
Appropriate pelvic obliquity measurement method in Lenke type 5C adolescent idiopathic scoliosis: a preliminary study
Highlight box
Key findings
• In patients with adolescent idiopathic scoliosis (AIS) Lenke 5C, sacral obliquity (SO) is considered a more appropriate parameter than iliac obliquity (IO) for assessing pelvic obliquity (PO). This is because SO more effectively represents the effects on the lower lumbar spine.
What is known and what is new?
• IO has been utilized as a coronal pelvic parameter due to its high inter-rater and intra-rater reliability. However, IO reflects various factors such as leg length discrepancy, asymmetry of sacral and iliac morphology, and compensatory motion of the sacroiliac joints. These factors make it challenging to accurately evaluate the impact of PO on the lower lumbar spine tilt.
• This study introduces the significance of SO in assessing coronal pelvic parameters and explores the potential of substituting computed tomography (CT) imaging when SO measurement is difficult on standing posteroanterior whole-spine radiographs.
What is the implication, and what should change now?
• For assessing PO in AIS Lenke 5C, it is recommended to assess using SO instead of IO. If visibility of SO is compromised, CT imaging can serve as an alternative method.
Introduction
Adolescent idiopathic scoliosis (AIS) is a multifactorial three-dimensional spinal deformity in youth (1,2). AIS Lenke type 5C is defined as a structural thoracolumbar/lumbar (TL/L) curve without structural curves in the upper thoracic and main thoracic regions (3). In this condition, the lower lumbar vertebra and sacrum are often tilted to the left side with a left thoracolumbar curve and associated with clinically and radiological coronal imbalance (4-6). Due to concerns that the lower lumbar spine tilt may accelerate degenerative changes, a smaller Cobb angle threshold of 45 degrees is recommended as a surgical indication for Lenke type 5C (7), compared with 50 degrees for Lenke type 1A (8).
To correct the lower lumbar spine tilt, it is essential to consider the tilt of the pelvis, which is the foundation of the spine (9). Pelvic obliquity (PO), defined as a coronal pelvic tilt, has been reported to be a risk factor for postoperative coronal decompensation (10). Iliac obliquity (IO), the parameter of iliac tilt, has often been used to evaluate PO. However, IO reflects various factors such as leg length discrepancy (11), asymmetry of sacral and iliac morphology (12), and compensatory motion of the sacroiliac joints, making it difficult to properly evaluate PO’s effect on lower lumbar spine tilt. On the other hand, sacral obliquity (SO), which directly affects the lower lumbar tilt, is presumed to be an appropriate pelvic parameter for AIS.
A challenge in measuring SO on standing posteroanterior (PA) whole-spine radiographs is that a large anteroposterior tilt of the sacrum, which forms considerable angle with the angle of the X-ray beam, makes it difficult to identify and measure SO precisely in some patients. However, if the parameters for measuring SO using multiplanar reconstructed computed tomography (MPR-CT) images show a strong correlation with SO on standing PA whole-spine radiographs, the latter can still be estimated using the former, even in patients with a large anteroposterior tilt of the sacrum. This study aimed to establish an appropriate measurement method using MPR-CT images to evaluate PO in patients with Lenke type 5C AIS. We present this article in accordance with the STROBE reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-23-138/rc).
Methods
This was a retrospective cross-sectional study. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of Osaka University Hospital (No. 11360-7), and individual consent for this retrospective analysis was waived.
Of 34 consecutive patients who underwent corrective surgery for AIS with structural lower lumbar curve (Lenke type 3, 4, 5, 6) from August 2014 to February 2023 in Osaka University Hospital, 25 patients (74%) were included in this study. There were four cases of type 3, two cases of type 4, 21 cases of type 5, and seven cases of type 6. No patient had history of spinal surgery, history of hip joint dysfunction, lumbosacral transitional vertebrae, spina bifida occulta, and specific cause of scoliosis, such as neuromuscular disease, syringomyelia, congenital heart disease, and syndrome-related scoliosis. Nine cases were excluded from the study due to the preoperative CT scans not including the femoral heads bilaterally, which included two cases of type 3, one case of type 4, four cases of type 5, and two cases of type 6. In this study, Due to the limited number of cases for type 3, 4, and 6, they were only used for the validation of intraclass correlation coefficients (ICCs).
