
The impact of patient-specific spine rods on spinopelvic parameters after short segment degenerative lumbar fusions
Highlight box
Key findings
• Planning and patient-specific spine rods (PSSRs) significantly improved pelvic incidence to lumbar lordosis (PI-LL) alignment in degenerative lumbar fusion surgery.
• Seventy-four percent of patients maintained spinopelvic alignment (preserved category), and 18% achieved improved alignment (restored category) post-operatively with PSSRs.
• Planning and PSSRs were associated with fewer cases of worsened alignment compared to conventional rods.
What is known and what is new?
• Previous studies have underscored challenges in achieving and maintaining spinopelvic alignment with conventional rods in degenerative lumbar fusion.
• This study introduces planning and PSSRs in degenerative lumbar fusion, demonstrating their potential to enhance PI-LL alignment and improve surgical outcomes.
What is the implication, and what should we change now?
• Surgeons should consider adopting planning and PSSRs for degenerative lumbar fusion to optimize spinopelvic alignment and potentially improve patient outcomes.
• Further research is needed to validate these findings and explore long-term benefits and risks associated with planning and PSSR implementation.
Introduction
Degenerative lumbar conditions, such as spinal stenosis, degenerative disc disease, facet arthropathy, and spondylolisthesis, are prevalent sources of low back pain, radiculopathy, and claudication (1-5). Despite conservative treatments, lumbar fusion emerges as an effective intervention for managing symptoms and instability associated with degenerative diseases (1,6). However, suboptimal outcomes, characterized by persistent pain or recurrent symptoms due to residual stenosis, adjacent segment degeneration, or post-operative malalignment, remain a concern (7-10).
In recent years, advancements in spinal imaging systems, pre-operative planning software, and a deeper understanding of spinal alignment have underscored the importance of achieving harmonious spinopelvic balance (11-14). Parameters like sagittal vertical axis (SVA), pelvic tilt (PT), and pelvic incidence to lumbar lordosis (PI-LL) mismatch have gained traction for predicting and enhancing outcomes in degenerative lumbar pathologies. PI-LL, particularly, serves as a marker of spinopelvic alignment, with a PI-LL ≤10° indicative of a well-aligned spine (13,15). Yet, while routinely assessed in adult deformity surgery, their significance in short-segment constructs for degenerative spine surgery remains unclear (16,17).
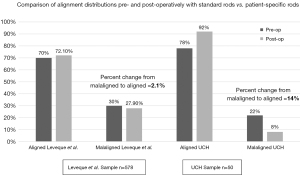
A seminal study by Leveque et al. retrospectively assessed spinopelvic malalignment following short-segment degenerative lumbar fusion procedures (18). Their findings, derived from a multi-institutional cohort of 578 patients at 18 institutions across the United States, underscored the prevalence of malalignment both pre- and post-operatively, with 30% of patients malaligned pre-operatively and 28% malaligned post-operatively. Alignment was preserved in 63%, restored in 9%, and not corrected in 21% of cases. Notably, 7% of patients had a PI-LL ≤±10° prior to surgery but were malaligned in post-operative imaging, placing them in the worsened category. Over 25% of patients were malaligned post-operatively, highlighting the importance of considering spinopelvic alignment in decision-making and operative planning (18).
While the study by Leveque et al. sheds light on the challenges of achieving spinopelvic alignment in short-segment lumbar fusion, it also raises questions about the optimal strategies for addressing these challenges. Conventional spinal rods, while widely used, present several notable limitations in the context of degenerative lumbar fusion. Primarily, these rods are designed with a one-size-fits-all approach, meaning they are pre-curved based on general anatomical averages rather than tailored to individual patient needs. This can result in a mismatch between the rod’s curvature and the patient’s specific spinal alignment, leading to suboptimal correction of deformities and persistent post-operative misalignment. Additionally, the static design of conventional rods does not account for the dynamic changes in spinal alignment that occur as patients heal. As the spine adapts and shifts during the recovery process, conventional rods may not adequately accommodate these changes, potentially resulting in worsening deformity or misalignment over time. Moreover, this mismatch and lack of adaptability can contribute to a higher risk of complications such as rod breakage, screw pull-out, and adjacent segment degeneration.
