
Lumbar total disk replacement versus microsurgical lumbar discectomy in treatment of radicular and back pain in railway workers: a prospective randomized controlled trial
Introduction
One of the leading causes of disability worldwide is low back pain and sciatica (1). Lumbar disk herniation (LDH) is often accompanied by pain in the back and lower extremities (2).
In cases of ineffectiveness of conservative therapy, a microsurgical lumbar discectomy (MLD) using to remove prolapsed or extruded disc fragment and decompress the symptomatic nerve (3). It was found that after lumbar discectomy have risk for loss of disc height, foraminal stenosis with postoperative radiculopathy and reoperation associated with recurrent herniation (4,5). Thus, revision surgery for recurrent disc herniations is predominantly fusion surgery (4). So, high rate of LDH patients at 1 year after spinal surgery expressed unhappiness with the level of pain (6).
Rigid spinal fusion is frequently considered as one of the preferred methods of surgical treatment for patients with lumbar degenerative diseases (7). Fusion techniques reduce pain by restricting the abnormal motion, reducing instability, and restoring spinal alignment (8). However, rigid fixation of a spinal segment is considered to be one of the risk factors that may lead to accelerated degeneration of the adjacent level associated with increase intradiscal pressure (9).
The lumbar total disk replacement (TDR) in surgical treatment of degenerative disk disease is a known alternative to fusion interventions in specific cases (10). This technology preserves natural biomechanics, maintains physiological movements and reduces the risk of degeneration of the adjacent segment degenerative disease (11). With correct selection of patients and indications for lumbar TDR may have better clinical outcomes compared to the fusion (12).
It is well recognized that heavy physical work may contribute to the development of degenerative changes in the lumbar spine segments (13). This leads to acceleration of degenerative disk disease with the development of clinical compression symptoms, which reduces the preoperative workload of Railway workers (14). The ability to maintain tolerance to intense physical activity with the restoration of previous professional activities is important for this category of patients (15).
In this study, we conducted a prospective, blinded, and randomized trial to determine 1-year results of clinical effectiveness and return to work rate (RWR) after lumbar TDR and MLD in railway workers with LDH. Clinical and radiographic observers were blinded for the assigned treatment during the 12-month follow-up. We present this article in accordance with the CONSORT reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-24-63/rc).
Methods
Patient population
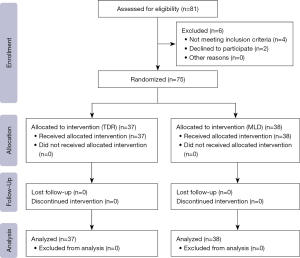
We performed a randomized prospective controlled clinical study, in which 75 patients out of a total of 81 patients, 49 men and 26 women aged 25–35 years with one-level LDH were eligible to participate, and were enrolled from March 2021 and August 2022 (Figure 1) to undergo TDR and MLD by a surgical team in Center for Neurosurgery of the Irkutsk Railway Clinical Hospital. Patients who met the inclusion criteria were randomized to single-level TDR surgery (group I) or MLD surgery (group II). Randomization was carried out using a web-based system for computer-generated random treatment assignment in a 1:1 ratio. The study was approved by the Ethics Committee of the Irkutsk State Medical University (No. 1, dated February 24, 2021). Irkutsk Railway Clinical Hospital is a clinical base for the Department of Neurosurgery and a University hospital for the Irkutsk State Medical University. Each patient gave voluntary consent to be included in the study. The analysis of the clinical material was carried out in accordance with the principles of the Declaration of Helsinki (as revised in 2013). The patients’ data used to support the findings of this study are restricted by the Ethics Committee of Irkutsk State Medical University in order to protect of the patient privacy. Data are available from the corresponding author (V.A.B., byval75vadim@yandex.ru) for researchers who meet the criteria for access to confidential data. And this study was registered in the Russian Clinical Trial Registry (http://rosrid.ru/) with the identifier 622011400059-4.
Surgical techniques
One primary surgeon (V.A.B.) performed TDR and MLD.