Demographic and radiological information was collected through a review of the electronic medical records. Demographic data included preoperative patient age, sex, height, weight, and body mass index (BMI). Radiological information was obtained with standing PA whole-spine radiographs and CT which was performed using either of two scanners (Discovery CT750 HD; GE Healthcare Japan, Tokyo, Japan or Aquilion ONE; CANON MEDICAL SYSTEMS CORPORATION, Tochigi, Japan), preoperatively. We used a three-dimensional image analysis device (Synapse Vincent; Fuji Medical Systems, Tokyo, Japan) for CT evaluation. All patients had standing PA whole-spine radiographs taken the day before or the day of CT.
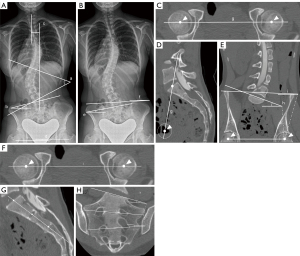
Measurement of radiological parameters
The measurement of radiological parameters is shown in Figure 1. TL/L Cobb angle (Cobb angle), L5 tilt, distance from C7 plumb line to center sacral vertebral line (C7PL-CSVL), and leg length discrepancy (LLD) were measured on standing PA whole-spine radiographs. Cobb angle was measured as the angle between the superior end plate of the most cephalad end vertebra and the inferior end plate of the most caudal end vertebra in the curve. L5 tilt was measured as the angle between the horizontal line and the upper endplate of L5. C7PL-CSVL was the vertical distance between two vertical lines drawn from the center of the C7 vertebral body and from the middle of the S1 vertebra. LLD was the difference between the height of horizontal lines that were tangent to the top of the highest femoral head and lowest femoral head (13). Standing PA whole-spine radiographs and MPR-CT images were used to determine the SO and IO values, referred to as SO/IO-X-ray and SO/IO-CT, respectively. SO-X-ray is the angle between the upper endplate of the S1 vertebra and the horizontal plane, and IO-X-ray is the angle between the line of the iliac crest and the horizontal plane (14), measured on standing PA whole-spine radiographs. SO-CT and IO-CT are both angles measured on a plane passing through three points: the center of the S1 vertebra’s upper endplate and the centers of two femoral heads. Specifically, SO-CT is defined as the angle between the upper endplate of the S1 vertebra and the line connecting the two femoral heads’ centers, while IO-CT is the angle between the line of the iliac crest and the same line connecting the femoral head centers. The sacral asymmetry parameters, S1 vertebral wedge angle (S1 angle) and S2 vertebral wedge angle (S2 angle) were determined using MPR-CT images. S1 angle/S2 angle are the angles of the upper and lower endplates in the plane parallel to the line connecting the two femoral heads and passing through the center of the upper and lower endplates of S1/S2. Three raters who had experience with spine surgery for 6 and 2 years measured SO-CT and IO-CT. Each parameter was measured three times with a 1-month interval. Inter-rater and intra-rater reliability were assessed by calculating ICCs, with ICCs of 0.8–1.0, 0.6–0.79, and <0.6 defined as good, moderate, and poor, respectively (15).
Statistical analysis
The statistical analysis was performed using IBM SPSS statistics version 27.0 (IBM Corp., Armonk, NY, USA). All descriptive statistics with continuous variables were analyzed for normality using Shapiro-Wilk test. For normally distributed parameters, the mean, standard deviation (SD), and range were calculated, and the parameters were compared using the paired-t-test. For not normally distributed parameters, the median and interquartile range (IQR) were calculated, and the parameters were compared using Wilcoxon signed-rank test. Correlations between the variables of the spinopelvic parameters were examined using Spearman’s rank correlation coefficient. In all validity analyses, the coefficient values were characterized as follows: 0–0.19 was slight almost negligible relationships; 0.20–0.39 was low correlation; 0.40–0.69 was moderate correlation; 0.70–0.89 was high correlation; 0.90–1.00 was very high correlation/ very dependable relationship (16). Furthermore, we performed a multiple linear regression analysis using SO-CT, IO-X-ray, and IO-CT as factors to explain SO-X-ray, investigating which factors contributed most to SO-X-ray as explanatory variables.
