
Robot-assisted minimally invasive transforaminal interbody fusion: a complete workflow pilot feasibility study
Highlight box
Key findings
• Our case series has shown high pedicle screw and transforaminal interbody cage insertion accuracy with the Mazor™ X Stealth Edition (Medtronic, Sofamor Danek USA) robotic-arm platform.
• There is also low complication rates comparable to that of conventional minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) O-arm navigation system.
What is known and what is new?
• Current literature regarding the use of robotic-assisted technology in spine surgery is scarce, and revolves largely around pedicle screw insertion. Multiple studies have shown higher screw accuracy and similar complication rates with robot-assisted surgeries, yet data on overall patient outcome measures are limited.
• Our study will be the first to describe a surgical workflow for MIS-TLIF procedure utilising the Mazor™ X Stealth Edition robotic arm navigation for the planning and insertion of the interbody cage. The clinical safety and cost-effectiveness of robot-assisted systems has still yet to be proven over conventional computer O-arm navigation in this study.
What is the implication, and what should change now?
• Potential system-related pitfalls such as instrument skiving, navigation errors still exist with the current Mazor™ X Stealth robotic-arm system.
• The discerning surgeon should be on the lookout for potential system-related pitfalls, as well as understand the limitations for robotic interbody cage placement.
• A high learning curve is required with robot-assisted navigation to achieve comparable surgical timings to conventional computer-navigation system.
• Larger sample size comparative studies will be required to achieve greater statistical significance, with emphasis on patient outcomes to warrant its high acquisition and maintenance costs.
Introduction
The increasing prevalence of degenerative lumbar spine conditions has been reported in developed societies with ageing populations. One commonly used surgical approach involves spinal decompression with fusion, via the transforaminal lumbar interbody fusion (TLIF) approach (1). Minimally invasive TLIF surgery (MIS-TLIF) has been developed with the advent of computer-assisted navigation and to increase screw placement accuracy and smaller incisions, leading to less post-operative pain and bleeding, thus shortening length of hospital stay (2,3).
More recently, the advancement of robotic technology has pushed this further with the inclusion of planning software and robotic arm guidance, reporting improved accuracy of screw placement, efficiency and reduced radiation exposure (4). Current robotics on the market include the Renaissance (Medtronic, Denver, CO, USA), SpineAssist (Medtronic, Louisville, KY, USA), ROSA Spine (Zimmer Biomet, Warsaw, IN, USA), Excelsius GPS (Globus, Eagleville, PA, USA), and Mazor™ X Stealth Edition (Medtronic, Sofamor Danek USA, USA) (5).
Current literature regarding the use of robotic-assisted technology in spine surgery is scarce, and revolves largely around pedicle screw insertion. Our study will be the first to describe a surgical workflow for MIS-TLIF procedure utilising the Mazor™ X Stealth Edition robotic arm navigation for the planning and insertion of the interbody cage. We will also report on the results of our institution’s robotic MIS-TLIF case series, and describe some of the technical pearls and pitfalls. We present this article in accordance with the STROBE reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-24-70/rc).
Methods
This is a single-centre, single surgeon prospective case series of 29 patients who underwent elective robot-assisted TLIF (RA-TLIF) with Mazor™ X Stealth system in our institution. Patient age, gender, body mass index (BMI), Charlson Comorbidity Index (CCI), post-operative day 1 ambulation and hospital length of stay are collected. All intra-operative and post-operative complications are also reported.
Statistical analysis
Descriptive analysis on the aforementioned parameters are analysed using SPSS Statistics Package Version 26 (IBM, Armonk, NY, USA), including frequency, median, mean and standard deviation. The level of statistical significance was set to P<0.05 for all statistical analysis.
Ethical statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical approval was obtained from the Singhealth Centralised Institutional Review Board (No. 2023-2505). Informed consent from participating patients was not required as no patient identifiable data was used in this study per the terms of the Ethical Board approval.
Setting up the operating field and registration
The Mazor™ X Stealth Edition platform consists of the workstation equipped with a computer interface for surgical planning and a robotic surgical arm. The robot attaches to the Jackson table bedframe via a custom side-mount near the foot of the bed. The surgical arm has 2 optical cameras and 1 infrared camera that create the 3-define area. This allows the robotic software to calculate the safest and most efficient areas of interest for the planned screw trajectories. The robot also includes a sidearm capable of housing a sterile surgeon screen table.