In response to these limitations, patient-specific spine rods (PSSRs) have been developed to offer a more personalized approach to spinal surgery. By tailoring the rods to the individual’s spinal anatomy and alignment needs, PSSRs aim to enhance the accuracy of deformity correction, improve post-operative alignment stability, and reduce the risk of complications. The customization of these rods promises a more precise fit, better accommodating the dynamic nature of spinal healing and potentially leading to improved clinical outcomes. PSSRs have emerged as a promising intervention for correcting spinal deformities (19,20). These custom rods, tailored to individualized surgical plans and manufactured based on pre-operative spinopelvic parameters, have demonstrated significant improvement in maintaining and improving spinopelvic alignment in adult spinal deformity surgery (19,20). Recent studies have shown that PSSRs can provide excellent correction in adult spinal deformity surgery, with benefits including shorter operating times, fewer mechanical complications such as rod failure, and improved execution of the pre-operative surgical plan, potentially leading to improved spinopelvic alignment and health-related quality of life (HRQOL) scores (13,21).
However, the application of PSSRs in short-segment lumbar fusions for degenerative conditions remains uncertain. This study aims to bridge this gap by comparing radiographic parameters of patients who underwent lumbar fusion using PSSRs for degenerative lumbar conditions to patients who underwent fusion with conventional rods. Leveraging the data from the Leveque et al. study, which predominantly employed standard rods, allows for comparison and assessment of the implications of PSSRs in degenerative lumbar fusion surgery. Through this investigation, we seek to elucidate the potential benefits of PSSRs in optimizing spinopelvic alignment and ultimately improving patient outcomes in this clinical context. We present this article in accordance with the TREND reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-24-75/rc).
Methods
After obtaining institutional review board approval, a retrospective analysis was conducted on patients undergoing short-segment lumbar fusions. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Colorado Multiple Institutional Review Board (COMIRB) (No. 20-2245) and informed consent was obtained from all individual participants. To mitigate potential confounding variables associated with historical controls and variations in surgical techniques, this study focused exclusively on cases performed by the same team of surgeons at our institution. To address potential confounders related to variations in surgical technique and surgeon experience, we adhered to a standardized surgical protocol developed by our institution. By conducting the study at a single institution, we ensured consistent guidelines and practices were followed for all procedures.
The PSSR comparison group comprised surgeries performed by one of three surgeons between September 2016 and August 2018, including either anterior lumbar interbody fusion (ALIF) or transforaminal lumbar interbody fusion (TLIF) combined with posterolateral fusion. The goal of this study was to compare radiographic outcomes of lumbar fusions performed using PSSRs with those reported in historical cohorts, particularly focusing on the differences in spinopelvic alignment. To achieve this, radiographic outcomes were systematically analyzed up to a follow-up period of 2 years.
Follow-up evaluations were scheduled up to 2 years post-operatively. During each follow-up visit, standardized radiographic assessments were conducted to measure key parameters, including PI and LL. The changes in PI-LL mismatch were specifically analyzed to assess the impact of PSSRs on spinopelvic alignment over time. This longitudinal approach aimed to provide a comprehensive evaluation of the effectiveness of PSSRs in maintaining or improving radiographic outcomes compared to historical data.
Inclusion criteria encompassed patients aged 18 years and above who underwent posterior instrumented lumbar fusion involving four levels or fewer with interbody fusion. Patients who underwent posterolateral fusion without interbody support, those with fusions extending into the thoracic spine, or those with fusions spanning more than four levels were excluded. Additionally, patients lacking visible femoral heads on pre-operative imaging were excluded from the analysis.
PI and LL measurements were obtained pre- and post-operatively using imaging software, based on either standing lumbar biplanar films or full body biplanar films. Patients were categorized into four groups (preserved, restored, not corrected, and worsened) based on pre- and post-operative PI-LL measurements. The PSSR cohort was compared to the historical cohort published by Leveque et al., which included 578 patients at 18 institutions across the United States.