Two study groups were identified: in the TDR-group (n=37) we used total discectomy with bilateral foraminotomy and mandatory resection of the posterior longitudinal ligament from the left-sided pararectal extraperitoneal approach was performed. A prosthesis “M6-L” (Spinal Kinetics, Switzerland, no conflict interest) was used, consisting of ultra-high-molecular-weight polyethylene fibers wound in multiple redundant layers around a polycarbonate urethane polymer core and through titanium alloy endplates with keels to provide fixation to the superior and inferior vertebral bodies. In the MLD-group (n=38), intervention was performed from the interlaminar intermuscular approach, ligamentum flavum was excised, after dissection of adhesions, the microsurgical discectomy with nucleus pulposus removal was performed. Nerve root pulsation and its free displacement indicated adequate discectomy.
Eligible patients were discogenic back pain in addition to lumbar radiculopathy, persistent radicular pain syndrome, resistant to conservative therapy for 6–8 weeks (as a conservative treatment using non-narcotic analgesics, muscle relaxants, vitamins, epidural blockade with steroids, physiotherapy), LDH in the segments L4–L5 or L5–S1 without disk migrations on preoperative magnetic resonance imaging (MRI): type “root compression” according to van Rijn classification system and “lumbar disk extrusion” according to Combined Task Force (CTF) classification system (16). At the same time, disc herniation has a collar with a disc quite good (crack), I–II grade of intervertebral disk (IVD) according to Pfirrmann et al. (17), I–II grade of facet joints (FJs) according to Fujiwara et al. (18), preservation of the height of the interbody space—more than 50% of the overlying one, no signs of segmental instability in the functional spinal unite (FSU)—Slip Percentage >15%, Dynamic Slip >4.5 mm, Dynamic Segmental Angle >20° (L4–L5) and >25° (L5–S1), no signs of posterior osteophytes.
Patients presenting with LDH in the segments L4–L5 or L5–S1 with disk migrations on preoperative MRI, type “no root compression, possibly no root compression, indeterminate root compression, possible root compression” according to van Rijn classification system and “normal lumbar disk, focal protrusion, broad-based protrusion” according to CTF classification system (16), previously lumbar spinal surgery, osteoporosis, competing pathological process in the lumbar spine (traumatic injuries, systemic connective tissue diseases, infectious and inflammatory diseases, tumor lesions, etc.), segmental instability, spondylarthrosis, decrease in the height of the interbody space—more than 50% of the overlying one, positive test with FJ blockade, spinal stenosis, and patients who refused to participate in the study were excluded.
Data analyzed
The demographic parameters obtained through a review of medical records included sex, age, body mass index.
All patients were assessed when they checked in for surgery, at the time of hospital discharge, and at follow-up appointments 3, 6, and 12 months after surgery. Patients completed a questionnaire at each follow-up appointment yielding their Oswestry Disability Index (ODI) score (19). The ODI score was considered the primary outcome. Pain severity was evaluated using the Visual Analog Scale (VAS) (20). Quality of life was studied according to SF-36 (21).
The criterion for the restoration of working capacity was the absence of pain and neurological disorders during the performance of physical activity loads with the restoration of the previous employment.
Workload intensity criteria were used to analyze return to work 1 year after surgery, which included sedentary, light-moderate and heavy-very heavy type of the workload (https://occupationalinfo.org). The number of days of disability required before returning to work after surgery was also analyzed.
Prior to surgical intervention and at the last postoperative follow-up X-ray assessment we analyzed: (I) range of motion (ROM); (II) general lumbar lordosis (GLL). MRI was also used to evaluate pre- and postoperative changes in the lumbar spine.
The analysis of data was carried out by two experts (neurosurgeon and radiologist) previously blinded to the patient’s information. Statistical evaluation of expert agreement on each issue was performed using Kappa statistics (Graph Pad Software, Inc., USA).