Results
The mean age of the patients was 18.7±3.9 years at the time of surgery, and all of them were females. Table 1 shows the preoperative radiographic parameters on standing PA whole-spine radiographs and the results of comparing SO ad IO measuring on standing PA whole-spine radiographs and CT. The mean Cobb angle was 44.0±6.4° (range, 40.6–47.4°), L5 tilt was 12.9±3.6° (range, 11.0–14.9°), C7PL-CSVL was −27.0±12.1° (range, −34.3 to −19.7°), and LLD was 5.4±4.3 mm (range, 2.6–8.3 mm). There was no patient with an LLD larger than 20 mm. SO-X-ray was 7.8±2.5° (range, 6.4–9.1°), SO-CT was 9.8±5.1° (range, 7.1–12.5°), IO-X-ray was 3.3±2.1° (range, 2.2–4.4°), and IO-CT was 2.2±1.1° (range, 1.7–2.8°). SO was larger than IO in both measurement methods (P<0.001). The mean S1 angle was 4.5±3.5° (range, 2.7–6.4°), and the S2 angle was 1.2±2.1° (range, 0.0–2.3°), which was significantly smaller than the mean S1 angle (P<0.001). Table 2 shows that SO-CT was larger than SO-X-ray (P=0.02) and IO-CT was larger than IO-X-ray (P=0.02). The ICCs for intra- and inter-rater reliability of SO-CT were 0.984 and 0.970, and those of IO-CT were 0.936 and 0.921.
Table 1
| Variable | Overall (n=17) | P value |
|---|---|---|
| Cobb angle (°) | 44.0±6.4 (40.6–47.4) | |
| L5 tilt (°) | 12.9±3.6 (11.0–14.9) | |
| C7PL-CSVL (mm) | −27.0±12.1 (−34.3 to −19.7) | |
| LLD (mm) | 5.4±4.3 (2.6–8.3) | |
| Pelvic parameter on X-ray | <0.001* | |
| SO-X-ray (°) | 7.8±2.5 (6.4–9.1) | |
| IO-X-ray (°) | 3.3±2.1 (2.2–4.4) | |
| Pelvic parameter on CT | <0.001* | |
| SO-CT (°) | 9.8±5.1 (7.1–12.5) | |
| IO-CT (°) | 2.2±1.1 (1.7–2.8) | |
| Sacral parameter on CT | <0.001* | |
| S1 angle (°) | 4.5±3.5 (2.7–6.4) | |
| S2 angle (°) | 1.2±2.1 (0.0–2.3) |
Values are presented as mean ± standard deviation (range). *, statistically significant difference. C7PL-CSVL, distance from C7 plumb line to center sacral vertebral line; LLD, leg length discrepancy; SO-X-ray, sacral obliquity-X-ray; IO-X-ray, iliac obliquity-X-ray; SO-CT, sacral obliquity-computed tomography; IO-CT, iliac obliquity-computed tomography; S1 angle, S1 vertebral wedge angle; S2 angle, S2 vertebral wedge angle.
Table 2
| Variable | Measurement methods | ||
|---|---|---|---|
| X-ray | CT | P value | |
| SO (°) | 7.8±2.5 (6.4–9.1) | 9.8±5.1 (7.1–12.5) | 0.02* |
| IO (°) | 3.3±2.1 (2.2–4.4) | 2.2±1.1 (1.7–2.8) | 0.02* |
*, statistically significant difference. Values are presented as mean ± standard deviation (range). CT, computed tomography; SO, sacral obliquity; IO, iliac obliquity.
