
A case report of lobular intradural extramedullary capillary hemangioma in a 14-year-old patient: resection and reconstruction
Highlight box
Key findings
• Prompt recognition and treatment of intradural hemangiomas is recommended due to the risk of hemorrhage.
What is known and what is new?
• Intradural hemangiomas are benign, potentially curable tumors.
• Pediatric cases are extremely rare.
What is the implication, and what should change now?
• Laminoplasty allows for reconstruction of the spinal column and return of normal anatomy/function.
• Anatomic normalization is a special consideration for pediatric patients.
Introduction
Intradural extramedullary capillary hemangiomas of the cauda equina are exceedingly rare malformations arising from the endothelial cells of the nervous system vasculature (1). These are benign tumors owing their pathologic propensity to mass effect leading to pain and neurologic deficits. Only 20 cases have been previously reported in the literature, with the sole pediatric case being in a 17-year-old patient (1-4). Here we report a case of an intradural, extramedullary capillary hemangioma of the cauda equina in a 14-year-old patient. We present this article in accordance with the CARE reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-23-113/rc).
Case presentation
Preoperative presentation
A 14-year-old female with no known chronic medical problems presented with a two-month history of worsening low back pain and bilateral leg pain into the entirety of her feet. She also noted slight weakness of her lower extremities that excluded her from prior athletic activities. She reported no bowel or bladder incontinence. Physical examination revealed decreased sensation to her bilateral lower extremities to soft touch and painful stimulation, throughout the entirety of her lower extremity sensory dermatomes being more pronounced on her right side. Objectively, her strength was normal 5/5 in all muscle groups. She had diminished but present patellar and achilles reflexes.
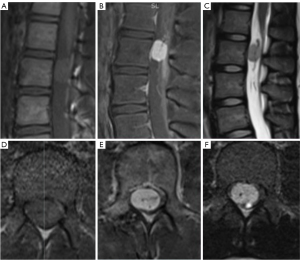
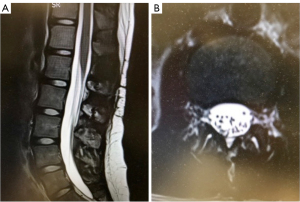
Magnetic resonance imaging (MRI) revealed a well-defined homogenous gadolinium-enhancing intradural, extramedullary mass centered at L2 causing severe spinal canal stenosis and posterior displacement of the spinal nerve roots. There was also a T2 flow void, indicating vascularity of the lesion (Figure 1).
Operative technique
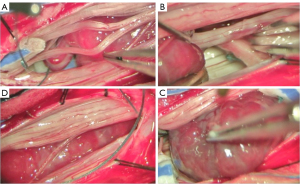
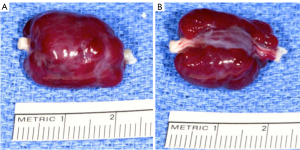
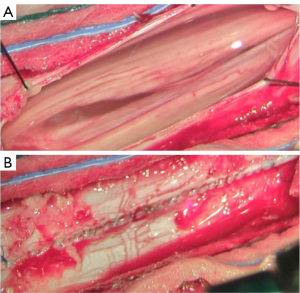
The patient underwent L1–2 laminoplasty for resection of intradural tumor. Bilateral troughs were drilled along the lamina of L1 and L2 and the L1 and L2 lamina/spinous process complex was removed in one piece. The dura was opened along the midline and a classically described mud-brown/purplish mass was visualized arising from a single, thickened nerve root (Figure 2). There was also a feeding vessel that was identified and coagulated during the dissection. Intraoperative electrophysiological monitoring was employed. The entering and exiting roots from the mass were stimulated up to 1.5 mA with only a very weak anal sphincter response. Surrounding nerve roots were stimulated briskly at 0.5 mA. The decision was made to amputate this nerve root above and below the tumor in order to remove the mass en bloc. After careful arachnoid dissection, the tumor was removed in one piece (Figure 3). In general, hemostasis was not difficult to achieve despite the vascular nature of the lesion, most likely due to the coagulation of the feeding vessel prior. The nerve roots were completely decompressed after removal and the dura was closed primarily with Prolene suture (Figure 4). The L1 and L2 lamina were fixated in their original position with cranial mini plates and screws and the supraspinous ligament was reapproximated with 0 vicryl suture.
Postoperative follow-up
Postoperatively, the patient awoke with no deficits and resolved leg pain. A 3-month postoperative MRI revealed no tumor recurrence and fully healed lamina (Figure 5). She was cleared to resume competitive sports.
Case pathology
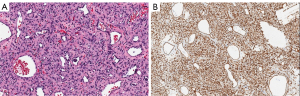
On lower magnification, sections demonstrate a cellular proliferation of small cells forming small vascular structures with scattered larger vessels and areas of peri-vascular edema as well as scattered areas of erythrocytes. On higher magnification, the neoplasm is composed of a cellular proliferation of round to spindled cells with minimal pleomorphism with no significant mitoses or apoptotic bodies seen. Further staining demonstrated strong CD34 positivity (Figure 6). All these findings are consistent with capillary hemangioma.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent for publication of this case report and accompanying images was unable to be obtained from the patient or guardians after all possible attempts were made on several occasions. The patient information provided in this report is written to ensure anonymity. Likewise, the accompanying visuals, such as MRI scans, pathology slides, and close up intraoperative photos, are devoid of any identifying characteristics.