Statistical analysis
Statistical analysis was conducted using one-way analysis of variance (ANOVA) tests and one- and two-sample t-tests, performed with R programming language software. P values were calculated using a two-sample t-test for equality of proportions with continuity correction, with significance set at P<0.05.
This approach facilitated a comprehensive comparison of radiographic parameters between patients undergoing lumbar fusion with PSSRs and those with conventional rods, providing valuable insights into the efficacy of PSSRs in optimizing spinopelvic alignment.
Results
Out of sixty patients who underwent lumbar fusion with PSSRs, fifty met the inclusion criteria for analysis. Among them, 37 underwent TLIF with posterolateral instrumented fusion, while 13 underwent ALIF with posterolateral instrumented fusion. Pre-operative measurements for the PSSR cohort indicated an average LL of 49.4°, PI of 58.1°, and PI-LL of 8.6° (Table 1). Post-operatively, the averages were LL of 54.3°, PI of 58.7°, and PI-LL of 4.4°. Statistically significant changes were observed in average LL and average PI-LL from pre- to post-operative time points.
Table 1
| Radiographic parameters | Pre-op (°) | Post-op (°) | Pre- to post-op change | SD of change | P value | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Avg | SD | Range | Avg | SD | Range | |||||
| LL | 49.4 | 14.1 | 21.5 to 79.0 | 54.3 | 11.2 | 28.6 to 73.2 | 4.8 | 8.4 | <0.001 | |
| PI | 58.1 | 11.7 | 37.0 to 93.3 | 58.7 | 11.0 | 41.9 to 88.2 | 0.6 | 3.4 | 0.21 | |
| Spinopelvic alignment (PI-LL) | 8.6 | 11.2 | −15.4 to 43.7 | 4.4 | 8.9 | −11.7 to 23.3 | −4.2 | 8.1 | <0.001 | |
A P value less than 0.05 indicates a significant difference in the pre- to post-operative changes for LL (P≤0.001) and PI-LL (P≤0.001), while the change in PI was not statistically significant (P=0.21). PSSR, patient-specific spine rod; LL, lumbar lordosis; PI, pelvic incidence; PI-LL, pelvic incidence to lumbar lordosis; pre-op, before surgery; post-op, after surgery; Avg, average; SD, standard deviation.
Comparison of pre-operative parameters between the PSSR cohort and the historical cohort from Leveque et al. revealed significant differences, indicating a baseline distinction between the two groups (Table 2). Notably, while the pre-operative PI-LL for the PSSR group (8.6°) exceeded the threshold for spinopelvic malalignment, it was significantly higher than the average for the Leveque cohort (3.7°, P=0.005). Moreover, the PI-LL change post-operatively by an average of −4.2° in the PSSR group, compared to minimal change (−0.1°) in the comparison cohort (P=0.001).
Table 2
| Average PI-LL | Leveque et al. (°) | PSSR sample (°) | P value |
|---|---|---|---|
| Average pre-operative PI-LL | 3.7 | 8.6 | 0.005 |
| Average pre- to post- operative change in PI-LL | −0.1 | −4.2 | 0.001 |
PI-LL, pelvic incidence to lumbar lordosis; PSSR, patient-specific spine rod.
Figure 1 illustrates alignment changes in the PSSR cohort, with 74% (37/50) of patients demonstrating preservation of spinopelvic parameters post-operatively. Additionally, nine patients (18%) with pre-operative spinopelvic mismatch experienced restored PI-LL alignment post-operatively. Only four out of fifty patients exhibited spinopelvic mismatch post-operatively, with two each in the worsened and not corrected categories. Thus, 92%, 46 out of 50 patients achieved radiographically appropriate spinopelvic alignment after lumbar fusion with PSSRs.
