
Analysis of antibiotic regimens and outcomes in spinal brucellosis: insights from a retrospective cohort study in Makkah, Saudi Arabia
Highlight box
Key findings
• Triple-antibiotic therapy had a cure rate of 100% among spinal brucellosis patients, except in the combination of streptomycin + doxycycline + rifampicin antibiotic regimen (75%).
• Extending the duration of antibiotics in patients with abscesses may obviate the need for surgical intervention.
What is known and what is new?
• There is no consensus on the optimal antibiotic regimens for spinal brucellosis and data are limited.
• This study aims to compare antibiotic treatment regimens for spinal brucellosis and evaluate their efficacy.
What is the implication, and what should change now?
• No difference in overall cure rate was observed between the triple- and dual-antibiotic regimens. In addition, prolonging the antibiotic duration showed good clinical outcomes in patients requiring surgical intervention.
• Further studies are now needed to identify the optimal antibiotic regimen.
Introduction
Brucellosis is an endemic zoonotic disease with a global reach and is considered a major health problem worldwide. It is also known as Mediterranean fever, Malta fever, Gibraltar fever, and undulant fever. Brucellosis is caused by various species, leading to damage in multiple organs with a protean presentation (1,2). In several regions, such as the Mediterranean basin, Mexico, South and Central America, Eastern Europe, Asia, Africa, the Caribbean, and the Arabian Peninsula, brucellosis is considered an endemic disease. Its incidence rate varies depending on demographic, occupational, and socioeconomic factors. For example, in many brucellosis-endemic countries, weak health-care systems, poor surveillance systems, and passively acquired official data are likely to underestimate the true burden of this disease. Hence, high-quality studies are needed to accurately estimate the true incidence of the disease (3,4).
According to the Statistical Yearbook released in 2019 by the Saudi National Registry of the Ministry of Health, the incidence rate among Saudis was 13.41/100,000 compared with 18.1/100,000 among non-Saudis. This difference could be explained by the fact that non-Saudis are more likely to work as shepherds (5). Some countries have an annual global incidence rate of more than 10 per 100,000 of their population affected. Although the infection rate in Saudi Arabia has been decreasing over time, it remains higher than in other countries (3-5).
Brucellosis patients can be asymptomatic due to various factors, while symptoms may vary based on the infected organs. The primary symptom is an undulating fever accompanied by fatigue, sweating, malaise, anorexia, and arthralgia. The infection mainly targets the musculoskeletal and reticuloendothelial organs (1,2). Osteoarticular manifestations are observed in 10–85% of patients, with spondylitis and spondylodiscitis being the most frequent complications (also known as spinal brucellosis). Previous studies indicate that the lumbar region is the most affected (60–69%), followed by the thoracic region (19%) and cervical region (6–12%) (6). Serious complications with spinal brucellosis are associated with abscess formation (7).
The most common complaint in spondylodiscitis is back pain, and patients may also present with fever, sweating, lymphadenopathy, and hepatosplenomegaly. However, the clinical symptoms are variable and non-specific, making diagnosing challenging. Therefore, in endemic areas, Brucellar spondylitis should be considered in the differential diagnoses of patients with long-term back pain (6). According to Ulu-Kilic et al., a triple-antibiotic regimen is recommended for a prolonged duration in complicated cases (8). Nevertheless, the exact antibiotic regimen, course duration, and the need for surgical intervention remain controversial (4). The presence of an abscess may alter the management plan, as suggested by Kaptan et al., who conclude that patients with Brucella spondylitis accompanied by an abscess may require a longer course of treatment and even surgical intervention (7).
Currently, data on the optimal antibiotic regimens for spinal brucellosis are limited, and the findings are mixed. Therefore, this study aims to compare antibiotic treatment regimens for spinal brucellosis at our center and evaluate their efficacy. We present this article in accordance with the STROBE reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-23-104/rc).
