
Minimizing neurovascular complications during image-guided percutaneous cryoablation of a cervical spinal aneurysmal bone cyst using protective doxycycline sclerotherapy: a case report
Highlight box
Key findings
• Using image-guided percutaneous doxycycline sclerotherapy (DS) to dissect and treat the portion closest to neurovascular structures plus image-guided percutaneous cryoablation (CYOA) for the remainder of the lesion of an aneurysmal bone cyst (ABC) within the vertebral body of C5 allowed for effective, safe treatment after recurrence with CYOA alone.
What is known and what is new?
• Minimally invasive image-guided techniques, including CYOA and DS, are increasingly being used to treat ABCs, especially cases not amenable to surgical curettage.
• The combined use of DS and CYOA for the treatment of ABC is reported. However, the use of adjunctive DS as a protective agent and treatment of lesion portions near neurovascular structures during treatment of ABC with CYOA is not documented.
What is the implication, and what should change now?
• DS could be used safely and effectively as a dissection agent and adjunctive therapy to CYOA in the treatment of ABCs in close relationship to critical neurovascular structures.
Introduction
Aneurysmal bone cysts (ABCs) are rare (0.14/1 million), benign, and locally aggressive bone tumors mostly found in pediatric patients (1). Although typical locations of ABCs are the metaphyses of long bones, they may also appear in the cervical spine (1). Surgical curettage has been considered the standard treatment for ABCs (2). However, it poses a particularly challenging task in the cervical spine due to its potential impact on the structural stability of the neck and proximity to crucial neurovascular structures. Minimally invasive procedures, including transarterial embolization (TAE), image-guided percutaneous cryoablation (CYOA) and image-guided percutaneous doxycycline sclerotherapy (DS), have shown to be viable options in the treatment of ABCs when surgery is not possible (3,4). This case report describes a successful treatment with combined CYOA and DS of a symptomatic cervical spinal C5 ABC encompassing the right vertebral artery (RVA) and in close contact with critical nervous structures in a 4-year-old patient not amenable to surgery or TAE. DS was used as a complementary therapy and as an additional layer of protection for critical neurovascular structures during treatment. We present this case in accordance with the CARE reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-23-147/rc).
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent for publication of this case report and accompanying images was obtained from the patient’s parents.
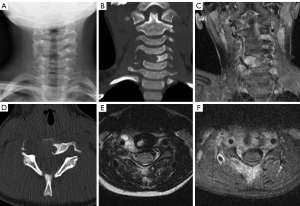
A 4-year-old male and his parents were referred to our center in February 2020, complaining of a right lateral cervical mass that had progressively increased in size, associated with limiting pain and right-hand movement impairment. Imaging work-up reported a 20-mm expansive bone tumor located on the right lateral aspect of the C5 vertebral body with extension into the pedicle. It completely encompassed the RVA, partially occupied the right C5–C6 intervertebral foramen and extended into the spinal canal. Findings were highly suggestive of an ABC (Figure 1). After multidisciplinary discussion, surgical curettage was deemed unsuitable due to the challenging anatomical location. Treatment with TAE was initially considered but disregarded after a diagnostic angiography showed the lesion feeding vessels originating directly from the RVA, which entailed a high risk of iatrogenic posterior fossa and spinal cord ischemia (Figure 2A). Finally, treatment with CYOA was proposed.
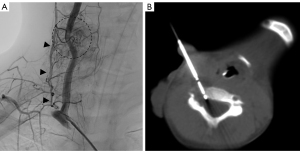
The procedure was performed in a biplane angio-suite under general anesthesia and neurophysiological monitoring. First, cone-beam computed tomography (CBCT) was performed for procedural planning. Next, a 14-G coaxial access was placed inside the lesion using live 3D needle guidance software (XperGuide; Koninklijke Philips N.V., Amsterdam, The Netherlands), and a histopathological sample was taken. Intraoperative analysis of the sample confirmed a primary ABC. Subsequently, an IceSphere1.5CXTM (Boston Scientific, Marlborough, USA) CYOA needle was placed through the coaxial system into the lesion, performing two freezing and two thawing cycles of 10 minutes each (Figure 2B). The patient presented initial symptom improvement after the first follow-up. However, clinical recurrence and incomplete ossification on imaging follow-up were observed six months after treatment. Therefore, it was decided to conduct a second CYOA session. This second procedure used the same approach and material described in the first session. However, the decision was made to use DS as a dissection agent and as adjuvant therapy in the portion of the lesion in intimate relation with critical neurovascular structures. Three mL of a 100 mg/5 mL solution of doxycycline was used before CYOA at the edge and inside that portion of the lesion, allowing a more aggressive and complete CYOA procedure which was carried out during the same procedure. The patient remained under observation and was discharged the following day without adverse events.
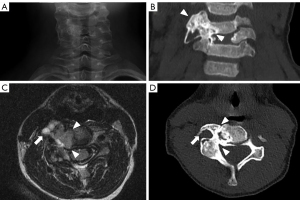
Subsequent clinical follow-ups at 3, 10 and 21 months after the second round of CYOA revealed complete resolution of pain symptoms, restoration of cervical mobility and unrestricted hand movement. Moreover, the imaging revealed almost total sclerosis of the ABC, with only a small remnant in the transverse process, which did not justify further treatment (Figure 3).