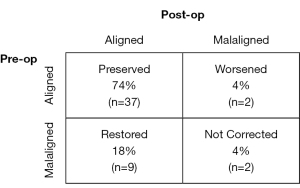
Significant differences were observed in average pre-operative LL and PI-LL among the four categories (Table 3). While post-operative radiographic parameters did not differ significantly between categories, the degree of change from baseline in average LL and PI-LL varied significantly (P<0.001). Categorical distribution analysis between the PSSR and non-PSSR cohorts (Table 4) revealed a higher proportion of preserved parameters (74% vs. 63.5%, P=0.18) and fewer patients with not corrected parameters (4% vs. 21.3%, P<0.01) in the PSSR group. Although not statistically significant, a greater proportion of patients in the PSSR group exhibited restored parameters (18% vs. 8.7%, P=0.05), while fewer were in the worsened category (4% vs. 6.6%, P=0.67).
Table 3
| Parameters | Preserved, n=37 (74%) (°) |
Restored, n=9 (18%) (°) |
Not corrected, n=2 (4%) (°) |
Worsened, n=2 (4%) (°) |
P value |
|---|---|---|---|---|---|
| Preoperative | |||||
| Avg LL | 52.7 | 41.5 | 24.6 | 49.95 | 0.008 |
| Avg PI | 58.3 | 56.8 | 60.3 | 57.1 | 0.98 |
| Avg PI-LL | 5.6 | 15.3 | 35.7 | 7.15 | <0.001 |
| Postoperative | |||||
| Avg LL | 55.0 | 56.0 | 42.8 | 44.25 | 0.25 |
| Avg PI | 59.1 | 57.7 | 57 | 56.9 | 0.98 |
| Avg PI-LL | 4.1 | 1.7 | 14.2 | 12.65 | 0.17 |
| Changes from baseline | |||||
| Avg LL | 2.3 | 14.5 | 18.2 | −5.7 | <0.001 |
| Avg PI | 0.8 | 0.9 | −3.3 | −0.2 | 0.41 |
| Avg PI-LL | −1.5 | −13.6 | −21.5 | 5.5 | <0.001 |
PSSR, patient-specific spine rod; Avg, average; LL, lumbar lordosis; PI, pelvic incidence; PI-LL, pelvic incidence to lumbar lordosis.
Table 4
| Category of patients | Leveque et al. (%) | PSSR (%) | P value |
|---|---|---|---|
| Preserved group | 63.5 | 74.0 | 0.18 |
| Restored group | 8.7 | 18.0 | 0.05 |
| Not corrected group | 21.3 | 4.0 | <0.01 |
| Worsened group | 6.6 | 4.0 | 0.67 |
PSSR, patient-specific spine rod.
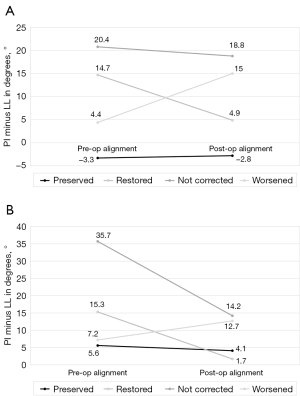
Figure 2 illustrates post-operative alignment changes between the two cohorts, showing a trend towards improved alignment with steeper downward sloping lines indicating greater correction. Despite not meeting the technical definition for acceptable alignment, patients in the custom rod cohort exhibited substantial improvement in spinopelvic alignment. Overall, the proportion of malaligned patients pre-operatively decreased from 22% to 8% in the PSSR cohort, compared to a change of 30% to 27.9% in the Leveque cohort (Figure 3).
Discussion
Following lumbar fusion surgery, residual pain or future disability remains a concern for many patients (7). This can be attributed to factors such as adjacent segment degeneration, occurring in 31% to 83% of cases post-lumbar arthrodesis, and iatrogenic flatback resulting from inadequate lordosis, leading to pain, disability, and sagittal balance issues (8,17,22,23).