Methods
Using a convenience sampling technique, we included all patients of all age groups and both sexes over an 11-year period from 2010 to 2021, who were diagnosed with brucellosis based on polymerase chain reaction (PCR) with a titer of 2-mercaptoethanol (2-ME) ≥1:80 in the presence of clinical signs and symptoms compatible with brucellosis and had magnetic resonance imaging (MRI) findings suggestive of spinal brucellosis (spondylitis or spondylodiscitis). Patients were excluded due to poor file documentation, duplicated records or lost to follow-up. This retrospective cohort study was conducted at Al-Noor Specialist Hospital in Makkah City, Saudi Arabia, and was approved by the Ethics Committee of the Ministry of Health (No. H-02-K076-1221-624). It is noteworthy that Al-Noor Specialist Hospital, being a governmental facility overseen by the Ministry of Health. Consequently, researchers intending to conduct studies within the hospital premises are compelled to seek ethical approval directly from the Ministry of Health, adhering to its regulatory protocols and guidelines. Informed consent was taken from all the patients. Additionally, the study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
The authors have collected information regarding the following clinical presentation: low back pain, fever, lower or upper limb weakness, vomiting, neck pain, headache, myalgia, cough, and shortness of breath. Various therapy regimens were used, including gentamicin + doxycycline + ciprofloxacin (GDC), streptomycin + rifampicin + ciprofloxacin (SRC), streptomycin + doxycycline + rifampicin (SDR), streptomycin + rifampicin + trimethoprim/sulfamethoxazole (SRT), gentamicin + trimethoprim/sulfamethoxazole + ciprofloxacin (GTC), streptomycin + doxycycline + trimethoprim/sulfamethoxazole (SDT), streptomycin + trimethoprim/sulfamethoxazole + ciprofloxacin (STC), doxycycline + streptomycin (DS), and streptomycin + rifampicin (SR) (Table 1).
Table 1
| Regimen of therapy | Combination of antibiotics | Dosage and duration of therapy |
|---|---|---|
| GDC | Gentamicin + doxycycline + ciprofloxacin | 5 mg/kg OD (7 d) + 100 mg po BID + 750 mg po BID |
| SRC | Streptomycin + rifampicin + ciprofloxacin | 1 g IV/IM OD (21 d) + 600–900 mg po q24h + 750 mg po BID |
| SDR | Streptomycin + doxycycline + rifampicin | 1 g IV/IM OD (21 d) + 100 mg po BID + 600–900 mg po q24h |
| SRT | Streptomycin + rifampicin + trimethoprim/sulfamethoxazole | 1 g IV/IM OD (21 d) + 600–900 mg po q24h + 5 mg/kg (TMP component) po q12h |
| GTC | Gentamicin + trimethoprim/sulfamethoxazole + ciprofloxacin | 5 mg/kg OD (7 d) + 5 mg/kg po q12h + 750 mg po BID |
| SDT | Streptomycin + doxycycline + trimethoprim/sulfamethoxazole | 1 g IV/IM OD (21 d) + 100 mg po BID + 5 mg/kg po q12h |
| STC | Streptomycin + trimethoprim/sulfamethoxazole + ciprofloxacin | 1 g IV/IM OD (21 d) + 5 mg/kg po q12h + 750 mg po BID |
| DS | Doxycycline + streptomycin | 100 mg po BID + 1 g IV/IM OD (21 d) |
| SR | Streptomycin + rifampicin | 1 g IV/IM OD (21 d) + 600–900 mg po q24h |
OD, once daily; d, day; po, per oral; BID, twice a day; IV, intravenous; IM, intramuscular; q24h, every 24 h; TMP, trimethoprim; q12h, every 12 h.
Patients were excluded if the duration of the received antibiotic regimen or follow-up was poorly documented (Figure 1). We retrieved records for each case, including clinical manifestations and treatment outcomes until the last follow-up. We also contacted all patients to confirm their final status (cured or treatment failure), including those who were lost to follow-up in the second or third appointment. Patients were considered cured if they showed complete improvement in clinical symptoms and signs after completing the treatment duration. Patients who received all the prescribed treatment pills but missed the third follow-up were also considered cured. Therapeutic failure was considered if the patient required a second-line regimen due to persistent signs and symptoms after completing the duration of the first-line regimen. Additionally, due to information bias, relapse status was considered a therapeutic failure. The surgical indications for this study included severe neurological deficits, abscess collection compressing the spinal cord, and failure of medical treatment.
Statistical analysis
Data analysis was conducted using RStudio (R version 4.1.1). Categorical variables were presented as frequencies and percentages, while numerical variables were summarized using the median and interquartile range (IQR). The approach to handling missing data was done by analysis and directly applying methods unaffected by the missing values. The administered medications and first-line regimens were visualized through stacked column bars.