Table 3 presents the Spearman’s correlation coefficients. There was no significant correlation between SO-X-ray and IO-X-ray (r=0.240, P=0.35). The correlation between SO-X-ray and IO-CT was moderate (r=0.512, P=0.04). Meanwhile, SO-X-ray was highly correlated with SO-CT (r=0.838, P<0.001). L5 tilt had higher correlation with SO-CT (r=0.884, P<0.001) than SO-X-ray (r=0.726, P=0.001) and IO-CT (r=0.550, P=0.02); meanwhile, L5 tilt was correlated poorly with IO-X-ray (r=0.104, P=0.69). S1 angle also correlated moderately with SO-CT (r=0.603, P=0.01), and L5 tilt (r=0.641, P=0.006). LLD was moderately correlated with IO-X-ray (r=0.695, P=0.002). Meanwhile, Cobb angle and C7PL-CSVL did not correlate significantly with any of the parameters.
Table 3
| Variable | Value | Cobb angle | L5 tilt | C7PL-CSVL | LLD | SO-X-ray | IO-X-ray | SO-CT | IO-CT | S1 angle | S2 angle |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cobb angle | ρ | 0.093 | −0.196 | −0.176 | −0.018 | −0.039 | 0.197 | 0.264 | 0.095 | −0.308 | |
| P | 0.72 | 0.45 | 0.50 | 0.95 | 0.88 | 0.45 | 0.31 | 0.72 | 0.23 | ||
| L5 tilt | ρ | 0.093 | −0.375 | −0.162 | 0.726 | 0.104 | 0.884 | 0.550 | 0.641 | 0.155 | |
| P | 0.72 | 0.14 | 0.53 | 0.001* | 0.69 | <0.001* | 0.02* | 0.006* | 0.55 | ||
| C7PL-CSVL | ρ | −0.196 | −0.375 | 0.372 | −0.024 | 0.003 | −0.143 | −0.254 | −0.283 | 0.442 | |
| P | 0.45 | 0.14 | 0.14 | 0.93 | 0.99 | 0.58 | 0.32 | 0.27 | 0.08 | ||
| LLD | ρ | −0.176 | −0.162 | 0.372 | −0.094 | 0.695 | −0.230 | −0.023 | −0.239 | 0.057 | |
| P | 0.50 | 0.53 | 0.14 | 0.72 | 0.002* | 0.37 | 0.93 | 0.36 | 0.83 | ||
| SO-X-ray | ρ | −0.018 | 0.0726 | −0.024 | −0.094 | 0.240 | 0.838 | 0.512 | 0.221 | 0.322 | |
| P | 0.95 | 0.001* | 0.93 | 0.72 | 0.35 | <0.001* | 0.04* | 0.39 | 0.21 | ||
| IO-X-ray | ρ | −0.039 | 0.104 | 0.003 | 0.695 | 0.240 | 0.113 | 0.469 | −0.082 | −0.122 | |
| P | 0.88 | 0.69 | 0.99 | 0.002* | 0.35 | 0.67 | 0.06 | 0.75 | 0.64 | ||
| SO-CT | ρ | 0.197 | 0.884 | −0.143 | −0.230 | 0.838 | 0.113 | 0.571 | 0.603 | 0.300 | |
| P | 0.45 | <0.001 | 0.58 | 0.37 | <0.001* | 0.67 | 0.02* | 0.01* | 0.24 | ||
| IO-CT | ρ | 0.264 | 0.550 | −0.254 | −0.023 | 0.512 | 0.469 | 0.571 | 0.366 | −0.030 | |
| P | 0.31 | 0.02* | 0.32 | 0.93 | 0.04* | 0.06 | 0.02* | 0.15 | 0.91 | ||
| S1 angle | ρ | 0.095 | 0.641 | −0.283 | −0.239 | 0.221 | −0.082 | 0.603 | 0.366 | 0.037 | |
| P | 0.72 | 0.006* | 0.27 | 0.36 | 0.39 | 0.75 | 0.01* | 0.15 | 0.89 | ||
| S2 angle | ρ | −0.308 | 0.155 | 0.442 | 0.057 | 0.322 | −0.122 | 0.300 | −0.030 | 0.037 | |
| P | 0.23 | 0.55 | 0.08 | 0.83 | 0.21 | 0.64 | 0.24 | 0.91 | 0.89 |
*, statistically significant difference. C7PL-CSVL, distance from C7 plumb line to center sacral vertebral line; LLD, leg length discrepancy; SO-X-ray, sacral obliquity-X-ray; IO-X-ray, iliac obliquity-X-ray; SO-CT, sacral obliquity-computed tomography; IO-CT, iliac obliquity-computed tomography; S1 angle, S1 vertebral wedge angle; S2 angle, S2 vertebral wedge angle; ρ, Spearman correlation coefficient.