The robotic arm is used with the patient in the prone position to facilitate placement of the reference marker—single posterior superior iliac spine (PSIS) Schanz pin, which is then securely attached to the bone mount bridge on the robot (Figure 1). A 3-defined scan is then performed on the surrounding by the infrared camera, marking out the operating field to avoid collision with the robotic arm. To enhance accurate visualisation by the infrared camera, the field is covered with sterile drapes including any fixtures such as a Mayo table (Figure 1). The registration process is then completed with the attachment of the star marker on the effector arm over the centre of the area of region, close to the patient’s body while avoiding skin contact. The star marker acts as reference array, with all 4 fiducials to be visualised during the O-arm scan. The O-arm is then draped and positioned to obtain a 3-dimensional fine-cut computed tomography (CT) scan (0.4–1 mm; mAs: 150 kv/130 mAs), which is then transmitted to the Mazor™ X Stealth workstation for surgical planning.

Surgical planning for pedicle screw and interbody cage placement
The Mazor™ Software locates the segment of interest, allowing image rotation to correct for any coronal or sagittal malalignment. It then calculates the optimal screw size and anatomic and alignment coordinates for screw placement, which then allows the surgeon to fine tune prior to screw placement (Figure 2). The interbody cage (Elevate™ Spinal System, Medtronic) is templated at the relevant disc levels using the pre-set template. The trajectory starts from the facet joint, crossing obliquely to the intervertebral disc midline, with the cage anterior tip resting on the anterior apophyseal ring (Figure 2).

Screw placement
Once planning is complete, the robotic arm is sent sequentially to the locations of screw trajectories, where the entry point is marked on the skin to plan the skin incision (Figure 3). The skin incision is made and the lumbar fascia is divided with electrocautery. The robotic effector arm is moved to the pedicle screw position and a navigated dilator is inserted through until it is docked on the facet joint. Once the entry point position is confirmed on the navigation screen, an outer cannula is railroaded over the dilator in the robotic arm, followed by removal of the dilator, creating a port for drilling and screw insertion. A 3-mm navigated drill is then mounted into the outer cannula to drill the pedicle to the 30-mm positive stop (Figure 3).
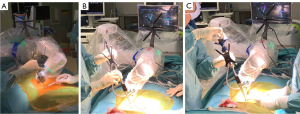
The drill is then removed and a navigated tap can then be inserted to tap the screw canal. The screw of pre-planned length and size is mounted on a navigated screw driver, which is then introduced into the robotic arm and inserted to the appropriate depth by hand (Figure 3). These steps are then repeated for each screw as pre-planned on the Mazor™ X Stealth software. However, on the ipsilateral side of the planned facetectomy and interbody cage insertion, a flexible 1-mm guidewire is placed temporarily into the tapped inferior pedicle. This is to prevent collision of the METRX™ tubes (Medtronic) against the screw tulip heads.
Interbody carpentry and cage placement
The robotic arm is directed towards the planned facetectomy site. A partial facetectomy is achieved with the navigated drill through the robotic arm under navigation. This is followed with the navigated dilator and sequential dilator tubes docked over the remaining facet to establish the 22-mm working port. The facetectomy is completed under the microscope using the high-speed burr and Kerrison punches, followed by flavum removal to expose Kambin’s triangle and the intervertebral disc space.
Discectomy is performed through an incised window on the annulus using up- and down-facing curettes and pituitary rongeurs. Resection of the nucleus and inner annulus is performed with caution not to breach the anterior annulus where the major vessels lie. A blunt ball-tipped probe is inserted into the neuroforamen to confirm adequate decompression of the nerve root and dural sac. The disc space is then irrigated with saline to remove any undetected disc fragment.
Navigated interbody fusion cage insertion
Gentle distraction of the disc space is performed using navigated dilators and shavers to the desired height which can be visualised on the robotic screen. The superior and inferior vertebral endplates are prepared with curette, excising its overlying cartilage, with care taken not to cause a fracture, especially in patients with indwelling osteoporosis. Bone graft material is then packed into disc space prior to cage insertion, using a funnel and temp. The robotic arm is moved to position over the cage insertion site. The pre-planned cage implant is then packed with bone allograft (demineralised bone matrix) and mounted on a navigated cage driver, which is then slotted into the robotic arm to guide its entry trajectory. The cage is then inserted into the disc space with gentle mallet taps to the appropriate depth as visualised on the navigation screen. The cage is then expanded to the earlier measured height using the attached 2.5 Nm torque handle to prevent endplate damage. The remaining screw is then inserted over the guidewire under navigation. The surgery is then completed with the insertion of the contoured rods and securing with locking caps through the percutaneous screw head sleeves. One final antero-posterior and later fluoroscopic check is then performed to confirm accurate placement of implants. This is followed by layered closure and optional drain insertion. Post-operatively, all patients were administered empirical intravenous antibiotic and oral analgesia as per hospital protocol. All patients were ambulated within 24 hours post-operatively. Prior to discharge, pedicle screw placement was qualitatively assessed using post-operative X-rays.
