
A case series in vertebral body tethering results in improvement in coronal Cobb angle but deterioration in axial rotation: a 3-dimensional analysis
Highlight box
Key findings
• This is the first case series to reveal apical axial rotation progression despite coronal Cobb angle improvements post-vertebral body tethering (VBT) surgery.
• VBT does not control changes in axial rotation and coupling effect may not hold true.
What is known and what is new?
• VBT has shown improvements in coronal and sagittal plane correction in patients with adolescent idiopathic scoliosis, however axial rotation correction overtime remains unexplored.
• We observed that apical axial rotation deteriorates compared to pre-operatively at 2 years follow up, while coronal Cobb angle shows improvement overtime at 2 years follow up.
What is the implication, and what should change now?
• Surgeons and patients should be aware of such findings in their decision to select VBT as their procedure of choice.
Introduction
Adolescent idiopathic scoliosis (AIS) is a complex three-dimensional (3D) deformity of the spine (1-4) which are commonly detected by radiographs, characterized by the rotation of the apical vertebrae away from the midline (3D) pattern (5,6). Notably, imaging studies have revealed that the apical vertebrae in AIS curves exhibit the greatest degree of axial rotation (7,8).
Traditionally, posterior spinal fusion (PSF) surgery had been the treatment of choice for severe scoliosis. Vertebral body tethering (VBT) has a raising popularity as a non-fusion method of treatment (9). VBT utilizes the Hueter-Volkman phenomenon (10), limiting the growth of spine on one side, and allowing the curvature to progressively correct with growth. Previous studies have demonstrated that VBT can lead to significant improvements in the coronal Cobb angle, with correction rates ranging from 28.5% to 100.0% at the 2-year follow-up compared to pre-operative angles (11-25).
Furthermore, VBT has been shown to maintain thoracic kyphosis (TK) values within a stable range of 5.0° (15-17,19,21,24-27), and even normalised to 20°–40° (28) at the 2-year follow-up. Additionally, lumbar lordosis (LL) was found to be stable within 7° at 2 years follow-up (13,17,24,25,27). On the other hand, axial correction of the deformity has not been well studied. Some studies utilising scoliometers have suggested improvements at 2-year follow-up (13,27,29).
It is generally recognized that if spinal deformity is corrected in one plane, the other planes will also spontaneously correct (30). However, it is currently unclear whether coupling effects and 3D spinal corrections occur in VBT patients. The objective of this study was to evaluate 3D corrections following VBT surgery and investigate whether axial correction is coupled with the correction of coronal deformity. We present this case series in accordance with the AME Case Series reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-24-59/rc).
Case presentation
This is a retrospective analysis of prospectively collected data of eight AIS subjects with right sided thoracic scoliosis treated by VBT at the Department of Orthopaedics and Traumatology, the University of Hong Kong, between February 2019 and December 2020, reported as a case series. Inclusion criteria were initial curve magnitude larger than 40°, a Risser sign of ≤2 at VBT surgery and with a minimum 2 years of follow-up. Ten continuous subjects were retrieved and assessed for eligibility. Of them, 2 were excluded since they did not have complete set of biplanar images or had only lumbar scoliosis. All procedures performed in this study were in accordance with the ethical standards of the institutional research committee of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (approval number: 19-002) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients and their parents for the publication of this case series and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
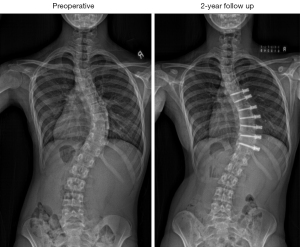
Measurements
For each subject, pre-operative standing anteroposterior (AP) and lateral (LAT) biplanar spine radiographs were taken using EOS® system (EOS® imaging, Paris, France) preoperatively (pre-op). Subsequent images were then taken at immediate post-operative (post-op) with first erect X-ray, at 1- and 2-year follow-up. Subject-specific 3D spinal reconstruction models were then created by blinded evaluator at each timepoint using sterEOS® software (EOS® Imaging, Paris, France). Coronal, sagittal, and axial rotation measurements including major curve Cobb angle, TK (vertebral levels T1–12), LL (vertebral levels L1–5) and axial rotation of curve apex were made from 3D reconstruction models. Data were then compared at each timepoints.
3D reconstruction
The 3D reconstruction model data were compared with measurements made on original 2D biplanar radiographs for each subject at every timepoint, and difference between 2D and 3D measurement outcomes was compared to published thresholds (31).