Statistical analysis
Statistical processing of the study results study was carried out on a personal computer using the Statistica 13.5 program. The necessary statistical power of the study and the number of cases in each group were calculated, and the ODI score was considered the main indicator of functional outcome. A minimum of 37 cases was needed in each group to achieve 80% statistical power, with P<0.05 as the 2-tailed level of significance indicating achievement of the minimum clinically significant 10-point difference in ODI score (standard deviation =15).
The character of the distribution of signs was evaluated by the Shapiro-Wilk, Kolmogorov-Smirnov and Lilliefors tests for normality. Considering the presence of statistically significant differences according to these tests (P<0.05), the distribution was considered to be different from normal. In this regard, the criteria of nonparametric statistics were used to assess the significance of the differences in the samples. The obtained results are presented by the median, the values of the 1st and 3rd quartiles—Me (Q25, Q75). For a comparative analysis of the obtained values, the Mann-Whitney U-test and the Wilcoxon criterion, the χ2 criterion for binomial signs were used.
Results
Seventy-five respondents (49 men and 26 women) who were operated on with either TDR and MLD were analyzed. General information about the study groups of patients is shown in Table 1. A comparative analysis found that the groups were representative of all the analyzed features. Comparative intergroup analysis of preoperative clinical data demonstrated no statistically significant differences for all parameters (P>0.05).
Table 1
| Criterion | TDR group (n=37) | MLD group (n=38) | P |
|---|---|---|---|
| Age (years) | 29 [23–36] | 27 [22–38] | 0.37 |
| Sex | 0.68 | ||
| Male | 25 (67.6) | 24 (63.2) | |
| Female | 12 (32.4) | 14 (36.8) | |
| Operation level | 0.73 | ||
| L4–L5 | 18 (48.6) | 17 (44.7) | |
| L5–S1 | 19 (51.4) | 21 (55.3) | |
| ASA score | 0.42 | ||
| I | 12 (32.4) | 10 (26.3) | |
| II | 14 (37.8) | 16 (42.1) | |
| III | 11 (29.7) | 12 (31.6) | |
| Smoking | 10 (27.0) | 8 (21.1) | 0.54 |
| Interbody height (mm) | 9.1 [7.8–9.7] | 9.2 [8.0–9.8] | 0.36 |
| Modic type | 0.73 | ||
| Modic type 1 | 20 (54.1) | 23 (60.5) | |
| Modic type 2 | 17 (45.9) | 15 (39.5) | |
| Pain syndrome, VAS (mm) | |||
| Lumbar spine | 82 [75–84] | 82 [78–88] | 0.15 |
| Lower limbs | 89 [83–92] | 92 [85–100] | 0.06 |
| Preoperative neurological symptoms | 0.17 | ||
| Motor deficit | 2 (5.4) | 3 (7.9) | |
| Sensory deficit | 23 (62.2) | 22 (57.9) | |
| Reflex changes | 28 (75.7) | 27 (71.1) | |
| Primary presenting complaint | 0.92 | ||
| Back pain | 18 (48.6) | 19 (50.0) | |
| Radiculopathy | 37 (100.0) | 38 (100.0) | |
| Functional state according to ODI score | 82 [74–88] | 80 [68–88] | 0.15 |
| SF-36 score | |||
| Physical component score | 24.51 [19.84–26.18] | 23.18 [20.56–25.99] | 0.69 |
| Mental component score | 23.44 [21.22–27.69] | 23.57 [20.71–26.72] | 0.92 |
| Preoperative workload | |||
| Sedentary | 5 (13.5) | 4 (10.5) | 0.69 |
| Light-medium | 15 (40.5) | 18 (47.4) | 0.55 |
| Heavy-very heavy | 17 (45.9) | 16 (42.1) | 0.73 |
Data are presented as Me [Q25–Q75] or n (%). TDR, total disc replacement; MLD, microsurgical lumbar discectomy; Me, median; ASA, American Society of Anaesthesiologists; mm, millimeters; VAS, Visual Analogue Scale; ODI, Oswestry Disability Index.