This analysis aimed to assess the impact of PSSRs on radiographic parameters following lumbar fusion for degenerative conditions. Leveraging the multicenter retrospective study conducted by Leveque et al., we compared our patient cohort to their historical cohort (18). Our findings revealed a significant difference in the average pre- and post-operative PI-LL (P≤0.001) with the use of PSSRs. Notably, while Leveque et al. reported a lack of statistically significant difference in PI-LL from pre- to post-operative stages (P=0.79), our results suggest the beneficial impact of custom rods on post-operative spinopelvic parameters, with a substantial reduction in PI-LL discrepancy.
However, it is important to acknowledge the limitations inherent in this comparison. One notable limitation is the inability to perform a propensity score matching analysis between our cohort and the historical cohort from Leveque et al., as we did not have access to individual patient data from their study. This lack of direct data access prevented us from matching patients based on baseline characteristics, such as preoperative PI-LL, which could influence the outcomes. Consequently, baseline differences between the cohorts may affect the comparability of our results. The cohort from Leveque et al. [2018] included patients without well-defined exclusion criteria such as prior spinal fusions or the severity of preoperative deformities. This lack of stringent criteria could result in differences in baseline patient characteristics between their cohort and our PSSR cohort, potentially impacting the comparability of outcomes. For instance, patients in the Leveque et al. cohort may have had more severe preoperative conditions or prior spinal interventions, which were not accounted for in their study but were rigorously considered in our patient selection.
These discrepancies in patient selection criteria may introduce variability in the outcomes, affecting the interpretation of our results. To address this, future studies should aim to include more detailed patient selection criteria and consider using propensity score matching or other statistical techniques to control for baseline differences when comparing outcomes between different cohorts. This would help in reducing potential biases and improving the robustness of comparisons across studies.
Examining general outcomes, we observed an overall improvement in alignment with the use of PSSRs. A greater proportion of patients in the preserved and restored categories and fewer in the not corrected and worsened categories demonstrated improved alignment post-operatively. Specifically, 74% of patients in our PSSR cohort fell into the preserved category, indicating maintenance of spinopelvic alignment, while 18% were restored to appropriate alignment. In contrast, only 4% of patients were categorized as not corrected, suggesting minimal post-operative misalignment, and 4% were classified as worsened, indicating a slight deterioration in alignment. This suggests that PSSRs may offer better maintenance or correction of spinopelvic alignment compared to conventional rods.
Only two of our patients went from the aligned to the malaligned category with the use of PSSRs, placing them in the “worsened” category. The first of these cases was a patient who underwent a three-level ALIF with interbody fusions and instrumented posterior spinal fusion from L3–S1. Pre-operatively, LL was −48.4°, sacral slope (SS) was 27°, PT was 26.9°, and PI was 53.9°. Post-operatively, LL was −43.1°, SS was 29.9°, PT was 24.1°, and PI was 54°. This resulted in a pre-operative PI-LL mismatch of 5.5° and a post-operative PI-LL of 10.9°, exceeding the threshold of 10° used to define malalignment and technically placing this patient in the “worsened” category. In the second case, a patient underwent two-level ALIF and instrumented posterior spinal fusion from L4 to S1. The pre-operative LL was −50.5°, SS was 35.5°, PT was 11.1°, and PI was 46.6°. Post-operatively, LL was −56.1°, SS was 34.2°, PT was 11.5°, and PI was 45.7°. This resulted in a pre-operative PI-LL of −3.9°, which post-operatively worsened to −10.4°, crossing the malalignment threshold by just 0.4°. While the clinical relevance of values so close to the threshold of 10° can be debated, they technically place patients in the “malaligned” category even with use of a PSSR. This suggests that even with advanced PSSR technology, their use does not guarantee appropriate correction in alignment.
Even patients categorized as not corrected showed substantial improvement in pre- to post-operative PI-LL parameters. Despite residual PI-LL exceeding 10°, these patients exhibited significant improvement compared to the non-custom rod cohort, with an average improvement of over 20° compared to only 2° in the non-custom rod cohort. Furthermore, patients categorized as worsened in the Leveque cohort experienced nearly double the increase in PI-LL compared to those in the custom rod cohort.