Tether breakage
Tether cord integrity were closely assessed at each follow-up and tether breakages were confirmed with computed tomography (CT) scan (32,33).
Statistical analysis
All statistical data analyses were performed using SPSS software (SPSS Inc., Chicago, Illinois, USA). A paired t-test were used to evaluate whether the corrections in coronal, sagittal and axial planes were significant compared to pre-operative angles (P value of 0.05). A Pearson’s correlation coefficient was conducted to analyse the relationship of each parameter at each timepoint (P value of 0.05).
Demographics
There were 7 females and 1 male subjects included in our series with a mean follow-up of 26.8±4.1 months (range, 24–36 months). The average age at VBT surgery performed was 11.8±1.3 years (range, 10.0–13.9 years). Four subjects had Risser 0, one Risser 1 and three Risser 3 at the time of surgery. Six subjects had Lenke type 1 with thoracic VBT and two subjects had Lenke type 3 with thoracic and lumbar VBT. Subjects underwent tethering of an average of 7.1±0.6 (range, 6–8) levels, with the most proximal being T5 and most distal L1 (Table 1).
Table 1
| Subject | Pre-op Cobb angle (°) | Fulcrum bend (°) | 2YFU correction rate (%) | VBT tethered levels | Tether breakage |
|---|---|---|---|---|---|
| 1 | 44.0 | 16.5 | 86.1 | T6–L1 | Y |
| 2 | 45.4 | 4.1 | 77.8 | T7–L1 | Y |
| 3 | 49.8 | 17.9 | 1.0 | T6–T12 | N |
| 4 | 41.3 | 16.8 | 26.4 | T5–T12 | Y |
| 5 | 65.7 | 35.8 | 39.0 | T6–T12 | N |
| 6 | 51.8 | 3.6 | 38.4 | T5–T11 | Y (15M) |
| 7 | 46.9 | 14.1 | 63.3 | T6–T12 | Y |
| 8 | 58.1 | 10.3 | 45.4 | T6–T11 | Y |
Subject 3 and 5 did not have tether breakage. Subject 6 had tether breakage at 15 months while others were after 2 years. VBT, vertebral body tethering; Pre-op, preoperative; 2YFU, 2-year follow-up; Y, yes; N, no; 15M, 15 months.
Coronal and sagittal correction
Coronal and sagittal correction results are summarised in Table 2. There is an improvement in mean coronal angle correction from 50.4°±8.1° to 27.1°±14.9° in 2 years. TK and LL had remained stable at 2 years follow-up.
Table 2
| VBT subjects | Coronal Cobb angle | Apical axial rotation | TK | LL |
|---|---|---|---|---|
| Pre-op | 50.4° (8.1°) | −5.5° (5.0°) | 35.2° (10.1°) | 46.1° (8.7°) |
| Immediate post-op | 28.4° (10.0°) | −1.4° (4.8°) | 39.0° (8.5°) | 42.8° (11.0°) |
| Correction rate | 43.7% | 74.7% | −10.7% | 7.3% |
| P | 0.001* | 0.071 | 0.037 | 0.062 |
| 1-year follow-up | 19.2° (14.0°) | −3.2° (4.9°) | 31.3° (15.4°) | 36.5° (15.3°) |
| Correction rate | 62% | 42.4% | 11.3% | 20.9% |
| P | <0.001* | 0.207 | 0.492 | 0.015 |
| 2-year follow-up | 27.1° (14.9°) | −7.0° (5.9°) | 37.0° (14.5°) | 42.8° (10.5°) |
| Correction rate | 46.2% | −27.2% | −4.9% | 7.3% |
| P | 0.001* | 0.275 | 0.325 | 0.18 |
The results are expressed as mean and standard deviation. Correction rate is relative to pre-operative angles. *, significant differences (P<0.05). VBT, vertebral body tethering; Pre-op, preoperative; Post-op, postoperative; TK, thoracic kyphosis; LL, lumbar lordosis.
Apical axial rotation
Axial rotation of the curve apex showed a mean deterioration from −5.5°±5.0° to −7.0°±5.9° over 2 years with results summarised in Table 2. Subject-specific axial rotation changes are shown in Figure 1. Subject 1, 2, and 5 showed improvements at 2 years follow-up, while subject 3, 4, 6, 7, and 8 showed deterioration at 2-year follow-up when compared to preoperative angles.

