
Short-term clinical and radiographic results of expandable cages that expand both height and lordosis for minimally invasive transforaminal lumbar interbody fusion (MIS TLIF)
We are writing in response to the “Letter to the Editor” regarding our article “Expandable cages that expand both height and lordosis provide improved immediate effect on sagittal alignment and short-term clinical outcomes following minimally invasive transforaminal lumbar interbody fusion (MIS TLIF)” (1,2).
We will address the author’s comments in sequence.
- Single surgeon study that limits generalizability: we acknowledge the limitation of generalizability inherent in a single surgeon study. MIS TLIF is widely practiced globally for its effective direct decompression, minimally invasive approach, and manageable learning curve (3,4). Therefore, our findings are likely representative of outcomes observed by other surgeons performing MIS TLIF procedures.
- Timing of postoperative outcome measures: we explicitly indicated in the manuscript, including its title, that our study focuses on the “immediate” postoperative effects on radiologic parameters and short-term clinical outcomes.
- Regarding the statistical methods used: we utilized Student’s t-test to compare means of normally distributed continuous variables, as described in the methods section of our manuscript. This approach was selected based on the nature of our data and is commonly accepted for such analyses.
- Indications of cages: we described that the choice of cage was determined by its availability. We transitioned from using the RISE® cage to the SABLE® cage as it became available. The indications for both cages were the same.
- Fig. 2: we appreciate the identification of an error in Fig. 2, which displayed only radiographs with no magnetic resonance image (MRI) provided. We have added the figure with the appropriate MRI images in this letter as requested (Figure 1).
- Concern about functional outcomes: our study focused on radiographic parameters and the short-term postoperative period. Oswestry Disability Index (ODI) scores at three months are not predictive of final outcome (5). However, our study revealed significant reductions in both back and leg pain postoperatively reflective of the immediately beneficial effect of nerve root decompression. The point of this study was to describe the radiographic impact of expandable cages. We recognize the need for longer-term studies to comprehensively evaluate sustained functional improvements following MIS TLIF.
- Radiographic measurements: while not radiologists, we confirm that measurements were conducted by two research fellows following study protocols, ensuring consistent and reliable data collection throughout the study. However, given the distinct shapes of the cages visible in X-rays, blinding of assessors for the cage types was not feasible.
- Testing differences between postoperative measurement in Tab. 2: regarding the concern about Tab. 2, we have incorporated mean differences and utilized a linear regression model to analyse the treatment group effects on each radiographic outcome, adjusting for baseline values. This approach ensures that the reported differences in postoperative measurements are accurately attributed to the treatment groups, thereby improving the scientific validity of the findings (6) (Table 1).
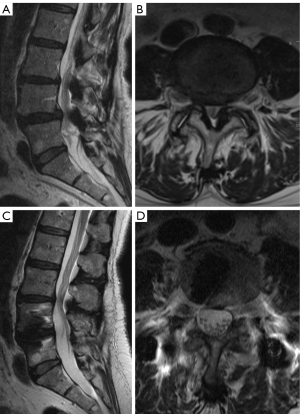
Table 1
| Radiologic measurement | Types of expandable cages | Mean difference (95% CI) | P value | |
|---|---|---|---|---|
| Group H (n=40) | Group HL (n=109) | |||
| Anterior DH (mm) | 1.16 (0.25, 2.06) | 0.01 | ||
| Baseline | 9.4±3.5 | 9.2±4.0 | ||
| Postoperative | 12.6±2.8 | 13.7±3.1 | ||
| Changes (increase) | 3.3±3.8 | 4.5±3.1 | ||
| Posterior DH (mm) | −0.76 (−1.57, 0.05) | 0.06 | ||
| Baseline | 5.0±2.7 | 4.9±2.0 | ||
| Postoperative | 8.7±2.2 | 7.9±2.4 | ||
| Changes (increase) | 3.7±2.8 | 3.0±2.6 | ||
| FH (mm) | −0.15 (−0.75, 0.45) | 0.62 | ||
| Baseline | 15.8±3.3 | 15.6±2.2 | ||
| Postoperative | 18.2±3.4 | 17.9±1.9 | ||
| Changes (increase) | 2.3±1.7 | 2.1±1.8 | ||
| Lumbar lordosis (°) | 1.81 (0.10, 3.51) | 0.04 | ||
| Baseline | 46.5±13.3 | 44.3±13.5 | ||
| Postoperative | 46.9±11.7 | 46.5±13.3 | ||
| Changes (increase) | 0.4±5.7 | 2.5±4.8 | ||
| Segmental lordosis (°) | 2.12 (0.81, 3.43) | 0.002 | ||
| Baseline | 18.0±8.0 | 16.4±6.8 | ||
| Postoperative | 19.7±6.0 | 20.8±6.8 | ||
| Changes (increase) | 2.1±4.8 | 4.4±3.5 | ||
| Disc angle (°) | 3.95 (2.70, 5.21) | <0.001 | ||
| Baseline | 5.9±4.2 | 5.5±4.5 | ||
| Postoperative | 8.1±3.8 | 11.8±4.5 | ||
| Changes (increase) | 2.2±4.3 | 6.3±3.8 | ||
Data are presented as mean ± SD. MIS TLIF, minimally invasive transforaminal lumbar interbody fusion; Group H, expandable cages with only height expansion; Group HL, expandable cages with lordosis and height expansion; CI, confidence interval; DH, disc height; FH, foraminal height; SD, standard deviation.