Results
The 27 included patients’ demographics and surgical outcomes are summarised in Tables 1,2. Two patients were pre-excluded from the study due to the Mazor™ X Stealth system startup failure and were converted to open/computer-assisted navigation. No intra-operative changes were recorded to the patients’ pre-operative neuro-monitoring. Mean operative time was 186.0±34.82 minutes for single-level and 245.0±41.68 minutes for two-level surgery. No intra-operative revision was required as all 116 robot-navigated screws and 31 interbody cages were placed in positions as planned on the robotic software on final intra-operative fluoroscopic checks. At 6-month follow-up, all implants remained in position with the exception of one migrated L3/4 interbody cage which was due to inaccurate sizing of the cage. This patient subsequently underwent revision surgery 3 months post-operatively (Table 3). No other post-operative complications such as infections, pulmonary embolism or cardiac complications were observed in this case series.
Table 1
| Variables | Values (N=27) |
|---|---|
| Age (years), mean ± SD | 67.7±12.63 |
| Body mass index (kg/m2), mean ± SD | 27.1±4.29 |
| Gender, n | |
| Male | 12 |
| Female | 15 |
| Length of stay (days), mean ± SD | 2.93±2.12 |
| Charlson Comorbidity Index | 4.00±2.45 |
| Intra-operative complications, n | |
| Implant related | 0 |
| Navigation issues | 1 |
| Durotomy | 0 |
RA-TLIF, robot-assisted minimally invasive transforaminal lumbar interbody fusion; SD, standard deviation.
Table 2
| Included cases | Surgery time (min) | Length of stay (days) | Post-op day 1 mobilisation (months) |
|---|---|---|---|
| One-level (n=23) | 186.0±34.82 | 2.91±2.24 | 37.61±24.88 |
| Two-level (n=4) | 245.0±41.68 | 3.0±1.22 | 37.5±14.79 |
Data are presented as mean ± standard deviation.
Table 3
| Complications at 90 days | N |
|---|---|
| Surgical site infection | 0 |
| Blood loss requiring transfusion | 0 |
| Long-term numbness/weakness | 0 |
| Malpositioned screw | 0 |
| Cage migration* | 1 |
| Surgical revision within 90 days* | 1 |
*, this patient who had cage migration underwent surgical revision within 90 days.
Discussion
This current Mazor™ X Stealth system is a shared-control system (6), simultaneously allowing both the surgeon and robot to control instruments and motions. Such a system can reduce the efforts in hand-eye coordination, complex movements required of the surgeon in traditional O-arm navigated TLIF. This is an upgrade of the Mazor SpineAssist® (Mazor Robotics Ltd., Caesarea, Israel), the first robot approved for spine surgery in the US, combined with the Stealthstation Surgical Navigation System for O-arm navigation. While this has been a great improvement on previous market offerings (7-9), it is not without its limitations (Table 4).
Table 4
| Advantages | Limitations |
|---|---|
| (I) Higher screw placement accuracy with planning software | (I) Longer set-up time for robotic arm |
| (II) Faster screw insertion time | (II) Potential for systematic errors with registration and navigation |
| (III) Risk of skiving during screw placement | |
| (IV) Rigidity of robotic arm, limiting it to minimally invasive approaches only | |
| (V) Limited planning capability for interbody fusion | |
| (VI) Not able to assist with decompressions or discectomy/interbody work |
RA-TLIF, robot-assisted minimally invasive transforaminal lumbar interbody fusion.
Currently, many different systems are available on the market and have been reported to have higher screw placement accuracy in comparison to conventional free-hand computer-navigation techniques. A systematic review by Liounakos et al. (7) reported 86.16% to 100% accuracy of robot-assisted screw placement, which are similar to our findings. In our study, all 116 screws inserted by robotic-guided navigation had satisfactory positions during intra-operative fluoroscopic checks, and also had no radiographic change in position at 6-month follow-up. There was no return to operating theatre for screw-related complications.