Correlation
Pearson correlation was performed to identify associations between all spinal planes after VBT surgery. Coronal Cobb angle correction was found to be significant negatively correlated to apical axial rotation correction at 2-year follow-up (Table 3).
Table 3
| VBT subjects | Coronal Cobb angle | Apical axial rotation | TK | LL | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| R | Sig. | R | Sig. | R | Sig. | R | Sig. | ||||
| Pre-op | |||||||||||
| Coronal Cobb angle | 1.000 | – | – | – | – | – | – | – | |||
| Apical axial rotation | −0.310 | 0.455 | 1.000 | – | – | – | – | – | |||
| TK | −0.330 | 0.425 | −0.468 | 0.243 | 1.000 | – | – | – | |||
| LL | 0.165 | 0.695 | −0.735 | 0.038* | 0.532 | 0.175 | 1.000 | – | |||
| Post-op | |||||||||||
| Coronal Cobb angle | 1.000 | – | – | – | – | – | – | – | |||
| Apical axial rotation | 0.209 | 0.619 | 1.000 | – | – | – | – | – | |||
| TK | 0.768 | 0.026* | 0.014 | 0.974 | 1.000 | – | – | – | |||
| LL | 0.489 | 0.219 | 0.140 | 0.741 | 0.322 | 0.437 | 1.000 | – | |||
| 1-year follow-up | |||||||||||
| Coronal Cobb angle | 1.000 | – | – | – | – | – | – | – | |||
| Apical axial rotation | 0.120 | 0.776 | 1.000 | – | – | – | – | – | |||
| TK | 0.739 | 0.036* | −0.216 | 0.608 | 1.000 | – | – | – | |||
| LL | 0.339 | 0.411 | −0.011 | 0.979 | 0.509 | 0.197 | 1.000 | – | |||
| 2-year follow-up | |||||||||||
| Coronal Cobb angle | 1.000 | – | – | – | – | – | – | – | |||
| Apical axial rotation | −0.776 | 0.024* | 1.000 | – | – | – | – | – | |||
| TK | 0.257 | 0.539 | −0.705 | 0.051 | 1.000 | – | – | – | |||
| LL | −0.143 | 0.735 | −0.385 | 0.347 | 0.868 | 0.005** | 1.000 | – | |||
*, significant (P<0.05); **, significant (P<0.01). VBT, vertebral body tethering; Pre-op, preoperative; Post-op, postoperative; TK, thoracic kyphosis; LL, lumbar lordosis; R, Pearson correlation coefficient; Sig., significance.
Tether breakage
Six out of 8 subjects had radiological tether breakage, all were clinically asymptomatic and not affecting daily activities or regular sports. Five of the tether breakages were after 2-year follow-up, 1 was at 15 months follow-up. The mean Cobb angle correction rate was 56.2% compared to preoperative angle. Four of the tether breakage subjects had mild apical axial deterioration ranging from 1.1°−5.4° (Table 1, Figure 1). Two remaining subjects had no tether breakage (Table 1). Notably, subject 3 with no tether breakage had the least correction rate in Cobb angle and greatest progression in apical axial rotation at 2-year follow-up compared to pre-op (Table 1, Figure 1).
Discussion
This study is the first to describe the progression of apical axial rotation in VBT subjects. At the 2-year follow-up, five out of eight subjects showed worsened axial rotation despite coronal correction, with subject 3 experiencing the greatest deterioration (as shown in Figure 1) and subject 6 with the least apical axial rotational changes (Figure 2). Notably, subject 3 (Figure 3), who had undergone the greatest apical axial rotational correction preoperatively, had a deterioration from −6.3° to −19.8°, while subject 1 (Figure 4) experienced an improvement from −11.6° to −3.4°. However, changes in axial rotation over time were highly variable between each subject and were not significant.


Previous PSF studies typically show improved apical axial rotation with sustained Cobb angle after surgery (34,35). One study interestingly highlighted derotation of 2.7° at 2-year follow-up, overlooking a significant 10° axial correction compared to preoperative angles in their PSF cohort (36). In contrast, our VBT subjects experienced apical derotation at 2-year follow-up compared to preoperative angles, despite significant corrections in the coronal Cobb angle over time. Furthermore, we found a significant negative correlation between the apical axial rotation and the coronal Cobb angle correction at the 2-year follow-up. Our result suggests that the coupling effect, where the correction of one spinal plane results in the spontaneous correction of other spinal planes, may not hold true in VBT subjects, despite previous findings in PSF (30). This underscores that VBT may not necessarily correct axial rotation to the same extent as coronal plane deformities, emphasizing the importance of assessing both spinal planes when evaluating treatment outcomes.