A multiple linear regression analysis was utilized to predict SO-X-ray with SO-CT, IO-X-ray, and IO-CT as the independent variables, yielding an R-squared value of 0.687. This suggests our model accurately predicts the dependent variable. The standardized beta coefficient for SO-CT was notably higher at 0.781 (P=0.004), compared to 0.021 for IO-X-ray (P=0.91) and 0.055 for IO-CT (P=0.83), indicating SO-CT’s dominant contribution to the model.
Discussion
In this study, SO and IO were examined as PO. SO and IO showed no significant relationship with global balances such as Cobb angle and C7PL-CSVL. SO-CT was larger than SO-X-ray, and SO was significantly larger than IO for both measures. SO-CT showed a higher correlation with SO-X-ray than with either IO-X-ray or IO-CT. SO showed a higher correlation than IO with L5 tilt for all measures. The ICCs for intra- and inter-rater reliability of SO-CT and IO-CT were good.
The pelvis serves as the foundation and adjacent structure to the lower lumbar spine; PO is an essential parameter in corrective surgery for AIS. However, there is no standard method to evaluate PO, and various techniques are used. The ilium, sacrum, and ischium are often used as reference points for determining PO. Some methods that utilize the iliac crest as a reference point, i.e., IO, include the Maloney technique (17), the Osebold technique (14), and the Allen and Ferguson technique (18). The PO measurement in the Maloney technique is defined as the angle between the line perpendicular to the line connecting the iliac crest and T1, and the line connecting the center of S1. In the Osebold technique, PO is the angle between the line connecting the iliac crest and a horizontal line. Meanwhile, in the Allen and Ferguson technique, PO is calculated as the angle between the line perpendicular to the line connecting the iliac crest and the line connecting the L4 and L5 spinous processes. A previous comparative study showed that the interclass correlation coefficients are highest in the Maloney and Osebold techniques and did not differ significantly between the two (19). In this study, we adopted the Osebold technique as an IO measurement because of its reliability and widespread use. Techniques utilizing the sacrum as a reference point, i.e., SO, include the O’Brien technique (13) and the Cho technique (20). The O’Brien technique determines PO as the angle between the endplate line of the S1 vertebra and the horizontal plane, while the Cho technique calculates PO as the angle between the line connecting the transition point of the sacral wing and the superior articular process of the S1 vertebra and the horizontal plane. We used the O’Brien technique as a SO measuring method because patients with deformity of the upper part of the S1 vertebra are common.
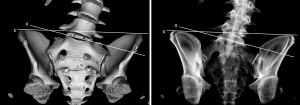
Because of its high visibility, many previous reports have used the ilium-based measurement method known as IO. However, the suitability of IO as a proxy for PO is still being evaluated. In this study, IO was smaller than SO in both measurement methods on standing PA whole-spine radiographs and CT. Figure 2 illustrates a typical case. A previous report about 303 AIS cases showed that SO [1.86°±3.06° (range, −10° to 14°)] was larger than IO [1.10°±2.28° (range, −6° to 8°)] (20). Moreover, the frequency of ≥5° of SO and IO were 20.2% and 8.3%. Another study reported that SO was larger than IO in scoliosis with lumbar curve whereas no significant difference was found between SO and IO in cases with developmental dysplasia of the hip (21). SO is also larger than IO in the present study, consistent with previous reports.