An intergroup comparison of intraoperative parameters and the specificity of the course of the postoperative period in the studied patients showed statistically lower duration of surgery in MLD group compared with TDR group: 50 [40, 65] vs. 90 [75, 135] min, respectively (P=0.01); the volume of blood loss 35 [20, 50] vs. 75 [50, 100] mL, respectively (P=0.03). At the same time, comparable parameters were registered between MLD group and TDR group: time to mobilization 1 [1, 2] vs. 1 [1, 2] days, respectively (P=0.96); the duration of inpatient treatment 2 [2, 3] vs. 2 [1, 3] days, respectively (P=0.14).
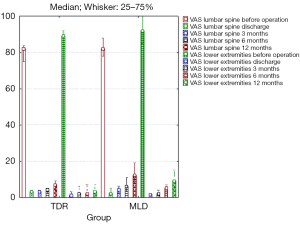
VAS scores (Figure 2) indicated considerable back pain and leg pain relief immediately after surgery (P<0.01) and remaining low thereafter. There was no difference at time point between back pain (discharge, P=0.28; 3 months, P=0.61) and leg pain scores (discharge, P=0.45; 3 months, P=0.58; 6 months, P=0.06). There was significantly lower back pain (6 months, P=0.005; 12 months, P<0.001) and leg pain (12 months, P<0.001) in the TDR group than in the MLD group.
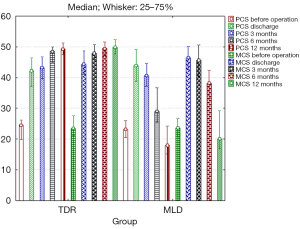
At discharge, ODI scores indicated highly significant improvement in patients’ quality of life in both groups (P<0.01) (Figure 3). There was no difference at time point in the patients’ ODI scores (discharge, P=0.96; 3 months, P=0.65). Intergroup comparison showed difference in the patients’ ODI scores across groups at 6 and 12 months after TDR group than in the MLD group (P=0.01, P<0.001, respectively).

Intergroup comparison showed better outcomes after TDR in comparison to MLD according to SF-36 at 6 and 12 months after surgery (Figure 4). There was no difference at time point between PCS (discharge, P=0.35; 3 months, P=0.10) and MCS (discharge, P=0.13). There was significantly higher PCS (6 months, P<0.001; 12 months, P<0.001) and MCS (3 months, P=0.01; 6 months, P<0.001; 12 months, P<0.001) in the TDR group than in the MLD group.
The inter-observer agreement for each of the measured radiological parameter was good and excellent according to Kappa statistics: Modic changes pre-operatively—0.950±0.14 [95% confidence interval (CI): 0.874–1.000], disc height pre-operatively—0.851±0.165 (95% CI: 0.762–0.941); ROM pre-operatively—0.729±0.142 (95% CI: 0.582–1.000), as well as post-operatively—0.908±0.082 (95% CI: 0.740–1.000); GLL pre-operatively—0.908±0.082 (95% CI: 0.740–1.000), as well as post-operatively—0.818±0.120 (95% CI: 0.584–1.000). Data are presented as kappa agreement ± standard error (95% CI).
The analysis showed a change in ROM from 5.9° (5.3°, 6.5°) to 8.3° (7.3°, 8.9°) (P<0.001) in TDR group and from 6.0° (5.1°, 6.7°) to 5.75° (5.1°, 6.3°) (P=0.04) in MLD group. There was no difference of the ROM before operation (P=0.88). Intergroup comparison showed better ROM across groups at 12 months after TDR group than in the MLD group (P<0.001).
At 12 months registered change of GLL from 38° (34°, 42°) to 39° (35°, 45°) (P=0.04) in TDR group and from 36° (32°, 40°) to 32° (30°, 38°) (P=0.38) in MLD group. There was no difference of the GLL before operation (P=0.29). Intergroup comparison showed difference of the GLL across groups at last follow-up after TDR group than in the MLD group (P=0.03).
After the operation, the patient began an active rehabilitation program, the same in both groups. In the 3rd week after the surgery, a home exercises were used; in the 5th week, low-intensity exercise started; in the 7th week, high-intensity exercise restarted.