Results
General characteristics of the included patients
A total of 35 patients were included and analyzed in the current study (Figure 1). Most were male (77.1%) and Saudi nationals (94.3%). Two patients were non-Saudis; one was Yemeni, and the other was Malian. The median (IQR) age of the patients was 58.0 (48.0 to 63.0) years, and the median (IQR) duration of admission was 14.0 (6.5 to 22.0) days, whereas only one missing value was observed. The most common comorbidities were diabetes mellitus (44.4%) and hypertension (22.9%) (Table 2). The most frequently reported symptoms upon admission included low back pain (83.3%), fever (44.4%), and lower limb weakness (19.4%) (Figure 2).
Table 2
| Parameters | Values |
|---|---|
| Age (years), median (IQR) | 58.0 (48.0, 63.0) |
| Sex, n (%) | |
| Female | 8 (22.9) |
| Male | 27 (77.1) |
| Nationality, n (%) | |
| Non-Saudi | 2 (5.7) |
| Saudi | 33 (94.3) |
| Comorbidities, n (%) | |
| DM | 16 (44.4) |
| HTN | 8 (22.9) |
| Smoking history | 0 (0.0) |
| CKD | 1 (2.9) |
| Dyslipidemia | 1 (2.9) |
| Asthma | 1 (2.9) |
| HIV | 0 (0.0) |
| Osteoarthritis | 1 (2.9) |
| Hypothyroidism | 1 (2.9) |
| Hospitalization period (days)†, median (IQR) | 14.0 (6.5, 22.0) |
| Diagnostic test positivity, n (%) | |
| Brucella PCR | 35 (100.0) |
| Brucella culture | 2 (5.7) |
| Type of Brucella species on PCR, n (%) | |
| B. melitensis | 1 (2.9) |
| B. abortus | 1 (2.9) |
| Both | 33 (94.3) |
†, the variable had one missing value. IQR, interquartile range; DM, diabetes mellitus; HTN, hypertension; CKD, chronic kidney disease; HIV, human immunodeficiency virus; PCR, polymerase chain reaction; B. melitensis, Brucella melitensis; B. abortus, Brucella abortus.
Regarding radiological characteristics, spondylodiscitis was the most commonly observed pathology (77%). The lumbar vertebrae were the most frequently involved vertebral level, followed by the lumbosacral vertebrae. Five patients were associated with epidural abscess, and one had a paravertebral abscess (Table 3).
Table 3
| Vertebral level affected | Total† | Paravertebral abscess, 1 (3%) |
Epidural abscess, 5 (14%) |
Spondylitis, 8 (23%) |
Spondylodiscitis, 27 (77%) |
|---|---|---|---|---|---|
| Lumbar | 23 | ||||
| L1–L2 | 3 | – | – | 1 | 2 |
| L2–L3 | 5 | – | 1 | 1 | 4 |
| L3–L4 | 5 | – | 1 | 1 | 4 |
| L4–L5 | 10 | 1 | 2 | – | 10 |
| Lumbo-sacral | 6 | ||||
| L5–S1 | 6 | – | – | 2 | 4 |
| Thoracic | 3 | ||||
| T5–T6 | 1 | – | – | – | 1 |
| T9–T10 | 1 | – | – | – | 1 |
| T10–T11 | 1 | – | – | – | 1 |
| Cervical | 3 | ||||
| C1–C2 | 1 | – | – | 1 | – |
| C4–C5 | 1 | – | – | 1 | – |
| C3–C6 | 1 | – | 1 | 1 | – |
Data are presented as numbers. †, the “total” column represents the total number of patients affected at each vertebral level (individual patients may have more than one type of spinal condition concurrently). MRI, magnetic resonance imaging.
Characteristics of the first-line regimen therapy
Figure 3 demonstrates the distribution of eight types of first-line regimen therapies prescribed to the patients. The most frequently administered regimen was the combination of SDR (20 patients, 55.6%), followed by the combination of SRT (eight patients, 22.2%). The duration of medication use for all regimens ranged from 1 to 8 months. Regimen therapy failure was observed in five patients who received SDR (25%) and one patient who received a combination of SDT (50%). Overall, out of the total 35 patients who received first-line treatment, only six patients experienced therapy failure (Table 4).