Discussion
Surgical treatment of symptomatic ABCs is complex in the cervical spine and especially problematic in pediatric patients, considering their musculoskeletal system is still developing (5,6). An alternative investigational treatment involves the administration of concentrated autologous bone marrow injections, which have shown promising outcomes for these lesions (7). Image-guided minimally invasive techniques, including DS and CYOA, have been successfully used independently or combined to treat ABCs. Published case series have demonstrated a good safety profile with low recurrence rates (3,8). These techniques have also proven especially useful in anatomically complex locations in the pediatric population (3,9).
CYOA involves delivering cycles of extreme cold and thawing through a cryoprobe, which induces osmotic imbalance, leading to cellular rupture and, ultimately, tumor destruction. Doxycycline is an antibiotic with antitumor properties that stimulate bone growth and has been proven to be a promising agent for ABCs sclerotherapy (8). The combination of both techniques may be effective in the treatment of ABCs. A recently published case series demonstrated a 10% recurrence rate and a 7.7% complication rate in patients treated with percutaneous ablation, DS, or a combination of both. This study also observed that patients treated with CYOA required fewer sessions than those treated solely with DS (3). In this case, not only was DS used as a complementary therapy to CYOA, but it was also used as a protective agent to shield the neurovascular structures in close contact with the lesion. This allowed for a safer and more effective treatment.
This case report describes a symptomatic, inoperable, and non-embolizable ABC in the cervical spine correctly treated with CYOA and complementary protective DS after a failed first CYOA session in a pediatric patient. Therapeutic management of this case was especially challenging. Surgery and TAE were ruled out due to the complex location of the lesion and the irrigation of the lesion by the RVA, respectively. CYOA was primarily preferred over DS due to the possibility of reducing the number of sessions. After the first CYOA session resulted in recurrence six months after treatment, a different approach was adopted for the second intervention. A single needle puncture was used to administer doxycycline both within the tumor and the edge immediately adjacent to the spinal cord, C5–C6 nerve roots and RVA. By doing so, this targeted DS conditioned partial sclerosis at the level of this critical portion of the lesion while adding a layer of protection for crucial neurovascular structures. This subsequently allowed a safer CYOA to be performed to treat the remaining ABC. After treatment, an almost complete imaging response and a total disappearance of symptomatology were reported up to 3 years after treatment. Inducing sclerosis in the portion of the lesion proximal to the spinal cord with DS proved to be a valuable adjunct to CYOA and also proved to be a beneficial protective agent that allowed us to be more aggressive with CYOA cycles.
Conclusions
DS might prove useful as a complementary and protective agent to CYOA during the treatment of a cervical ABC located next to critical neurovascular structures. Nevertheless, this experience is limited to our case and further evidence is needed.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-23-147/rc
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-23-147/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-23-147/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent for publication of this case report and accompanying images was obtained from the patient’s parents.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cottalorda J, Bourelle S. Modern concepts of primary aneurysmal bone cyst. Arch Orthop Trauma Surg 2007;127:105-14. [Crossref] [PubMed]
- Mankin HJ, Hornicek FJ, Ortiz-Cruz E, et al. Aneurysmal bone cyst: a review of 150 patients. J Clin Oncol 2005;23:6756-62. [Crossref] [PubMed]
- Arleo TL, Hawkins CM, Fabregas JA, et al. Percutaneous image-guided treatment of aneurysmal bone cysts: is there a superior treatment option? Pediatr Radiol 2022;52:1539-49. [Crossref] [PubMed]
- Masthoff M, Gerwing M, Schneider KN, et al. Combined Transarterial Embolization and Percutaneous Sclerotherapy as Treatment for Refractory and Nonresectable Aneurysmal Bone Cysts. J Vasc Interv Radiol 2021;32:1425-1434.e2. [Crossref] [PubMed]
- Park HY, Yang SK, Sheppard WL, et al. Current management of aneurysmal bone cysts. Curr Rev Musculoskelet Med 2016;9:435-44. [Crossref] [PubMed]
- Restrepo R, Zahrah D, Pelaez L, et al. Update on aneurysmal bone cyst: pathophysiology, histology, imaging and treatment. Pediatr Radiol 2022;52:1601-14. [Crossref] [PubMed]
- Barbanti-Brodano G, Girolami M, Ghermandi R, et al. Aneurysmal bone cyst of the spine treated by concentrated bone marrow: clinical cases and review of the literature. Eur Spine J 2017;26:158-66. [Crossref] [PubMed]
- Wong MN, Braswell LE, Murakami JW. Doxycycline sclerotherapy of cervical spine aneurysmal bone cysts: single-institution 13-year experience. Pediatr Radiol 2022;52:1528-38. [Crossref] [PubMed]
- Bavan L, Wijendra A, Kothari A. Efficacy of treatment interventions for primary aneurysmal bone cysts: a systematic review. Bone Jt Open 2021;2:125-33. [Crossref] [PubMed]