The analysis revealed a comparable number of symptomatic complications in both groups (P=0.47), with a greater frequency of reoperations in the follow-up period in MLD group in comparison TDR group (P=0.04) (Table 2).
Table 2
| Parameter | TDR group (n=37) | MLD group (n=38) | P |
|---|---|---|---|
| Surgery complication | 0.47 | ||
| Nerve root injury | – | 1 | |
| Surgical site infection | 1 | 1 | |
| Postoperative hematoma | 1 | 1 | |
| Spondylodiscitis | – | 1 | |
| Transient partial urination disturbance | – | 1 | |
| Retrograde ejaculation | 1 | – | |
| Reoperation | 0.04 | ||
| Adjacent segment degeneration | 1 | 1 | |
| Herniation recurrence | – | 3 | |
| Segmental instability | – | 1 | |
| Severe facet syndrome | 1 | 3 |
TDR, total disc replacement; MLD, microsurgical lumbar discectomy.
Table 3 displays median time to return to work for the three workload groups based on the procedure. The sedentary, light-moderate and heavy-very heavy groups had no difference time to return to work after TDR and MLD group (P>0.05).
Table 3
| Criterion | TDR group (n=37) | MLD group (n=38) | P |
|---|---|---|---|
| Time to return to work | |||
| Sedentary, Me [Q25–Q75] | 44 [37–58] | 40 [35–53] | 0.74 |
| Light-medium, Me [Q25–Q75] | 56 [46–67] | 51 [42–64] | 0.41 |
| Heavy-very heavy, Me [Q25–Q75] | 72 [64–91] | 70 [61–90] | 0.83 |
| Return to work rate | |||
| Sedentary, n (baseline/last follow-up), % | 5/5 (100.0) | 3/4 (75.0) | 0.23 |
| Light-medium, n (baseline/last follow-up), % | 15/15 (100.0) | 11/18 (61.1) | 0.006 |
| Heavy-very heavy, n (baseline/last follow-up), % | 15/17 (88.2) | 9/16 (56.25) | 0.01 |
TDR, total disc replacement; MLD, microsurgical lumbar discectomy; Me, median.
After TDR, the RWR 1 year after surgery was 94.6% and for MLD group was 60.5%—35 patients and 23 patients, respectively. In a comparative analysis, depending on the workload, a statistically significantly higher RWR was found after TDR compared with MLD in light-moderate and heavy-very heavy groups (P<0.05).
Discussion
High intensity workloads on the spine experienced by railway workers contribute to formation and acceleration of degeneration processes in the lumbar segments (14). This leads to the formation of LDH, deformities and segmental instability associated with persistent radicular neurological manifestations requiring surgical treatment (15).
MLD has relatively high clinical efficacy in the population due to the minimal trauma of the surgical procedure (3). It has been established that limited discectomy increases the risk of recurrent disc herniation, while more total removal of the IVD is associated with collapse of the interbody space, foraminal stenosis with compression of the nerve roots, or symptomatic facet syndrome (22).
Fusion surgery is common procedure of surgical treatment various lumbar spine degenerative diseases (23). At the same time, rigid fixation of the operated segments, are associated with limited mobility of the lumbar spine and changes in the kinematics of the spine as a whole (24). The use of artificial prosthesis that imitates the biomechanics of a normal IVD made it possible to achieve good clinical results and maintain physiological mobility to respondents in the shortest possible time (25). Thus, TDR is offered to the patient, to prevent a possible worsening of the disc condition and its tolerance. TDR techniques have been associated with early functional recovery, better clinical outcome and decreased postoperative pain than fusion surgery (26). The TDR only repairs damage to the disc and not the posterior elements directly. The argument that “M6-L” TDR fixing only the damaged part of the lumbar segment (disc rupture) needs to be highlighted. Thus, any lumbar TDR treatment should be compared to a discectomy rather than an internal stabilization and fusion on this biomechanical basis.
Railway workers—a cohort of patients with a high preoperative level of physical activity, motivated by a rapid professional recovery (14,27). Maintaining performance is the dominant reason for preventing the development of psychological, social and financial consequences (28). To our knowledge, this is the first study to report the rate and the time to return to work based on workload intensity in railway workers who have undergone one-level TDR versus MLD.