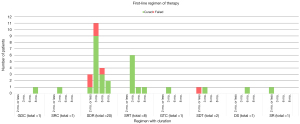
Table 4
| Regimen of therapy | No. of cases | Duration of therapy less than 3 months |
Duration of therapy for 3 months |
Duration of therapy for 6 months |
Duration of therapy for 8 months |
Overall cure rate | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | Cure rate | All | Cure rate | All | Cure rate | All | Cure rate | ||||||
| GDC | 1 | 0 (0.0) | – | 0 (0.0) | – | 0 (0.0) | – | 1 (100.0) | 1 (100.0) | 1 (100.0) | |||
| SRC | 1 | 0 (0.0) | – | 1 (100.0) | 1 (100.0) | 0 (0.0) | – | 0 (0.0) | – | 1 (100.0) | |||
| SDR | 20 | 3 (15.0) | 1 (33.3) | 11 (55.0) | 9 (81.8) | 4 (20.0) | 3 (75.0) | 2 (10.0) | 2 (100.0) | 15 (75.0) | |||
| SRT | 8 | 0 (0.0) | – | 6 (75.0) | 6 (100.0) | 1 (12.5) | 1 (100.0) | 1 (12.5) | 1 (100.0) | 8 (100.0) | |||
| GTC | 1 | 0 (0.0) | – | 1 (100.0) | 1 (100.0) | 0 (0.0) | – | 0 (0.0) | – | 1 (100.0) | |||
| SDT | 2 | 1 (50.0) | 0 (0.0) | 1 (50.0) | 1 (100.0) | 0 (0.0) | – | 0 (0.0) | – | 1 (50.0) | |||
| DS | 1 | 0 (0.0) | – | 0 (0.0) | – | 1 (100.0) | 1 (100.0) | 0 (0.0) | – | 1 (100.0) | |||
| SR | 1 | 1 (100.0) | 1 (100.0) | 0 (0.0) | – | 0 (0.0) | – | 0 (0.0) | – | 1 (100.0) | |||
Data are presented as number or number (%). GDC, gentamicin + doxycycline + ciprofloxacin; SRC, streptomycin + rifampicin + ciprofloxacin; SDR, streptomycin + doxycycline + rifampicin; SRT, streptomycin + rifampicin + trimethoprim/sulfamethoxazole; GTC, gentamicin + trimethoprim/sulfamethoxazole + ciprofloxacin; SDT, streptomycin + doxycycline + trimethoprim/sulfamethoxazole; DS, doxycycline + streptomycin; SR, streptomycin + rifampicin.
Characteristics of second-line regimen therapy and outcomes
Out of the total six patients who experienced first-line treatment failure with SDR (five patients, 83%) and SDT (one patient, 17%), surgery was indicated for three patients. The duration of drug administration ranged from 3 to 6 months, with only one patient receiving treatment for less than 3 months. The overall cure rate was found to be 75% among patients who received SRT. Additionally, a 100% cure rate was observed among two patients who were treated with STC, as well as SDT (Table 5).
Table 5
| 2nd line regimen of therapy | No. of cases | Case | The replaced, 1st regimen |
Duration of therapy for the 2nd line regimen | Outcome | Overall cure rate, n (%) | Surgery is indicated | Underwent surgical intervention |
|---|---|---|---|---|---|---|---|---|
| SRT | 4 | 1 | SDR (<3 months) | 3 months | Cure | 3 (75.0) | Yes | Yes |
| 2 | SDR (3 months) | 3 months | Cure | Yes | No | |||
| 3 | SDR (3 months) | 3 months | Cure | No | – | |||
| 4 | SDR (6 months) | 6 months | Failure | Yes | No | |||
| STC | 1 | 5 | SDT | 3 months | Cure | 1 (100.0) | No | – |
| SDT | 1 | 6 | SDR (<3 months) | Less than 3 months | Cure | 1 (100.0) | No | – |
SRT, streptomycin + rifampicin + trimethoprim/sulfamethoxazole; SDR, streptomycin + doxycycline + rifampicin; STC, streptomycin + trimethoprim/sulfamethoxazole + ciprofloxacin; SDT, streptomycin + doxycycline + trimethoprim/sulfamethoxazole.
Characteristics of patients who underwent surgical intervention
Surgical intervention was deemed necessary in 12 patients (34%) due to compressing abscess collection, severe neurological deficits, or treatment failure. Among these, three patients underwent anterior cervical discectomy and fusion (ACDF), while two patients underwent posterior lumbar decompression and fusion (PLDF), and dorsal spine decompression was performed in two other patients. Three patients chose not to undergo surgical intervention but still showed complete improvement upon completing the treatment duration. One patient experienced a postoperative complication, resulting in paraplegia (Table 6).