Regarding VBT tether breakage, a study suggested that breakage within the first year always leads to a loss of Cobb angle correction, while clinical impact is limited if breakage occurs after 1 year (32). Our study echoes; all breakages were asymptomatic, with Cobb angles remaining corrected by mean of 56.2% at 2-year follow-up. Notably, subject 3, without tether breakage, exhibited the most derotated apex compared to the preoperative angle, suggesting that axial rotation in VBT may be influenced by various factors. Unfortunately, the small number of subjects included in this study limits further analysis to identify factors contributing to axial plane corrections. These observations highlight the need for further comprehensive investigations to enhance the understanding of correction in AIS when VBT is the treatment of choice.
Previous studies have utilized scoliometer measurements to evaluate rib cage rotation post-VBT and have revealed improvements of up to 8° at the 2-year follow-up (13,27,29). However, it should be noted that the rib cage and spine do not rotate in the same way. In this study, 3D measurements of apical axial rotation were used to provide a more definitive and objective way of measuring changes at the vertebral level in VBT over time. This approach allows for a better understanding of the impact of VBT on spinal rotation and provides a more accurate assessment of treatment outcomes.
Consistent with earlier studies (11-25), we found that the correction of the coronal Cobb angle at the 2-year follow-up was consistent, and the sagittal parameters exhibited great stability. Specifically, the parameters for TK (15-17,19,21,24-27) and LL (13,17,24,25,27) only deviated by 5° and 7°, respectively, from established data, and by 2° and 4° from our study. Additionally, TK had normalized at the 2-year follow-up (27). The congruence of the coronal and sagittal parameters with established data strongly suggests that the axial plane measurements conform to acceptable standards, supporting the proposed association under investigation in this study.
Using 3D analysis of the spine after VBT allowed us to measure axial rotation in each vertebra, providing data that cannot be seen on daily biplanar radiographs. However, the small sample size and retrospective aspect of this study limit its generalizability. Further studies with larger cohorts and longer follow-up periods are necessary to better understand the effects of VBT on axial rotation.
Conclusions
In summary, this is the first study to show that apical axial rotation deteriorates in VBT subjects compared to pre-op at 2-year follow-up, while coronal Cobb angle shows improvement overtime at 2-year follow-up. The progression of apical axial rotation has revealed that VBT may not necessarily correct axial rotation to the same extent as coronal plane deformities and coupling effect may not hold true. While scoliometer measurements have been used in previous studies to assess rib cage rotation post-VBT, 3D measurements of apical axial rotation provide a more definitive and objective way of measuring changes at the vertebral level and offer a more accurate assessment of treatment outcomes. The present investigation has also found that the correction of the coronal Cobb angle at the 2-year follow-up is consistent with earlier studies, and the sagittal parameters exhibit remarkable stability. Tether breakage in VBT subjects was asymptomatic and not necessarily related to deteriorations in spinal parameters. However, the study is limited by its small sample size and retrospective nature. Further studies with larger cohorts and longer follow-up periods are needed to better understand the effects of VBT on axial rotation. Overall, this study highlights the importance of considering both spinal planes when assessing treatment outcomes in VBT subjects. Both surgeons and patients should be aware of such findings prior to selecting VBT as their treatment choice.
Acknowledgments
The authors would like to thank Ms. Lai Suet Wong for her kind assistance in digital measurements.
Funding: The research was supported by
Footnote
Reporting Checklist: The authors have completed the AME Case Series reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-24-59/rc
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-24-59/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-24-59/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional research committee of the University of Hong Kong / Hospital Authority Hong Kong West Cluster (approval number: 19-002) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients and their parents for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- De Smet AA, Asher MA, Cook LT, et al. Three-dimensional analysis of right thoracic idiopathic scoliosis. Spine (Phila Pa 1976) 1984;9:377-81. [Crossref] [PubMed]
- Kojima T, Kurokawa T. Quantitation of three-dimensional deformity of idiopathic scoliosis. Spine (Phila Pa 1976) 1992;17:S22-9. [Crossref] [PubMed]
- ROAF R. Rotation movements of the spine with special reference to scoliosis. J Bone Joint Surg Br 1958;40-B:312-32. [Crossref] [PubMed]
- Stokes IA, Bigalow LC, Moreland MS. Three-dimensional spinal curvature in idiopathic scoliosis. J Orthop Res 1987;5:102-13. [Crossref] [PubMed]
- Somerville EW. Rotational lordosis; the development of single curve. J Bone Joint Surg Br 1952;34-B:421-7. [Crossref] [PubMed]
- Roaf R. The basic anatomy of scoliosis. J Bone Joint Surg Br 1966;48:786-92.