Studies describing recovery as a function of workload intensity are sparse. According to Singh et al. (29), 1 year after non-fusion surgery RWR were sedentary (87%), light-medium (86%) and heavy-very heavy (80%). Median time to return to work were sedentary (41 days), light-medium (52 days) and heavy-very heavy (71 days).
Significant physical activity at work prolongs return to work and duration of disability (30). This influences spinal surgeons’ choice of recovery recommendations to withstand workloads depending on the type of surgery and workplace requirements (31). For non-fusion procedures, most surgeons recommended 2–6 weeks off work before returning to a sedentary to light-moderate workload job and 7–12 weeks off work for a heavy-very heavy workload job (29).
To our knowledge, this is the first study to compare TDR and MLD procedures on clinical outcomes and recovery time in Railway workers. In addition, in the specialized literature we have not encountered studies comparing the results of TDR and MLD procedures in patients with single-level LDH. We understand that performing lumbar TDR is beyond the scope outside of the standard of care, but according to our data, the expansion of surgical aggression is justified by better clinical outcomes, higher RWR and lower frequency of reoperations compared with microdiscectomy 12 months after surgery in railway workers. Thus, we have expanded the indications for performing TDR for herniated lumbar intervertebral discs in patients with radicular pain syndrome to prevent possible deterioration of the disc condition and restore tolerance to heavy physical exertion. The higher rate of complications after microdiscectomy found in the study, which is not consistent with clinical series published in the literature, is most likely due to the high intensity of work and physical activity of railway workers. Therefore, we believe that in this cohort of patients with discogenic back pain in addition to lumbar radiculopathy, the primary treatment of lumbar TDR would be a better option. At the same time, we must remember that the TDR is a major surgery compared to MLD. To obtain a good result the surgeon has to be trained to this surgery: approach, management of great vessels, section of posterior longitudinal ligament, controlled to distraction of disc space, size, angle and centering of the prosthesis etc. All of these skills may be unavailable or difficult for the average spinal surgeon, so if the specialist is not sufficiently trained, complications from TDR can be much more dangerous and serious than from MLD.
We found that some VAS and ODI parameters were comparable between the analyzed groups at discharge and in the period of 3–6 months after surgery. We believe that both surgical procedures provide effective removal of LDH and decompression of the nerve root. However, after 3–12 months, against the background of intense physical activity, complications associated with the progression of degenerative changes in the IVD with reherniation, as well as a decrease in the height of the interbody height with foraminal stenosis and repeated compression of the nerve root after MLD develop.
TDR and MLD procedures for single-level LDH had comparable number of surgical complications (P=0.47) and time to return to work (P>0.05). The use of TDR compared favorably to MLD with improved last follow up ODI (P<0.001), back pain (P<0.001), leg pain (P<0.001), SF-36 (P<0.001), as well as restoration of ROM (P<0.001), preservation of GLL (P<0.001) and lower rate of additional surgery procedures (P=0.04). After TDR procedure in light-moderate and heavy-very heavy workload patients groups had a statistically significantly higher RWR compared with MLD (P<0.05).
Strengths and limitations
The main limitations of this study were: (I) single center nature of the study; (II) this study primarily composed of a unique, relatively homogeneous population of railway workers with risky strenuous labor responsibilities; (III) relatively short follow-up period of 1 year; (IV) we did not analyze any other decompression and decompression-stabilization techniques; (V) we included only patients who were working preoperatively; (VI) information on post-operative rehabilitation and overall post-operative management were not available so the effect of rehabilitation could not be included.
Given the level of physical demand, the young age of the subjects, relatively short 12 months follow-up period and the particular artificial disc implant that was used, we planned follow these patient cohorts for annual evaluations and report longer-term outcomes.
Despite these limitations, the strengths of the study include its 1-year follow-up on a large population of patients, recruited randomly, with a single diagnosis, treated by a single team without numerous confounding variables.