Table 6
| No. | Surgical intervention | Vertebral level | 1st line regimen and duration | 2nd line regimen and duration | Outcome |
|---|---|---|---|---|---|
| 1 | PLDF | L4–L5 | SDR (3 months) | – | Cure |
| 2 | Dorsal spine decompression with fusion | D3–D4 | SDR (3 months) | – | Cure |
| 3 | ACDF | C3–C6 | SDR (<3 months) | SRT (3 months) | Cure |
| 4 | ACDF | C4–C6 | SRT (3 months) | – | Cure |
| 5 | Partial laminectomy | L4–L5 | SDR (<3 months) | – | Cure |
| 6 | Laminectomy without fusion | L3–L4 | SDR (3 months) | – | Cure |
| 7 | ACDF | C3–C6 | GDC (8 months) | – | Cure |
| 8 | PLDF | L4–L5 | SDR (3 months) | – | Cure |
| 9 | Refuse surgery | L1–L2 | SDR (3 months) | SRT (3 months) | Cure‡ |
| 10 | Refuse surgery | L1–L2 | SDR (8 months) | – | Cure‡ |
| 11 | Refuse surgery | L3–L4 | SRT (8 months) | – | Cure‡ |
| 12† | Dorsal spine decompression with fusion | D3–D8 | SDR (3 months) | – | Cure |
†, patient became paraplegic after the surgery; ‡, abscess collection resolved by antibiotic treatment only. PLDF, posterior lumbar decompression and fusion; SDR, streptomycin + doxycycline + rifampicin; ACDF, anterior cervical discectomy and fusion; SRT, streptomycin + rifampicin + trimethoprim/sulfamethoxazole; GDC, gentamicin + doxycycline + ciprofloxacin.
Discussion
Spinal brucellosis poses a management challenge as physicians must select from various antibiotic regimens, which remains controversial. The specific regimen and duration are determined based on the patient’s response. In Brucella spondylitis intervention, a combination therapy approved by the National Antimicrobial Resistance Committee (NARC) and the Administration of Pharmaceutical Care at the Ministry of Health in Saudi Arabia includes doxycycline 100 mg per oral (po) every 12 h (q12h) for 6–8 weeks, along with gentamycin intravenous (IV) 3 mg/kg every 24 h (q24h) for 2–3 weeks. Alternatively, an alternative therapy consists of doxycycline 100 mg po q12h combined with trimethoprim (TMP)-sulfamethoxazole (SMX) 5 mg/kg of TMP component IV q12h, both administered for 6–8 weeks.
Occasionally, some patients may necessitate monotherapy intervention, which is not commonly used due to its high relapsing rate. Conversely, others may require triple therapy as a first-line therapy regimen in neurobrucellosis, as recommended by NARC (9). The selection and alteration of the regimen primarily depend on the patient’s response, treatment failure, and relapse rates. This study compares the efficacy of different antibiotic regimens for spinal brucellosis. Additionally, patients will be categorized based on the prescribed regimen (dual versus triple) and the duration of treatment.
Based on the data presented in Table 4, both dual therapy regimens, SR and DS, demonstrated effectiveness with a 100% cure rate. However, it is worth noting that SR was administered for only 2 months, while DS required a longer treatment duration of 6 months. A different study using the same DS regimen for 45 days showed a failure rate of 19% among 21 patients (10). In contrast, a non-randomized open clinical trial comparing two dual therapy regimens, DS and ciprofloxacin + rifampicin (CR), on 31 cases with spinal brucellosis revealed a 100% cure rate for 15 patients treated with DS and 16 patients treated with CR, with treatment durations varying up to 24 weeks (11).
DR is widely utilized as a dual regimen for Brucella spondylitis. In Turkey, a study conducted on 293 patients with uncomplicated spondylitis (spinal brucellosis with clinical and radiological or scintigraphic evidence of inflammation of one or more vertebrae and/or discitis in a patient with brucellosis) revealed that 70 out of 77 patients treated with DR for 3 months were successfully cured. However, only one failure case was reported out of 18 cases with complicated spondylitis (defined as any extension of infection through paravertebral and epidural spaces, the psoas muscle, or radicles with/without neurological involvement) (8).
Another clinical trial, also conducted in Turkey, compared five antimicrobial regimens for treating Brucella spondylitis, with DR chosen as the intervention in 20 patients out of 102. It demonstrated a 75% cure rate after 45 days. In comparison, an Iranian study showed a 90% cure rate among 18 patients, with eight of these patients receiving the regimen for 3 months, nine for 4 months, and three for 6 months (10,12).