- Brink RC, Homans JF, Schlösser TPC, et al. CT-based study of vertebral and intravertebral rotation in right thoracic adolescent idiopathic scoliosis. Eur Spine J 2019;28:3044-52. [Crossref] [PubMed]
- Little JP, Izatt MT, Labrom RD, et al. Investigating the change in three dimensional deformity for idiopathic scoliosis using axially loaded MRI. Clin Biomech (Bristol, Avon) 2012;27:415-21. [Crossref] [PubMed]
- Wong DLL, Mong PT, Ng CY, et al. Can anterior vertebral body tethering provide superior range of motion outcomes compared to posterior spinal fusion in adolescent idiopathic scoliosis? A systematic review. Eur Spine J 2023;32:3058-71. [Crossref] [PubMed]
- Crawford CH 3rd, Lenke LG. Growth modulation by means of anterior tethering resulting in progressive correction of juvenile idiopathic scoliosis: a case report. J Bone Joint Surg Am 2010;92:202-9. [Crossref] [PubMed]
- Newton PO, Takahashi Y, Yang Y, et al. Anterior vertebral body tethering for thoracic idiopathic scoliosis leads to asymmetric growth of the periapical vertebrae. Spine Deform 2022;10:553-61. [Crossref] [PubMed]
- Mathew SE, Hargiss JB, Milbrandt TA, et al. Vertebral body tethering compared to posterior spinal fusion for skeletally immature adolescent idiopathic scoliosis patients: preliminary results from a matched case-control study. Spine Deform 2022;10:1123-31. [Crossref] [PubMed]
- Samdani AF, Pahys JM, Ames RJ, et al. Prospective Follow-up Report on Anterior Vertebral Body Tethering for Idiopathic Scoliosis: Interim Results from an FDA IDE Study. J Bone Joint Surg Am 2021;103:1611-9. [Crossref] [PubMed]
- Wong HK, Ruiz JNM, Newton PO, et al. Non-Fusion Surgical Correction of Thoracic Idiopathic Scoliosis Using a Novel, Braided Vertebral Body Tethering Device: Minimum Follow-up of 4 Years. JB JS Open Access 2019;4:e0026.
- Newton PO, Kluck DG, Saito W, et al. Anterior Spinal Growth Tethering for Skeletally Immature Patients with Scoliosis: A Retrospective Look Two to Four Years Postoperatively. J Bone Joint Surg Am 2018;100:1691-7. [Crossref] [PubMed]
- Newton PO, Bartley CE, Bastrom TP, et al. Anterior Spinal Growth Modulation in Skeletally Immature Patients with Idiopathic Scoliosis: A Comparison with Posterior Spinal Fusion at 2 to 5 Years Postoperatively. J Bone Joint Surg Am 2020;102:769-77. [Crossref] [PubMed]
- Miyanji F, Pawelek J, Nasto LA, et al. Safety and efficacy of anterior vertebral body tethering in the treatment of idiopathic scoliosis. Bone Joint J 2020;102-B:1703-8. [Crossref] [PubMed]
- Hoernschemeyer DG, Boeyer ME, Robertson ME, et al. Anterior Vertebral Body Tethering for Adolescent Scoliosis with Growth Remaining: A Retrospective Review of 2 to 5-Year Postoperative Results. J Bone Joint Surg Am 2020;102:1169-76. [Crossref] [PubMed]
- Mackey C, Hanstein R, Lo Y, et al. Magnetically Controlled Growing Rods (MCGR) Versus Single Posterior Spinal Fusion (PSF) Versus Vertebral Body Tether (VBT) in Older Early Onset Scoliosis (EOS) Patients: How Do Early Outcomes Compare? Spine (Phila Pa 1976) 2022;47:295-302. [Crossref] [PubMed]
- Baker CE, Kiebzak GM, Neal KM. Anterior vertebral body tethering shows mixed results at 2-year follow-up. Spine Deform 2021;9:481-9. [Crossref] [PubMed]
- Baroncini A, Courvoisier A, Berjano P, et al. The effects of vertebral body tethering on sagittal parameters: evaluations from a 2-years follow-up. Eur Spine J 2022;31:1060-6. [Crossref] [PubMed]