One of the cases encountered by the authors proved a challenge when the patient, whilst intubated, started coughing in between screw placement. This had caused a shift in patient position and the impaired the accuracy in robotic navigated insertion of the pre-planned pedicle screw. This is in part due to the reference fiducials (star marker) being attached to the robotic arm instead of directly on the patient’s body as with conventional O-arm navigation where the reference array is pinned to a bony landmark such as the iliac crest or an adjacent spinous process. The only direct reference of the patient’s positioning to the robotic arm is the single iliac crest Schanz pin via a coupler, while the main robotic arm unit is mounted on a side mount on the Jackson table. Even with a separate contralateral iliac crest Schanz pin attachment, it can still loosen and is still inadequate to negate or correct any movement in the patient’s spine, which can move independently from the pelvis.
Fortunately, the operating surgeon noticed the disparity of the landmark displayed on the surgical screen and the bony landmark on the patient prior to drilling. A repeat O-arm scan was performed and re-calibrated to the patient’s new position, with screw and interbody cage trajectory planning redone. The pedicle screws already inserted showed satisfactory position on the repeat O-arm scan and thus no implant revision was required. This highlights the importance of stabilising the reference fiducial position with respect to patient’s anatomy, as a key cornerstone to the accuracy of such platforms. Some potential solutions might lie in the other different options available by directly affixing the robotic arm to the patient’s spine, such as the spinous process clamp (single, dual or link bridge) (4). More body restraints and support during pre-operative positioning can potentially help reduce movement of the bony landmarks, but the effects will diminish in obese patients and pose risks of pressure sores.
In spine surgery, one of the common anaesthetic practices is total intravenous anaesthesia (TIVA) (10), with minimal muscle relaxant so as to allow effective motor-evoked potential neuromonitoring. Assistance from the anaesthetist to ensure deep enough anaesthesia to prevent intra-operative coughing (11).
Another potential issue highlighted by Buza et al. (4) was that of instrument skiving, even with the use of the robotic arm guide. Skive is a phenomenon described as a translational or angular change in position or trajectory of an instrument relative to its targeted bony landmark. In the case of lumbar pedicle screw insertion, skiving can occur when the surgeon introduces a translational force on the drill or screw driver down a steep slope of the lateral facet joint edge. Even with the navigation screen, minute instrument angular changes and changes to patient anatomical position might not be detected for reasons described above. In our study, we avoided issues of skiving by utilising the navigated high-speed drill (Medtronics) through the robotic arm. Drilling of the pilot hole was gently performed with minimal force while maintaining a constant in-line trajectory.
Skiving was also noted in one of our excluded cases which was attempted through a midline open incision with robotic arm assistance. The surrounding soft tissue envelope and erector spinae muscles had pushed the robot arm medially by a few millimetres (Figure 4), resulting in the navigated drill tip skiving medially. This case was then converted to conventional O-arm navigated MIS-TLIF with free hand screw insertion, where the navigation was corrected. The failure of the robot arm in this case was due to its rigidity which does not correct its position for external deviating forces.

Several morphological studies have also reported statistically smaller lumbar pedicle dimensions in Asian populations compared to Western counterparts, particularly in females (12-16). This places higher requirement for fine-cut CT scans used for navigation, and increases the margin of error to cause screw penetration of the pedicle with every degree of translation or angulation (17). This problem is also accentuated if there is movement of the patient’s anatomy, independent of the navigation reference points as described above.
In two cases not included in this study, there was a software error during the 3-define infrared scan, which was then unable to procced further. The operating team then had to switch the instruments to the conventional O-arm navigation platform (18). This highlights the importance of performing routine pre-operative system checks and having standby equipment and spare instrument sets in the event of system failure.
This pilot prospective case series describes our institution’s experience with RA-TLIF and describe the technical limitations with the Mazor™ X Stealth system (Table 4). The learning curve required to transition from computer O-arm-navigated techniques is well-documented despite sharing the same principles, skill sets, and anatomical landmarks (19). In our RA-TLIF cohort with each successive case (Figure 5), there is an observable trend, of decreasing and plateauing of operation duration after case #7 with exclusion of outlier cases #12, #20, #25 albeit not significant due to small sample size.

