) of his cervical spine showed significant diastasis of the occiput-C1 articulations with bilateral alar ligament avulsion fractures off of the occipital condyles, and diastasis at the C1-2 articulations (Figure 1).
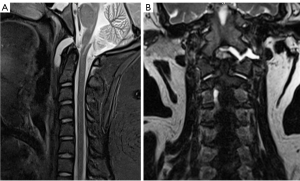
He was transferred to an outside academic hospital for admission to an intensive care unit and higher level of care. It was noted that his GCS had improved to 10T after transfer. The spine surgery team evaluated him for surgery but elected to treat his injury non-operatively since the risks of surgery were deemed to outweigh the benefits, as the patient was significantly obese weighing 540 pounds. The spine team cited need for weight loss and nutritional optimization as reasons for delaying surgery. He remained in a Miami J collar during his admission. A magnetic resonance imaging (MRI) study of the cervical spine obtained a week after his injury confirmed alar ligament injury and bilateral atlantooccipital joint diastasis, as well as a spinal cord signal changes at the level of C1-2 (Figure 2). He remained hospitalized for 53 days. A tracheostomy and percutaneous endoscopic gastrostomy (PEG) tube were placed. His neurological exam remained unchanged for 4 weeks after the injury. After 4 weeks he began to regain some motion on the left side of his body. He discharged to a rehabilitation center specializing in spinal cord injuries, and remained in a Miami J collar while there. A repeat CT scan obtained at the rehabilitation center 3 months after his injury showed less joint diastasis compared to his initial imaging but unhealed alar ligament avulsion fractures. He had developed some interval evidence of radiographic healing by that time.
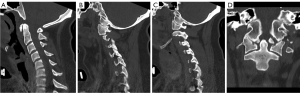
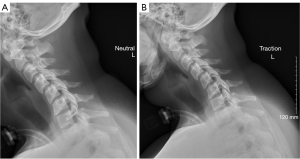
He then presented to our clinic for a surgical consultation 6 months after his injury. On our evaluation of him, he weighed 383 pounds. He had some posterior cervical pain consistent with muscular pain. He was using an electric wheelchair. His neurological exam showed inability to hold his left arm above his head but otherwise had 5/5 strength in the left biceps, triceps, wrist extensors, wrist flexors, and finger abduction. He could shrug the right shoulder but otherwise had 2/5 strength throughout the right upper extremity. His had 1/5 strength in the right quadriceps and 4/5 with the left, and 4/5 with right tibialis anterior and 5/5 with the left. He had decreased sensation in the right upper and lower extremities, and normal sensation in the left upper and lower extremities. The right hand he held in a closed fisted position with increased tone. A repeat CT scan 6 months after injury showed improved alignment of the occiput-C1 interval with healing across the bilateral atlantooccipital joints (Figure 3). We performed assisted flexion and extension radiographs as well as a manual traction stress radiograph (Figure 4). These demonstrated no gapping in the occiput-C1 or C1-2 junctions. We thus elected to continue non-operative treatment and began weaning him out of the hard cervical collar for two hours a day.
At 8 months after injury, a telephone interview was performed and the patient reported some persistent but stable muscular pain in his posterior cervical area but no neurological change. Anteroposterior (AP) and lateral radiographs were reviewed remotely which were stable compared to the radiographs obtained at 6 months after injury. At that point we recommended continued physical therapy and soft collar wear as needed for comfort.
At 17 months after his injury, another telephone interview was conducted with the patient and his family. Full strength and sensation of the left arm and leg were reported at that time. His right arm was able to be used for certain activities but is noticeably weaker than his left; his right leg requires assistance for movement. He does not wear a cervical collar and denied significant neck pain. He is able to use a walker with some assistance but primarily uses an electric wheelchair.
Patient perspective
The patient and his parents are surprised with his outcome. Overall, given his degree of injury, the amount of function he has seems shocking although he still does have some neurologic deficits. The patient and his family are adapting to normal life with the use of multiple assistive devices. They are hopeful that progress continues to be made with intensive therapy regarding his strength. The main limitation that seems to be his focus on recovery is his mobility.
Discussion
The stability of the craniocervical junction (CCJ) is conferred by both bony and ligamentous structures. Most of the stability of the CCJ is afforded by the intrinsic ligaments about the CCJ which include the tectorial membrane, cruciate ligament, and alar ligaments (1).