While the radiographic improvements observed with PSSRs are promising, their clinical significance must be considered. Improved PI-LL alignment can lead to better distribution of spinal loads and reduce the risk of adjacent segment degeneration, a common complication in lumbar fusion surgeries. Additionally, effective sagittal alignment correction is associated with reductions in back pain and disability. Studies have shown that optimal alignment correlates with better HRQOL scores, indicating improved patient outcomes (13,21). Although our study primarily focuses on radiographic changes, future research should integrate patient-reported outcomes to fully understand how these improvements translate into clinical benefits.
Our study included lumbar fusions performed via ALIF and TLIF, with no significant differences in radiographic parameters were noted between the two procedures (24). This suggests that both techniques can effectively contribute to spinopelvic alignment improvement.
This study represents the first analysis, to our knowledge, of the use of custom PSSRs for degenerative lumbar fusions. Despite promising results, additional limitations warrant consideration. We were constrained by the retrospective nature of the study, necessitating comparison with a historical cohort, which may introduce biases. However, it’s noteworthy that this historical cohort spanned 18 institutions with over 500 patients, potentially accounting for variances in surgical preferences, technologies, and techniques across the country. Furthermore, our study did not evaluate global spinopelvic alignment parameters, specific patient-reported outcomes, or complication rates. Despite these limitations, our findings provide valuable insights into the potential of custom spine rods to enhance spinopelvic alignment and patient outcomes, laying the groundwork for future research in this area.
Conclusions
In summary, our study emphasizes the significant impact of PSSRs in enhancing spinopelvic parameters in short segment lumbar fusions for degenerative conditions. Patients who underwent fusion with PSSRs experienced a notable improvement in PI-LL and demonstrated a heightened capacity to achieve pre-operative alignment objectives. These findings highlight the efficacy of custom rods in facilitating the restoration or preservation of spinopelvic alignment during lumbar fusion procedures. Considering these results, the integration of PSSRs should be carefully considered to optimize surgical outcomes and enhance patient care in this context.
Acknowledgments
Special thanks to Christina Khat, BS, from School of Medicine, University of Colorado Orthopedics, Aurora, CO for her assistance in manuscript preparation and submission.
Footnote
Reporting Checklist: The authors have completed the TREND reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-24-75/rc
Data Sharing Statement: Available at https://jss.amegroups.com/article/view/10.21037/jss-24-75/dss
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-24-75/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-24-75/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Colorado Multiple Institutional Review Board (COMIRB) (No. 20-2245) and informed consent was obtained from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bae HW, Rajaee SS, Kanim LE. Nationwide trends in the surgical management of lumbar spinal stenosis. Spine (Phila Pa 1976) 2013;38:916-26. [Crossref] [PubMed]
- Bederman SS, Kreder HJ, Weller I, et al. The who, what and when of surgery for the degenerative lumbar spine: a population-based study of surgeon factors, surgical procedures, recent trends and reoperation rates. Can J Surg 2009;52:283-90. [PubMed]
- Makanji H, Schoenfeld AJ, Bhalla A, et al. Critical analysis of trends in lumbar fusion for degenerative disorders revisited: influence of technique on fusion rate and clinical outcomes. Eur Spine J 2018;27:1868-76. [Crossref] [PubMed]