The true challenge lies in identifying troubleshooting software and navigation errors, to which the authors recommend performing verification of the navigation system’s accuracy rigorously after image acquisition and auto-registration using a bony landmark (20), such as a spinous process, which might involve a separate incision. Another difficulty will be the initial robotic arm set-up and familiarity of theatre staff to the equipment, which involves many steps and potential for systematic errors. Thus, it will be prudent to have separate instrument sets ready in the event of system failure.
Studies involving robot-assisted interbody fusion is limited (21-23), and in none of them was the robotic arm navigation was involved in the planning and placement of the intervertebral cage. In our workflow, the current software has incorporated planning for interbody cage sizing, but it is unable to fully assist with decompressions and interbody carpentry. Nonetheless, one can also argue that the robot-arm guidance could provide stability during insertion to prevent implant rotation and endplate injury.
Ultimately, the clinical safety and cost-effectiveness of robot-assisted systems has still yet to be proven over conventional computer O-arm navigation, which will be a key consideration in resource-limited public healthcare setting. While multiple studies have shown higher screw accuracy with robot-assisted surgeries (24,25) with similar complication rates, data on overall patient outcome measures are limited. The learning curve required for surgeons to avoid potential pitfalls may pose a risk for complications which, coupled with increased steps for set-up and registration, will inevitably lead to longer operative times. Larger sample size comparative studies will be required to achieve greater statistical significance, with emphasis on patient outcomes to warrant its high acquisition and maintenance costs.
Conclusions
Our single-institution pilot study is first to describe a surgical workflow utilising the Mazor™ X Stealth Edition robotic arm navigation for the planning and insertion of the interbody cage. Our case series has also shown high pedicle screw insertion accuracy and relatively low complication rates, comparable to that of conventional O-arm navigation system. However, the discerning surgeon should be on the ever lookout for potential system-related pitfalls, as well as understand the limitations in the planning software when planning interbody cage fusions. Further studies will also be required on patient outcomes and cost-effectiveness prior to consideration for wide scale implementation.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-24-70/rc
Data Sharing Statement: Available at https://jss.amegroups.com/article/view/10.21037/jss-24-70/dss
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-24-70/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-24-70/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical approval was obtained from the Singhealth Centralised Institutional Review Board (No. 2023-2505). Informed consent from participating patients was not required as no patient identifiable data was used in this study per the terms of the Ethical Board approval.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zhao FD, Yang W, Shan Z, et al. Cage migration after transforaminal lumbar interbody fusion and factors related to it. Orthop Surg 2012;4:227-32. [Crossref] [PubMed]
- Lee NJ, Zuckerman SL, Buchanan IA, et al. Is there a difference between navigated and non-navigated robot cohorts in robot-assisted spine surgery? A multicenter, propensity-matched analysis of 2,800 screws and 372 patients. Spine J 2021;21:1504-12. [Crossref] [PubMed]
- Le X, Tian W, Shi Z, et al. Robot-Assisted Versus Fluoroscopy-Assisted Cortical Bone Trajectory Screw Instrumentation in Lumbar Spinal Surgery: A Matched-Cohort Comparison. World Neurosurg 2018;120:e745-51. [Crossref] [PubMed]
- Buza JA 3rd, Good CR, Lehman RA Jr, et al. Robotic-assisted cortical bone trajectory (CBT) screws using the Mazor X Stealth Edition (MXSE) system: workflow and technical tips for safe and efficient use. J Robot Surg 2021;15:13-23. [Crossref] [PubMed]
- Cui GY, Han XG, Wei Y, et al. Robot-Assisted Minimally Invasive Transforaminal Lumbar Interbody Fusion in the Treatment of Lumbar Spondylolisthesis. Orthop Surg 2021;13:1960-8. [Crossref] [PubMed]