Neurologic deficits from AOD can range from normal neurological exam which is found in up to 20% of patients, to instant fatality (2,3). Initial screening lateral cervical radiograph is an acceptable first-line test, although more frequently cervical spine CT is the first imaging test done of the cervical spine. Harris et al. studied the lateral radiographs of 400 adults and defined normal radiographic atlantooccipital relationships (4). The basion-axis interval is defined as the distance from the basion to the rostral projection of the posterior cortex of the body of C1. The basion-dens interval (BDI) is defined as the distance between the basion and the rostral tip of the dens. Both of these parameters should normally be 12 mm or less on plain radiographs. Newer data suggests using a cutoff of 8.5 mm for the BDI when using CT scan for measurement (5). Martinez-Del-Campo et al. in a study using CT found that the average condyle-C1 interval (CCI) in adult patients without AOD was 0.89±0.12 mm, while the average CCI in adult patients with AOD was 3.35±0.18 mm. This group recommended a revised CCI and condylar sum cutoff for the diagnosis of AOD in the adult population (1.5 and 3.0 mm, respectively) (6). Other radiographic measurements to assist in diagnosis of AOD include the Power’s ratio and X-line method (7). Dziurzynski et al. studied the diagnostic usefulness of the Harris lines, Power’s ratio, X-line method, and condylar gap measured on both lateral radiographs and CT scan. They found greater sensitivity, specificity, and positive and negative predictive values for AOD when measuring these values on CT scan (8).
Nonoperative treatment of AOD has been associated with poorer outcomes in prior studies. Up to 50% of patients have been reported to get worse with non-operative management alone (9,10). The existing literature related to non-operative treatment of AOD is limited to a handful of case reports and case series (11-14). Halo vest immobilization was used in one adult patient as successful treatment in a case report published by Kaplan et al. (13). Horn et al. published a retrospective review of 33 patients with AOD, five of which were treated non-operatively in an external orthosis (15). The patients that were chosen for non-operative treatment in this series had no or “questionable” abnormalities on CT scan but had abnormalities on MRI of the atlantooccipital ligaments. Davis et al. reported successful treatment of AOD with a hard cervical collar alone in a patient with concomitant atlantooccipital association (14). They theorized that given there was a fracture that afforded bony healing, no evidence of ligamentous injury, and the patient had a normal neurological exam, successful non-operative treatment would be appropriate.
As described earlier, the primary mechanism of failure in AOD is ligamentous failure which makes the injury highly unstable without rigid internal fixation. Modern internal fixation techniques include pedicle screw and plate-rod systems (16,17). These internal fixation techniques have improved outcomes in patients with AOD (9,16,17). Overall outcomes following AOD depend on multiple factors, however, including presenting neurological deficits, associated injuries (in particular associated head injuries and cardiothoracic injuries), and timeliness to diagnosis. Mendenhall et al. reported a 26% 90-day mortality rate in their series of AOD. The strongest predictor for mortality was a missed diagnosis of AOD (18). Significant predictors of neurological improvement in this series included younger age, lower Glasgow coma score, worse initial ASIA spinal cord injury severity, and lower Injury Severity Score. Joaquim et al. published a systematic review of AOD and reported a 34.8% mortality rate, although they noted that this figure is likely higher as some studies excluded non-survivors from analysis (19). Filiberto et al. attempted to identify modifiable risk factors for poor outcomes following traumatic AOD in a series of 52 patients (20). GCS score on admission was identified as an independent risk factor for mortality following traumatic AOD. This group also noted that patients who were transported alive to a hospital and survived their other injuries were more likely to have a good outcome.
Our patient had a unique presentation in that he had gross abnormalities on his initial imaging, initially was found to have a GCS of 3, and had neurological abnormalities on exam yet was successfully treated with non-operative treatment. His radiologic parameters of AOD and his neurological exam improved with immobilization in a hard cervical external orthosis. Protective factors that he had include young age, incomplete spinal cord injury, and no delay in diagnosis.
Another factor that likely contributed to his successful outcome was the fact that his injuries consisted of bony avulsion fractures off of the occipital condyles which may have allowed favorable bone to bone healing. The nature of our patient’s injury was such that instead of purely ligamentous disruption across the atlanto-occipital joints (which would mandate surgical stabilization), he had bilateral Anderson and Montesano type III occipital condyle fractures which involve avulsions of the condyles related to the attachments of the alar ligaments. Allowing gravity reduction of these avulsion fractures in a collar likely played a key role in his successful outcome with non-operative management. A halo vest would not have provided this gravity assisted settling of the avulsion fractures and thus the appropriate non-operative treatment plan for this patient, regardless of his weight, would consist of a collar. With regard to the AAD component of his injury, the dorsal displacement and avulsion mechanism of the AOD likely contributed to his normal ADI and successful healing at the AA joint. If this patient had ventral displacement of the CCJ, he may not have had as favorable an outcome regarding the AAD as the articulations of C1-2 would likely be more disrupted.