- Martin BI, Mirza SK, Spina N, et al. Trends in Lumbar Fusion Procedure Rates and Associated Hospital Costs for Degenerative Spinal Diseases in the United States, 2004 to 2015. Spine (Phila Pa 1976) 2019;44:369-76. [Crossref] [PubMed]
- Rajaee SS, Bae HW, Kanim LE, et al. Spinal fusion in the United States: analysis of trends from 1998 to 2008. Spine (Phila Pa 1976) 2012;37:67-76. [Crossref] [PubMed]
- Yavin D, Casha S, Wiebe S, et al. Lumbar Fusion for Degenerative Disease: A Systematic Review and Meta-Analysis. Neurosurgery 2017;80:701-15. [Crossref] [PubMed]
- Koenders N, Rushton A, Verra ML, et al. Pain and disability after first-time spinal fusion for lumbar degenerative disorders: a systematic review and meta-analysis. Eur Spine J 2019;28:696-709. [Crossref] [PubMed]
- Maruenda JI, Barrios C, Garibo F, et al. Adjacent segment degeneration and revision surgery after circumferential lumbar fusion: outcomes throughout 15 years of follow-up. Eur Spine J 2016;25:1550-7. [Crossref] [PubMed]
- Potter BK, Lenke LG, Kuklo TR. Prevention and management of iatrogenic flatback deformity. J Bone Joint Surg Am 2004;86:1793-808. [Crossref] [PubMed]
- Le Huec JC, Faundez A, Dominguez D, et al. Evidence showing the relationship between sagittal balance and clinical outcomes in surgical treatment of degenerative spinal diseases: a literature review. Int Orthop 2015;39:87-95. [Crossref] [PubMed]
- Glassman SD, Berven S, Bridwell K, et al. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 2005;30:682-8. [Crossref] [PubMed]
- Johnson RD, Valore A, Villaminar A, et al. Sagittal balance and pelvic parameters--a paradigm shift in spinal surgery. J Clin Neurosci 2013;20:191-6. [Crossref] [PubMed]
- Schwab FJ, Blondel B, Bess S, et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976) 2013;38:E803-12. [Crossref] [PubMed]
- Le Huec JC, Charosky S, Barrey C, et al. Sagittal imbalance cascade for simple degenerative spine and consequences: algorithm of decision for appropriate treatment. Eur Spine J 2011;20:699-703. [Crossref] [PubMed]
- Aoki Y, Nakajima A, Takahashi H, et al. Influence of pelvic incidence-lumbar lordosis mismatch on surgical outcomes of short-segment transforaminal lumbar interbody fusion. BMC Musculoskelet Disord 2015;16:213. [Crossref] [PubMed]
- Roussouly P, Gollogly S, Berthonnaud E, et al. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976) 2005;30:346-53. [Crossref] [PubMed]
- Jang JS, Lee SH, Min JH, et al. Changes in sagittal alignment after restoration of lower lumbar lordosis in patients with degenerative flat back syndrome. J Neurosurg Spine 2007;7:387-92. [Crossref] [PubMed]
- Leveque JA, Segebarth B, Schroerlucke SR, et al. A Multicenter Radiographic Evaluation of the Rates of Preoperative and Postoperative Malalignment in Degenerative Spinal Fusions. Spine (Phila Pa 1976) 2018;43:E782-9. [Crossref] [PubMed]
- Barton C, Noshchenko A, Patel V, et al. Early Experience and Initial Outcomes With Patient-Specific Spine Rods for Adult Spinal Deformity. Orthopedics 2016;39:79-86. [Crossref] [PubMed]
- Kleck CJ, Calabrese D, Reeves BJ, et al. Long-Term Treatment Effect and Predictability of Spinopelvic Alignment After Surgical Correction of Adult Spine Deformity With Patient-Specific Spine Rods. Spine (Phila Pa 1976) 2020;45:E387-96. [Crossref] [PubMed]
- Solla F, Barrey CY, Burger E, et al. Patient-specific Rods for Surgical Correction of Sagittal Imbalance in Adults: Technical Aspects and Preliminary Results. Clin Spine Surg 2019;32:80-6. [Crossref] [PubMed]
- Rothenfluh DA, Mueller DA, Rothenfluh E, et al. Pelvic incidence-lumbar lordosis mismatch predisposes to adjacent segment disease after lumbar spinal fusion. Eur Spine J 2015;24:1251-8. [Crossref] [PubMed]
- Vazifehdan F, Karantzoulis VG, Igoumenou VG. Sagittal alignment assessment after short-segment lumbar fusion for degenerative disc disease. Int Orthop 2019;43:891-8. [Crossref] [PubMed]
- Mobbs RJ, Phan K, Malham G, et al. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg 2015;1:2-18. [PubMed]