- D'Souza M, Gendreau J, Feng A, et al. Robotic-Assisted Spine Surgery: History, Efficacy, Cost, And Future Trends. Robot Surg 2019;6:9-23. [Crossref] [PubMed]
- Liounakos JI, Khan A, Eliahu K, et al. Ninety-day complication, revision, and readmission rates for current-generation robot-assisted thoracolumbar spinal fusion surgery: results of a multicenter case series. J Neurosurg Spine 2022;36:841-8. [Crossref] [PubMed]
- Gao S, Wei J, Li W, et al. Accuracy of Robot-Assisted Percutaneous Pedicle Screw Placement under Regional Anesthesia: A Retrospective Cohort Study. Pain Res Manag 2021;2021:6894001. [Crossref] [PubMed]
- Tan L, Wen B, Guo Z, et al. Robot-assisted percutaneous vertebroplasty for osteoporotic vertebral compression fractures: a retrospective matched-cohort study. Int Orthop 2023;47:595-604. [Crossref] [PubMed]
- Scheufler KM, Zentner J. Total intravenous anesthesia for intraoperative monitoring of the motor pathways: an integral view combining clinical and experimental data. J Neurosurg 2002;96:571-9. [Crossref] [PubMed]
- Jo JY, Jung KW, Kim HJ, et al. Effect of Total Intravenous Anesthesia vs Volatile Induction With Maintenance Anesthesia on Emergence Agitation After Nasal Surgery: A Randomized Clinical Trial. JAMA Otolaryngol Head Neck Surg 2019;145:117-23. [Crossref] [PubMed]
- Fan Y, Du JP, Liu JJ, et al. Accuracy of pedicle screw placement comparing robot-assisted technology and the free-hand with fluoroscopy-guided method in spine surgery: An updated meta-analysis. Medicine (Baltimore) 2018;97:e10970. [Crossref] [PubMed]
- Hou S, Hu R, Shi Y. Pedicle morphology of the lower thoracic and lumbar spine in a Chinese population. Spine (Phila Pa 1976) 1993;18:1850-5. [Crossref] [PubMed]
- Verma V, Agrawal U Sr. Lumbar Pedicle Morphometry of Dry Vertebral Columns in Relation to Transpedicular Fixation: A Cross-Sectional Study From Central India. Cureus 2023;15:e38108. [Crossref] [PubMed]
- Kim NH, Lee HM, Chung IH, et al. Morphometric study of the pedicles of thoracic and lumbar vertebrae in Koreans. Spine (Phila Pa 1976) 1994;19:1390-4. [Crossref] [PubMed]
- Morita K, Ohashi H, Kawamura D, et al. Thoracic and lumbar spine pedicle morphology in Japanese patients. Surg Radiol Anat 2021;43:833-42. [Crossref] [PubMed]
- Soh TLT, Kho KC, Lim ZK, et al. Morphological Parameters of the Thoracic Pedicle in an Asian Population: A Magnetic Resonance Imaging-Based Study of 3324 Pedicles. Global Spine J 2021;11:437-41. [Crossref] [PubMed]
- O'Connor TE, O'Hehir MM, Khan A, et al. Mazor X Stealth Robotic Technology: A Technical Note. World Neurosurg 2021;145:435-42. [Crossref] [PubMed]
- Hu X, Lieberman IH. What is the learning curve for robotic-assisted pedicle screw placement in spine surgery? Clin Orthop Relat Res 2014;472:1839-44. [Crossref] [PubMed]
- Ling JM, Dinesh SK, Pang BC, et al. Routine spinal navigation for thoraco-lumbar pedicle screw insertion using the O-arm three-dimensional imaging system improves placement accuracy. J Clin Neurosci 2014;21:493-8. [Crossref] [PubMed]
- Beutler WJ, Peppelman WC Jr, DiMarco LA. The da Vinci robotic surgical assisted anterior lumbar interbody fusion: technical development and case report. Spine (Phila Pa 1976) 2013;38:356-63. [Crossref] [PubMed]
- Han XG, Tang GQ, Han X, et al. Comparison of Outcomes between Robot-Assisted Minimally Invasive Transforaminal Lumbar Interbody Fusion and Oblique Lumbar Interbody Fusion in Single-Level Lumbar Spondylolisthesis. Orthop Surg 2021;13:2093-101. [Crossref] [PubMed]
- Chen X, Song Q, Wang K, et al. Robot-assisted minimally invasive transforaminal lumbar interbody fusion versus open transforaminal lumbar interbody fusion: a retrospective matched-control analysis for clinical and quality-of-life outcomes. J Comp Eff Res 2021;10:845-56. [Crossref] [PubMed]
- Han X, Tian W, Liu Y, et al. Safety and accuracy of robot-assisted versus fluoroscopy-assisted pedicle screw insertion in thoracolumbar spinal surgery: a prospective randomized controlled trial. J Neurosurg Spine 2019;30:615-22. [Crossref] [PubMed]
- Staartjes VE, Klukowska AM, Schröder ML. Pedicle Screw Revision in Robot-Guided, Navigated, and Freehand Thoracolumbar Instrumentation: A Systematic Review and Meta-Analysis. World Neurosurg 2018;116:433-443.e8. [Crossref] [PubMed]