Among all the triple therapy regimens presented in Tables 4,5, SRT and SDR, both commonly used in our center, demonstrated an overall cure rate of 100% and 75%, respectively. However, these findings differ from earlier observations in the literature, where SDR exhibited a higher overall cure rate of 92.2% among 94 patients (8).
A retrospective cohort study conducted in 2021 compared outcomes between patients managed with DR alone and DR combined with an aminoglycoside, showing an overall cure rate of 80% in 20 out of 25 patients on triple therapy. Conversely, 29 patients on dual therapy exhibited an 86% cure rate. Nonetheless, no significant difference between the two regimens was observed (13).
One of the most recent studies—published by Jeyaraman et al. [2023]—has proposed a systematic management plan for spinal brucellosis. The study included 25 confirmed cases of spinal brucellosis from a single center in India. Based on their findings, the authors suggested the following criteria: mild cases (defined as complaints that do not interfere with work) were suggested to be managed with antibiotic therapy for 10–12 weeks. Moderate cases (interferes with work along with bone destruction) are to be managed with rigid bracing combined with antibiotics for 12 weeks. Severe cases (defined as excruciating pain that prevents working, adjacent structure involvement, and sensory/motor deficit) are to be managed by surgical decompression and stabilization, along with antibiotic therapy for 12 weeks. However, the study’s authors acknowledged that the treatment duration was individualized among their patients based on the functional needs of each patient. This management plan is a preliminary suggestion, representing the initial step toward improving the treatment of spinal brucellosis (14).
The ratio of surgical intervention in patients with spinal brucellosis varies widely, ranging from 7% to 33% (7). Consistent with the present results, a previous study has also demonstrated that the most affected vertebral levels are L4–L5 and L5–S1. Among the surgical approaches, posterior lumbar interbody fusion (PLIF) is the most commonly used, followed by oblique lateral interbody fusion (OLIF). Jia et al. reported that PLIF is superior to OLIF in terms of shorter operative duration, hospital stay, and better clinical improvement. However, OLIF is still preferred in cases with paravertebral abscesses (15).
Surgical intervention is recommended for spinal brucellosis under certain conditions, including antibiotic treatment failure, the presence of neurological deficits, and abscess formation. However, in cases where abscesses are present, an increase in antibiotic duration may sometimes be sufficient (6,16). Our earlier observations align with this, as we noted three patients who opted not to undergo surgery. Instead, they received antibiotics for 3 or 8 months and eventually showed complete clinical improvement and resolution of the abscesses.
The results of this study demonstrate a male predominance, similar to a study conducted in Al-Qassim, Saudi Arabia (17). This could be attributed to their occupations as veterinarians, shepherds, or farmers, which might expose them to a higher risk of contracting brucellosis. In the present study, the most affected age group was 48–63 years, whereas other studies conducted in Saudi Arabia reported the most affected age groups as 30–39 and 20–30 years (17,18).
Symptoms of brucellosis can be vague and non-specific (19). Although fever is the most commonly reported symptom in patients with uncomplicated brucellosis (20), among our patients, low back pain was the most frequently reported symptom, followed by fever and lower limb weakness.
Although our study has obtained important information regarding the treatment regimens and outcomes among patients with spinal brucellosis, it includes several limitations to disclose. First, the limited sample size may affect the results of our study, which, in turn, may affect the conclusion. Thus, we recommend future studies with relatively large samples to be conducted locally and internationally in multi-centers to express the findings. Second, the nature of our retrospective design of reviewing the data from the hospital’s system records may include reporting bias.