Conclusions
The results showed that lumbar TDR and MLD are highly effective in improving clinical results 1 year follow-up in railway workers. However, the TDR technique has statistically significant advantages in terms of the dynamics of the level of leg pain, restoration of the functional state and quality of life compared to MLD at last follow up period in patients with radicular and back pain. In addition, after lumbar TDR, there was a higher RWR in light-moderate and heavy-very heavy groups, which is most likely associated with restoration of segmental mobility, preservation of global lumbar lordosis and lower reoperations compared with MLD in patients with lumbar disc herniations and moderate loss of the disc height.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-24-63/rc
Data Sharing Statement: Available at https://jss.amegroups.com/article/view/10.21037/jss-24-63/dss
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-24-63/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-24-63/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of Irkutsk State Medical University (No. 1, dated February 24, 2021). All patients were anonymized. Each patient gave voluntary consent to be included in the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- GBD 2016 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1260-344. [Crossref] [PubMed]
- Jensen RK, Kongsted A, Kjaer P, et al. Diagnosis and treatment of sciatica. BMJ 2019;367:l6273. [Crossref] [PubMed]
- Mehendiratta D, Patel P, Bhambhu V, et al. Effect of Preoperative Parameters on Outcomes of Lumbar Microdiscectomy: A Retrospective Analysis. Asian J Neurosurg 2022;17:248-54. [Crossref] [PubMed]
- Koivunen K, Pernaa KI, Saltychev M. Back pain and radicular pain after lumbar microdiscectomy. BMC Surg 2023;23:210. [Crossref] [PubMed]
- Miller LE, McGirt MJ, Garfin SR, et al. Association of Annular Defect Width After Lumbar Discectomy With Risk of Symptom Recurrence and Reoperation: Systematic Review and Meta-analysis of Comparative Studies. Spine (Phila Pa 1976) 2018;43:E308-15. [Crossref] [PubMed]
- Fekete TF, Haschtmann D, Kleinstück FS, et al. What level of pain are patients happy to live with after surgery for lumbar degenerative disorders? Spine J 2016;16:S12-8. [Crossref] [PubMed]
- Yingsakmongkol W, Jitpakdee K, Varakornpipat P, et al. Clinical and Radiographic Comparisons among Minimally Invasive Lumbar Interbody Fusion: A Comparison with Three-Way Matching. Asian Spine J 2022;16:712-22. [Crossref] [PubMed]
- Pradeep K, Pal B. Biomechanical and clinical studies on lumbar spine fusion surgery: a review. Med Biol Eng Comput 2023;61:617-34. [Crossref] [PubMed]
- Ebrahimkhani M, Arjmand N, Shirazi-Adl A. Adjacent segments biomechanics following lumbar fusion surgery: a musculoskeletal finite element model study. Eur Spine J 2022;31:1630-9. [Crossref] [PubMed]
- Bai DY, Liang L, Zhang BB, et al. Total disc replacement versus fusion for lumbar degenerative diseases - a meta-analysis of randomized controlled trials. Medicine (Baltimore) 2019;98:e16460. [Crossref] [PubMed]
- Rossi V, Maalouly J, Choi JYS. Lumbar arthroplasty for treatment of primary or recurrent lumbar disc herniation. Int Orthop 2023;47:1071-7. [Crossref] [PubMed]
- Zigler J, Gornet MF, Ferko N, et al. Comparison of Lumbar Total Disc Replacement With Surgical Spinal Fusion for the Treatment of Single-Level Degenerative Disc Disease: A Meta-Analysis of 5-Year Outcomes From Randomized Controlled Trials. Global Spine J 2018;8:413-23. [Crossref] [PubMed]
- Videman T, Battié MC. The influence of occupation on lumbar degeneration. Spine (Phila Pa 1976) 1999;24:1164-8. [Crossref] [PubMed]