IO is challenging to accurately assess PO’s impact on lower lumbar spine tilt in patients with AIS Lenke 5C since IO reflects various characteristics including leg length variations, asymmetry of iliac morphology, but not intrinsic sacral deformity and compensatory motion of the sacroiliac joints (21). This study showed that L5 tilt strongly correlated with SO, a parameter between adjacent vertebrae, but had no significant correlation with IO. L5 tilt is an important parameter because it has been reported to be involved in postoperative coronal imbalance. Moreover, in the current study, S1 angle was 5.5±3.4°, and correlated well with SO-CT (r=0.603, P=0.01), and L5 tilt (r=0.641, P=0.006). These results may explain that the higher correlation of SO with L5 tilt compared to IO may reflect the sacral asymmetry common in Lenke 5 type C, but this has not been noted in previous literature.
SO may be more appropriate than IO in assessing global spinal alignment in Lenke type 5C patients, but the measurement of SO is controversial. Although SO-X-ray is straightforward, it has the disadvantage that the SO is not clear due to the anteroposterior tilting of the sacrum. In this case, SO-CT, which has a strong correlation with SO-X-ray and can measure SO without exception, is considered valuable. As the relative sacral anteroposterior tilt increased in the measurement plane, SO-CT became larger than SO-X-ray. In this study, the ratio of SO-X-ray to SO-CT is 0.75. Further studies to confirm the ratio would be useful for measuring SO.
This study has some limitations. First, we restricted the case to type 5C, the number of enrolled patients was small because the femoral head is not included in the imaging range in many cases. Further study of an appropriate measurement method that does not require the femoral head is needed. Second, the study’s retrospective design may have introduced bias. However, selection bias is minimized because all consecutive surgical cases are included in the study. Third, despite the strong relationship between LLD and scoliosis, we could not enroll large LLD cases. Patients with LLD larger than 20 mm have been noted to be associated with low back pain and other symptoms, and surgical correction may be considered (22). However, we do not consider that the results are significantly affected by this study or previous studies, as SO and LLD were not correlated in this study or previous studies. Finally, it was unable to determine in this study which came first, sacral asymmetry or scoliosis progression due to the lack of images preceding the progression of the curve. Future studies should focus on the sacral morphology prior to the scoliosis advancement.
Conclusions
Sacral tilt due to sacral vertebral asymmetry may be seen in AIS Lenke 5C patients. Given the asymmetric sacral morphology, SO is an appropriate pelvic parameter to represent the sacral tilt of AIS Lenke 5C, especially when measured using reconstructed CT to overcome the poor visibility on the standing radiographs due to a large anteroposterior tilt of the sacrum in some patients.
Acknowledgments
We would like to express our gratitude for the valuable advice received during the presentation of part of this research at the Japanese Society for Spine Surgery and Related Research session during Spineweek 2023.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-23-138/rc
Data Sharing Statement: Available at https://jss.amegroups.com/article/view/10.21037/jss-23-138/dss
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-23-138/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-23-138/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was approved by the Institutional Review Board of Osaka University Hospital (No. 11360-7) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Weinstein SL, Dolan LA, Wright JG, et al. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med 2013;369:1512-21. [Crossref] [PubMed]