- Miyanji F, Fields MW, Murphy J, et al. Shoulder balance in patients with Lenke type 1 and 2 idiopathic scoliosis appears satisfactory at 2 years following anterior vertebral body tethering of the spine. Spine Deform 2021;9:1591-9. [Crossref] [PubMed]
- Mishreky A, Parent S, Miyanji F, et al. Body mass index affects outcomes after vertebral body tethering surgery. Spine Deform 2022;10:563-71. [Crossref] [PubMed]
- Yucekul A, Akpunarli B, Durbas A, et al. Does vertebral body tethering cause disc and facet joint degeneration? A preliminary MRI study with minimum two years follow-up. Spine J 2021;21:1793-801. [Crossref] [PubMed]
- Rushton PRP, Nasto L, Parent S, et al. Anterior Vertebral Body Tethering for Treatment of Idiopathic Scoliosis in the Skeletally Immature: Results of 112 Cases. Spine (Phila Pa 1976) 2021;46:1461-7. [Crossref] [PubMed]
- Courvoisier A, Baroncini A, Jeandel C, et al. Vertebral Body Tethering in AIS Management-A Preliminary Report. Children (Basel) 2023;10:192. [Crossref] [PubMed]
- Samdani AF, Ames RJ, Kimball JS, et al. Anterior vertebral body tethering for idiopathic scoliosis: two-year results. Spine (Phila Pa 1976) 2014;39:1688-93. [Crossref] [PubMed]
- Stagnara P, De Mauroy JC, Dran G, et al. Reciprocal angulation of vertebral bodies in a sagittal plane: approach to references for the evaluation of kyphosis and lordosis. Spine (Phila Pa 1976) 1982;7:335-42. [Crossref] [PubMed]
- Pehlivanoglu T, Oltulu I, Ofluoglu E, et al. Thoracoscopic Vertebral Body Tethering for Adolescent Idiopathic Scoliosis: A Minimum of 2 Years' Results of 21 Patients. J Pediatr Orthop 2020;40:575-80. [Crossref] [PubMed]
- Luk KD, Vidyadhara S, Lu DS, et al. Coupling between sagittal and frontal plane deformity correction in idiopathic thoracic scoliosis and its relationship with postoperative sagittal alignment. Spine (Phila Pa 1976) 2010;35:1158-64. [Crossref] [PubMed]
- Ilharreborde B, Steffen JS, Nectoux E, et al. Angle measurement reproducibility using EOS three-dimensional reconstructions in adolescent idiopathic scoliosis treated by posterior instrumentation. Spine (Phila Pa 1976) 2011;36:E1306-13. [Crossref] [PubMed]
- Baroncini A, Migliorini F, Eschweiler J, et al. The timing of tether breakage influences clinical results after VBT. Eur Spine J 2022;31:2362-7. [Crossref] [PubMed]
- Wan SHT, Guldeniz O, Yeung MHY, et al. Inter-screw index as a novel diagnostic indicator of tether breakage. Spine Deform 2023;11:887-95. [Crossref] [PubMed]
- Pasha S, Flynn JM, Sponseller PD, et al. Timing of Changes in Three-Dimensional Spinal Parameters After Selective Thoracic Fusion in Lenke 1 Adolescent Idiopathic Scoliosis: Two-Year Follow-up. Spine Deform 2017;5:409-15. [Crossref] [PubMed]
- Faldini C, Perna F, Geraci G, et al. Triplanar correction of adolescent idiopathic scoliosis by asymmetrically shaped and simultaneously applied rods associated with direct vertebral rotation: clinical and radiological analysis of 36 patients. Eur Spine J 2018;27:165-74. [Crossref] [PubMed]
- Cui G, Watanabe K, Nishiwaki Y, et al. Loss of apical vertebral derotation in adolescent idiopathic scoliosis: 2-year follow-up using multi-planar reconstruction computed tomography. Eur Spine J 2012;21:1111-20. [Crossref] [PubMed]