Conclusions
While operative stabilization is still considered the standard of care for AOD and AAD, non-operative treatment may be feasible in a patient who is too unstable or unfit to undergo an operation. We presented here one such case of a patient with an unstable traumatic AOD who was managed in a hard cervical collar alone. A key to his successful treatment outcome is likely related to the bony involvement of his injury consisting of avulsion fractures of occipital condyles that were favorable for treatment in a collar alone.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-23-60/rc
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-23-60/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-23-60/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Verbal informed consent was obtained from the patient for publication of this case report and accompanying images. Every effort was made to contact the patient in person for written consent, but the patient lives several hundred miles away from our institution.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bransford RJ, Alton TB, Patel AR, et al. Upper cervical spine trauma. J Am Acad Orthop Surg 2014;22:718-29. [Crossref] [PubMed]
- Kim JW. Atlanto-Occipital Dislocation: A Case Report. Korean J Neurotrauma 2019;15:55-60. [Crossref] [PubMed]
- Munoz-Mahamud E, Combalia A, Bori G. Traumatic atlanto-occipital dislocation: a case report. J Orthop Surg (Hong Kong) 2012;20:391-4. [Crossref] [PubMed]
- Harris JH Jr, Carson GC, Wagner LK. Radiologic diagnosis of traumatic occipitovertebral dissociation: Normal occipitovertebral relationships on lateral radiographs of supine subjects. AJR Am J Roentgenol 1994;162:881-6. [Crossref] [PubMed]
- Rojas CA, Bertozzi JC, Martinez CR, et al. Reassessment of the craniocervical junction: normal values on CT. AJNR Am J Neuroradiol 2007;28:1819-23. [Crossref] [PubMed]
- Martinez-Del-Campo E, Kalb S, Soriano-Baron H, et al. Computed tomography parameters for atlantooccipital dislocation in adult patients: the occipital condyle-C1 interval. J Neurosurg Spine 2016;24:535-45. [Crossref] [PubMed]
- Lee C, Woodring JH, Goldstein SJ, et al. Evaluation of traumatic atlantooccipital dislocations. AJNR Am J Neuroradiol 1987;8:19-26.
- Dziurzynski K, Anderson PA, Bean DB, et al. A blinded assessment of radiographic criteria for atlanto-occipital dislocation. Spine (Phila Pa 1976) 2005;30:1427-32. [Crossref] [PubMed]
- Kasliwal MK, Fontes RB, Traynelis VC. Occipitocervical dissociation-incidence, evaluation, and treatment. Curr Rev Musculoskelet Med 2016;9:247-54. [Crossref] [PubMed]
- Theodore N, Aarabi B, Dhall SS, et al. The diagnosis and management of traumatic atlanto-occipital dislocation injuries. Neurosurgery 2013;72:114-26. [Crossref] [PubMed]
- Govender S, Vlok GJ, Fisher-Jeffes N, et al. Traumatic dislocation of the atlanto-occipital joint. J Bone Joint Surg Br 2003;85:875-8.
- Ghatan S, Newell DW, Grady MS, et al. Severe posttraumatic craniocervical instability in the very young patient. Report of three cases. J Neurosurg 2004;101:102-7. [Crossref] [PubMed]
- Kaplan NB, Molinari C, Molinari RW. Nonoperative Management of Craniocervical Ligamentous Distraction Injury: Literature Review. Global Spine J 2015;5:505-12. [Crossref] [PubMed]
- Davis JR, Kluckman ML, Mallory GW, et al. Successful non-operative management for atlanto-occipital dislocation resulting in spinal cord contusion in a patient with atlanto-occipital assimilation and severe Chiari I malformation. Surg Neurol Int 2020;11:338. [Crossref] [PubMed]
- Horn EM, Feiz-Erfan I, Lekovic GP, et al. Survivors of occipitoatlantal dislocation injuries: imaging and clinical correlates. J Neurosurg Spine 2007;6:113-20. [Crossref] [PubMed]
- Garrido BJ, Puschak TJ, Anderson PA, et al. Occipitocervical fusion using contoured rods and medial offset connectors: description of a new technique. Orthopedics 2009;32: [Crossref] [PubMed]
- Abumi K, Takada T, Shono Y, et al. Posterior occipitocervical reconstruction using cervical pedicle screws and plate-rod systems. Spine (Phila Pa 1976) 1999;24:1425-34. [Crossref] [PubMed]
- Mendenhall SK, Sivaganesan A, Mistry A, et al. Traumatic atlantooccipital dislocation: comprehensive assessment of mortality, neurologic improvement, and patient-reported outcomes at a Level 1 trauma center over 15 years. Spine J 2015;15:2385-95. [Crossref] [PubMed]
- Joaquim AF, Schroeder GD, Vaccaro AR. Traumatic Atlanto-Occipital Dislocation-A Comprehensive Analysis of All Case Series Found in the Spinal Trauma Literature. Int J Spine Surg 2021;15:724-39. [Crossref] [PubMed]
- Filiberto DM, Sharpe JP, Croce MA, et al. Traumatic atlanto-occipital dissociation: No longer a death sentence. Surgery 2018;164:500-3. [Crossref] [PubMed]