Discussion
Only 21 cases of intradural extramedullary capillary hemangiomas of the cauda equina have been reported, including our own (1). When considering the entire spine, approximately 40 total cases of these tumors have been reported (2,3). Additionally, our case is just the second pediatric instance to be described. Although the natural history of these lesions is largely unknown due to rarity, early diagnosis and treatment upon recognition has been recommended due to risk of hemorrhage leading to neurological decline (3-5).
Capillary hemangiomas are typically described on MRI as isointense on T1-weighted images, hyperintense on T2-weighted images, and homogenously enhancing on post-contrast imaging, similar to our case. When occurring in the central nervous system (CNS), these tumors are usually well defined intradural extramedullary lesions (6). The differential diagnosis for masses with these radiographic characteristics includes meningiomas most commonly, as well as capillary hemangiomas, metastatic lesions, lymphomas, paragangliomas, and ependymomas. Other vascular pathologies should also be included in the differential such as cavernous hemangiomas, hemangioblastomas, and angiomyolipoas (3,6).
Patients typically present with symptoms of other compressive lesions, including back pain, lower limb pain and numbness, lower limb weakness, and paresthesias that are typically progressive over time (1,4-8), however, there have been reports of acute onset of symptoms due to bleeding of a capillary hemangioma (3). The most common age range for patients is between 40 and 60 years (7). Due to the risk of rupturing that could cause acute neurologic decline, total resection, if possible, is treatment of choice (1,4-8). Total resection also decreases the likelihood of recurrence necessitating further surgery. At this time there is no role for radiation.
This entity has never previously been described in a patient as young as fourteen. Prompt recognition and complete surgical excision allowed for complete recovery and return to all activities with no need for further interventions in our patient. The only other described pediatric patient with this entity was a 17-year-old male who presented similarly without objective weakness but with leg pain and a similar appearing MRI. Total excision allowed for a complete neurologic recovery in this patient as well; however, a laminoplasty was not performed (8).
The use of laminoplasty is of particular interest as it allows for reconstruction of the posterior spinal elements and return of normal anatomy. Additionally, such as in our case, the end result is complete regrowth of the bony lamina and healing of the soft tissues, practically returning the patient to her preoperative state without the tumor. In our review only one other case applied this technique to an adult patient (9). Further in the pediatric population, laminoplasty was found to be associated with decreased rate of progressive spinal deformity requiring surgical correction (10).
Conclusions
The youngest case of intradural extramedullary capillary hemangioma of the cauda equina is reported. Given the benign nature, the operative goal is complete excision of the tumor without damage to neural structures. Postoperatively the goal is relief of pain and improvement in neurologic function. Reconstruction of the surgical site in a manner that returns the patient’s normal anatomy should be considered especially in younger patients.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-23-113/rc
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-23-113/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-23-113/coif). C.G. serves as an unpaid Associate Editor of Journal of Spine Surgery from November 2022 to October 2024. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent for publication of this case report and accompanying images was unable to be obtained from the patient or guardians after all possible attempts were made on several occasions. The patient information provided in this report is written to ensure anonymity. Likewise, the accompanying visuals, such as MRI scans, pathology slides, and close up intraoperative photos, are devoid of any identifying characteristics.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hughes LP, Largoza G, Montenegro TS, et al. Intradural extramedullary capillary hemangioma of the cauda equina: case report of a rare spinal tumor. Spinal Cord Ser Cases 2021;7:21.
- Bouali S, Maatar N, Bouhoula A, et al. Intradural Extramedullary Capillary Hemangioma in the Upper Cervical Spine: First Report. World Neurosurg 2016;92:587.e1-7. [Crossref] [PubMed]
- Panero I, Eiriz C, Lagares A, et al. Intradural-Extramedullary Capillary Hemangioma with Acute Bleeding: Case Report and Literature Review. World Neurosurg 2017;108:988.e7-988.e14. [Crossref] [PubMed]
- Liu JJ, Lee DJ, Jin LW, et al. Intradural extramedullary capillary hemangioma of the cauda equina: Case report and literature review. Surg Neurol Int 2015;6:S127-31. [Crossref] [PubMed]
- Unnithan AK, Joseph TP, Gautam A, et al. Case report of lumbar intradural capillary hemangioma. Surg Neurol Int 2016;7:S139-41. [Crossref] [PubMed]
- Shin JH, Lee HK, Jeon SR, et al. Spinal intradural capillary hemangioma: MR findings. AJNR Am J Neuroradiol 2000;21:954-6.
- Zhao Z, Zheng J, Zhou Y. Intradural extramedullary capillary hemangioma with intramedullary component: A case series. Medicine (Baltimore) 2022;101:e29862. [Crossref] [PubMed]
- Ganapathy S, Kleiner LI, Mirkin LD, et al. Intradural capillary hemangioma of the cauda equina. Pediatr Radiol 2008;38:1235-8. [Crossref] [PubMed]
- Chung SK, Nam TK, Park SW, et al. Capillary hemangioma of the thoracic spinal cord. J Korean Neurosurg Soc 2010;48:272-5. [Crossref] [PubMed]
- McGirt MJ, Chaichana KL, Atiba A, et al. Incidence of spinal deformity after resection of intramedullary spinal cord tumors in children who underwent laminectomy compared with laminoplasty. J Neurosurg Pediatr 2008;1:57-62. [Crossref] [PubMed]