- Khan MR, Singh NK. Prevalence of musculoskeletal disorders among Indian railway sahayaks. Int J Occup Environ Health 2018;24:27-37. [Crossref] [PubMed]
- Belykh E, Giers MB, Preul MC, et al. Prospective Comparison of Microsurgical, Tubular-Based Endoscopic, and Endoscopically Assisted Diskectomies: Clinical Effectiveness and Complications in Railway Workers. World Neurosurg 2016;90:273-80. [Crossref] [PubMed]
- Li Y, Fredrickson V, Resnick DK. How should we grade lumbar disc herniation and nerve root compression? A systematic review. Clin Orthop Relat Res 2015;473:1896-902. [Crossref] [PubMed]
- Pfirrmann CW, Metzdorf A, Zanetti M, et al. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 2001;26:1873-8. [Crossref] [PubMed]
- Fujiwara A, Lim TH, An HS, et al. The effect of disc degeneration and facet joint osteoarthritis on the segmental flexibility of the lumbar spine. Spine (Phila Pa 1976) 2000;25:3036-44. [Crossref] [PubMed]
- Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976) 2000;25:2940-52; discussion 2952. [Crossref] [PubMed]
- Bielewicz J, Daniluk B, Kamieniak P. VAS and NRS, Same or Different? Are Visual Analog Scale Values and Numerical Rating Scale Equally Viable Tools for Assessing Patients after Microdiscectomy? Pain Res Manag 2022;2022:5337483. [Crossref] [PubMed]
- Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473-83.
- Belykh E, Krutko AV, Baykov ES, et al. Preoperative estimation of disc herniation recurrence after microdiscectomy: predictive value of a multivariate model based on radiographic parameters. Spine J 2017;17:390-400. [Crossref] [PubMed]
- Bamps S, Raymaekers V, Roosen G, et al. Lateral Lumbar Interbody Fusion (Direct Lateral Interbody Fusion/Extreme Lateral Interbody Fusion) versus Posterior Lumbar Interbody Fusion Surgery in Spinal Degenerative Disease: A Systematic Review. World Neurosurg 2023;171:10-8. [Crossref] [PubMed]
- Toivonen LA, Mäntymäki H, Häkkinen A, et al. Postoperative Sagittal Balance Has Only a Limited Role in the Development of Adjacent Segment Disease After Lumbar Spine Fusion for Degenerative Lumbar Spine Disorders: A Subanalysis of the 10-year Follow-up Study. Spine (Phila Pa 1976) 2022;47:1357-61. [Crossref] [PubMed]
- Byvaltsev VA, Kalinin AA, Aliyev MA, et al. Clinical-Instrumental Results and Analysis of Functional Activity Restoration in Professional Athletes After Lumbar Total Disk Replacement. World Neurosurg 2021;151:e1069-77. [Crossref] [PubMed]
- Li YZ, Sun P, Chen D, et al. Artificial Total Disc Replacement Versus Fusion for Lumbar Degenerative Disc Disease: An Update Systematic Review and Meta-Analysis. Turk Neurosurg 2020;30:1-10. [Crossref] [PubMed]
- Byvaltsev VA, Kalinin AA, Pestryakov YY, et al. Prospective Randomized Comparison of Minimally Invasive Tlif versus Open Tlif: Clinical Effectiveness and Restoration of Working Capacity in Railway Workers. Global Spine J 2024; Epub ahead of print. [Crossref]
- Ji FL, Liu ZM, Liu ZS, et al. Mental health status in railway female workers and its occupational influencing factors. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2018;36:102-5. [Crossref] [PubMed]
- Singh S, McIntosh G, Dea N, et al. Effects of Workload on Return to Work After Elective Lumbar Spine Surgery. Global Spine J 2024;14:420-8. [Crossref] [PubMed]
- Schaafsma FG, Whelan K, van der Beek AJ, et al. Physical conditioning as part of a return to work strategy to reduce sickness absence for workers with back pain. Cochrane Database Syst Rev 2013;2013:CD001822. [Crossref] [PubMed]
- Russo F, Papalia GF, Vadalà G, et al. The Effects of Workplace Interventions on Low Back Pain in Workers: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health 2021;18:12614. [Crossref] [PubMed]