- Altaf F, Gibson A, Dannawi Z, et al. Adolescent idiopathic scoliosis. BMJ 2013;346:f2508. [Crossref] [PubMed]
- Lenke LG, Betz RR, Harms J, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am 2001;83:1169-81. [Crossref] [PubMed]
- Nissinen MJ, Heliövaara MM, Seitsamo JT, et al. Development of trunk asymmetry in a cohort of children ages 11 to 22 years. Spine (Phila Pa 1976) 2000;25:570-4. [Crossref] [PubMed]
- Banno T, Yamato Y, Hasegawa T, et al. Impact of pelvic obliquity on coronal alignment in patients with adolescent idiopathic scoliosis. Spine Deform 2020;8:1269-78. [Crossref] [PubMed]
- Zuckerman SL, Cerpa M, Sardar ZM, et al. Don't forget the pelvis: accounting for pelvic rotation in the preoperative assessment of adolescent idiopathic scoliosis. J Spine Surg 2021;7:181-9. [Crossref] [PubMed]
- Chan CYW, Naing KS, Chiu CK, et al. Pelvic obliquity in adolescent idiopathic scoliosis planned for posterior spinal fusion: A preoperative analysis of 311 lower limb axis films. J Orthop Surg (Hong Kong) 2019;27:2309499019857250. [Crossref] [PubMed]
- Weinstein SL, Ponseti IV. Curve progression in idiopathic scoliosis. J Bone Joint Surg Am 1983;65:447-55. [Crossref] [PubMed]
- Zuckerman SL, Sardar ZM, Marciano G, et al. The Importance of Pelvic Obliquity in Assessing Spinal Coronal Alignment: Normative Values, Demographic, and Radiographic Correlations. Clin Spine Surg 2024;37:E124-30. [Crossref] [PubMed]
- Schwender JD, Denis F. Coronal plane imbalance in adolescent idiopathic scoliosis with left lumbar curves exceeding 40 degrees: the role of the lumbosacral hemicurve. Spine (Phila Pa 1976) 2000;25:2358-63. [Crossref] [PubMed]
- Zuckerman SL, Lai CS, Shen Y, et al. Understanding the role of pelvic obliquity and leg length discrepancy in adult spinal deformity patients with coronal malalignment: unlocking the black box. J Neurosurg Spine 2022;37:64-72. [Crossref] [PubMed]
- Phillips L. An Oblique Pelvis Associated with a Congenital Dislocation of the Hipjoint. Br Med J 1901;2:1658-9. [Crossref] [PubMed]
- O’Brien MF, Kuklo TR, Blanke KM, et al. Radiographic Measurement Manual. Spinal Deformity Study Group (SDSG). Medtronic Sofamor Danek USA, Inc., Edition; 2008.
- Osebold WR, Mayfield JK, Winter RB, et al. Surgical treatment of paralytic scoliosis associated with myelomeningocele. J Bone Joint Surg Am 1982;64:841-56. [Crossref] [PubMed]
- Xue C, Yuan J, Lo GG, et al. Radiomics feature reliability assessed by intraclass correlation coefficient: a systematic review. Quant Imaging Med Surg 2021;11:4431-60. [Crossref] [PubMed]
- Guilford JP. Fundamental statistics in psychology and education. New York: McGraw Hill; 1956.
- Maloney WJ, Rinsky LA, Gamble JG. Simultaneous correction of pelvic obliquity, frontal plane, and sagittal plane deformities in neuromuscular scoliosis using a unit rod with segmental sublaminar wires: a preliminary report. J Pediatr Orthop 1990;10:742-9. [Crossref] [PubMed]
- Allen BL Jr, Ferguson RL. The Galveston technique of pelvic fixation with L-rod instrumentation of the spine. Spine (Phila Pa 1976) 1984;9:388-94. [Crossref] [PubMed]
- Karkenny AJ, Magee LC, Landrum MR, et al. The Variability of Pelvic Obliquity Measurements in Patients with Neuromuscular Scoliosis. JB JS Open Access 2021;6:e20.00143.
- Cho JH, Lee CS, Joo YS, et al. Association between Sacral Slanting and Adjacent Structures in Patients with Adolescent Idiopathic Scoliosis. Clin Orthop Surg 2017;9:57-62. [Crossref] [PubMed]
- Yu Y, Song K, Wu B, et al. Coronal Compensation Mechanism of Pelvic Obliquity in Patients With Developmental Dysplasia of the Hip. Global Spine J 2023;13:949-53. [Crossref] [PubMed]
- Sheha ED, Steinhaus ME, Kim HJ, et al. Leg-Length Discrepancy, Functional Scoliosis, and Low Back Pain. JBJS Rev 2018;6:e6. [Crossref] [PubMed]