Conclusions
In conclusion, the medical field has extensively debated the use of dual versus triple therapy in managing spinal brucellosis. In this study, we found that among 35 patients, treatment failure was observed only in six patients who received triple therapy. In addition, surgical intervention was indicated in 12 patients; however, three patients refused surgery and ultimately improved after changing or extending the duration of the antibiotic regimen.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-23-104/rc
Data Sharing Statement: Available at https://jss.amegroups.com/article/view/10.21037/jss-23-104/dss
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-23-104/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-23-104/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the Ethics Committee of the Ministry of Health (No. H-02-K076-1221-624). Informed consent was taken from all the patients. Additionally, the study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Centers for Disease Control and Prevention; National Center for Emerging and Zoonotic Infectious Diseases (NCEZID) D of HCP and P (DHCPP). Brucellosis. 2019. Available online: https://www.cdc.gov/brucellosis/index.html
- Dadar M, Fakhri Y, Shahali Y, et al. Contamination of milk and dairy products by Brucella species: A global systematic review and meta-analysis. Food Res Int 2020;128:108775. [Crossref] [PubMed]
- Dean AS, Crump L, Greter H, et al. Global burden of human brucellosis: a systematic review of disease frequency. PLoS Negl Trop Dis 2012;6:e1865. [Crossref] [PubMed]
- Brucellosis - Epidemiology. BMJ Best Practice 2019. Available online: https://bestpractice.bmj.com/topics/en-us/911
- Saudi National Registry of Ministry of Health. Statistical Yearbook. 2019:178-9. Available online: https://www.moh.gov.sa/en/Ministry/Statistics/book/Pages/default.aspx
- Esmaeilnejad-Ganji SM, Esmaeilnejad-Ganji SMR. Osteoarticular manifestations of human brucellosis: A review. World J Orthop 2019;10:54-62. [Crossref] [PubMed]
- Kaptan F, Gulduren HM, Sarsilmaz A, et al. Brucellar spondylodiscitis: comparison of patients with and without abscesses. Rheumatol Int 2013;33:985-92. [Crossref] [PubMed]
- Ulu-Kilic A, Karakas A, Erdem H, et al. Update on treatment options for spinal brucellosis. Clin Microbiol Infect 2014;20:O75-82. [Crossref] [PubMed]
- National Antimicrobial Therapy Guidelines for Community and Hospital Acquired Infections in Adults. [Cited 2023 Jul 6]. Available online: https://saudithoracicsociety.org/wp-content/uploads/2019/11/National-Antimicrobial-Guidelines-for-Community-and-Hospital-Acquired-Infections-in-Adults.pdf
- Bayindir Y, Sonmez E, Aladag A, et al. Comparison of five antimicrobial regimens for the treatment of brucellar spondylitis: a prospective, randomized study. J Chemother 2003;15:466-71. [Crossref] [PubMed]
- Alp E, Koc RK, Durak AC, et al. Doxycycline plus streptomycin versus ciprofloxacin plus rifampicin in spinal brucellosis BMC Infect Dis 2006;6:72. [ISRCTN31053647]. [Crossref] [PubMed]
- Smailnejad Gangi SM, Hasanjani Roushan MR, Janmohammadi N, et al. Outcomes of treatment in 50 cases with spinal brucellosis in Babol, Northern Iran. J Infect Dev Ctries 2012;6:654-9. [Crossref] [PubMed]
- Al-Madfaa RO, Alalawi MA, Basudan LO, et al. Dual versus triple therapy for uncomplicated brucellosis: A retrospective cohort study. J Infect Dev Ctries 2020;14:1380-6. [Crossref] [PubMed]
- Jeyaraman N, Jeyaraman M, Nallakumarasamy A, et al. A proposed management classification for spinal brucellosis from India. Travel Med Infect Dis 2023;54:102614. [Crossref] [PubMed]
- Jia YL, Zuo XH, Zhang Y, et al. Clinical value and effectiveness profiles of oblique lateral interbody fusion and posterior lumbar interbody fusion in the treatment of lumbar brucellosis spondylitis. Eur Rev Med Pharmacol Sci 2023;27:3854-63. [PubMed]
- Roushan MRH, Ebrahimpour S, Afshar ZM, et al. Cervical Spine Spondylitis with an Epidural Abscess in a Patient with Brucellosis: A Case Report. J Crit Care Med (Targu Mures) 2019;5:103-6. [Crossref] [PubMed]
- Alsoghair MI. Epidemiological characteristics of human brucellosis in Al-Qassim region, Saudi Arabia, between 2010 and 2014. Int J Community Med Public Health 2017;3:397-402.
- Al-Tawfiq JA, Abukhamsin A. A 24-year study of the epidemiology of human brucellosis in a health-care system in Eastern Saudi Arabia. J Infect Public Health 2009;2:81-5. [Crossref] [PubMed]
- Doganay M, Aygen B. Human brucellosis: an overview. Int J Infect Dis 2003;7:173-82. [Crossref]
- Bodur H, Erbay A, Colpan A, et al. Brucellar spondylitis. Rheumatol Int 2004;24:221-6. [Crossref] [PubMed]