We agree with the author’s emphasis on transparency regarding potential conflicts of interests and we take his concerns very seriously. The payment mentioned can be found on the “openpayments” website and was made by Globus to the senior author in 2022 for 1,000 USD. This was for his role as a moderator at the Global Spine Congress in Las Vegas:
Next generation of MIS surgery: advantages and challenges over traditional MIS
Date: Friday, June 3, 2022: 11:30 am – 12:30 pm
Moderator:
Roger Härtl, MD
The instructions from the “Journal of Spine Surgery” regarding disclosure of conflict are as follows: “In the interest of transparency, we ask you to disclose all relationships/activities/interests listed below that are related to the content of your manuscript. ‘Related’ means any relation with for-profit or not-for-profit third parties whose interests may be affected by the content of the manuscript. Disclosure represents a commitment to transparency and does not necessarily indicate a bias. If you are in doubt about whether to list a relationship/activity/interest, it is preferable that you do so.”
We did not believe that the payment received for the role as a moderator would qualify as a conflict of interest for this study as it was completely unrelated to the manuscript. We are certainly willing to addend the manuscript and add this as a conflict if the editor recommends this action. We affirm that our study received no specific funding or support from any entity related to the design or conduct of the research. Our primary objective was to objectively compare the performance of different types of expandable cages used in MIS TLIF procedures, without bias towards any specific manufacturer.
Finally, we note that Dr. Pravesh S. Gadjradj lists his affiliation and address for correspondence as the Department of Neurological Surgery at Weill Cornell Medicine in New York. This is not accurate. At the time when this letter was submitted, he had no affiliation with us. We request that this should be corrected.
In conclusion, we want to emphasize that our study is free of any conflict of interest, and we remain committed to upholding the highest standards of transparency, accuracy, and scientific rigor in our research endeavors. We sincerely appreciate the interest and constructive feedback provided by the author and have addressed each concern raised.
Acknowledgments
We extend our sincere gratitude to Dr. Chavithorn Ongkanchana and the Department of Medical Research and Education, Queen Savang Vadhana Memorial Hospital, Chonburi, Thailand, for their invaluable assistance and contributions to the statistical analysis.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Journal of Spine Surgery. The article did not undergo external peer review.
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-24-102/coif). R.H. reports receiving a payment from Globus for a presentation in 2022. The other authors have no conflicts of interest to disclose.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Jitpakdee K, Sommer F, Gouveia E, et al. Expandable cages that expand both height and lordosis provide improved immediate effect on sagittal alignment and short-term clinical outcomes following minimally invasive transforaminal lumbar interbody fusion (MIS TLIF). J Spine Surg 2024;10:55-67. [Crossref] [PubMed]
- Gadjradj PS. Conducting reliable research: transparency, integrity and disclosing conflicts of interest. J Spine Surg 2024;10:327-8. [Crossref] [PubMed]
- Sharif S, Afsar A. Learning Curve and Minimally Invasive Spine Surgery. World Neurosurg 2018;119:472-8. [Crossref] [PubMed]
- Shuman WH, Baron RB, Neifert SN, et al. MIS-TLIF Procedure is Improving With Experience: Systematic Review of the Learning Curve Over the Last Decade. Clin Spine Surg 2022;35:376-82. [Crossref] [PubMed]
- Asher AL, Chotai S, Devin CJ, et al. Inadequacy of 3-month Oswestry Disability Index outcome for assessing individual longer-term patient experience after lumbar spine surgery. J Neurosurg Spine 2016;25:170-80. Erratum in: J Neurosurg Spine 2016;25:279. [Crossref] [PubMed]
- Vickers AJ, Altman DG. Statistics notes: Analysing controlled trials with baseline and follow up measurements. BMJ 2001;323:1123-4. [Crossref] [PubMed]


